Sepsis can cause both brain dysfunction and neuroinflammation. New research from the University of Michigan indicates that gut bacteria play a role in brain dysfunction after sepsis. Researchers explain that sepsis causes gut bacteria to locate in the brain for several days and ultimately resolves in the weeks after the onset of illness. The findings, published in the American Journal of Respiratory and Critical Care Medicine, suggest that treating gut bacteria could help avoid or reduce brain dysfunction in sepsis survivors.
Previous studies have suggested that gut microbes, or microbiome, may increase the likelihood of lung inflammation during sepsis. However, little is known about the microbiome's effect on other organs, such as the brain. U-M researchers hypothesised that the brain injury in sepsis is directly related to gut bacteria independently moving to the brain, triggering an immune response that leads to longer-term effects from the injury.
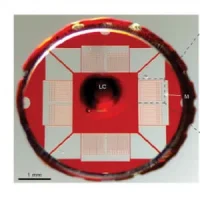
The researchers used mice models and brain tissue of deceased patients (the latter source came from the University of Michigan Brain Bank) to carry out the study. Mice that survived sepsis were compared with mice controls; brain tissue of patients who died of sepsis was compared with tissue of patients who died of noninfectious causes. In addition, the researchers used 16S rRNA gene sequencing, a technique that identifies bacteria present in a sample via their DNA signature, in the mice models and human tissues to identify which gut bacteria fuelled their hypothesis.
The U-M team found that gut bacteria present in the brains of the mice five days after surviving sepsis – but gone by 14 days after the infection – were associated with levels of S100A8, a marker of neuroinflammation. As was observed in mice, the researchers said, the gut bacteria detected in brains of patients who died of sepsis correlated with the S100A8 inflammation marker.
Benjamin Singer, MD, PhD, an assistant professor of internal medicine at Michigan Medicine and the study's lead author, notes that while the human tissue analysis was a small cohort, the research team noticed distinct differences between patients who died of sepsis and those who died of noninfectious causes.
"Anytime someone dies, bacteria grow out of control because the immune system is not keeping the bacteria in the body in check," Dr. Singer said. "But we found that the bacteria we isolated from patients that died of sepsis were quite different from the run-of-the-mill bacteria that sit in the body after a person dies – and did appear to be associated with neuroinflammation in the brain."
Because the gut bacteria were present in the brains of both the mice and humans who died of sepsis – and those bacteria were associated with the marker for inflammation of the brain – the findings indicate gut bacteria do appear to play a role in brain impairment after sepsis.
"The larger question raised by this study is: Is there anything we can do to intervene and change the consequences of critical illness for survivors?" Dr. Singer said. Although additional research would be needed to confirm the study's findings, the doctor is of the opinion that giving patients oral antibiotics to remove those bacteria in the gut may potentially reduce long-term effects of critical illness.
Source: Michigan Medicine - University of Michigan
Image Credit: Pixabay
References:
Singer BH et al. (2017) Bacterial Dissemination to the Brain in Sepsis. Am. J. Respir. Crit. Care Med. Online: December 12, 2017. https://doi.org/10.1164/rccm.201708-1559OC
Latest Articles
Sepsis, brain dysfunction, gut bacteria, Brain impairment, neuroinflammation
Sepsis can cause both brain dysfunction and neuroinflammation. New research from the University of Michigan indicates that gut bacteria play a role in brain dysfunction after sepsis.