ICU Management & Practice, Volume 22 - Issue 3, 2022
Introduction
Early mobilisation (EM) is a therapeutic strategy implemented to avoid and overcome impairments developed due to critical illness and ICU stay. Several benefits have been described throughout the literature such as overcoming ICU acquired weakness, reduction in days of mechanical ventilation and stay, greater functionality inside the ICU, higher levels of independence, and lower health care costs, among others. The main objective of this article is to highlight the most common mistakes in decision making and the practice of EM.
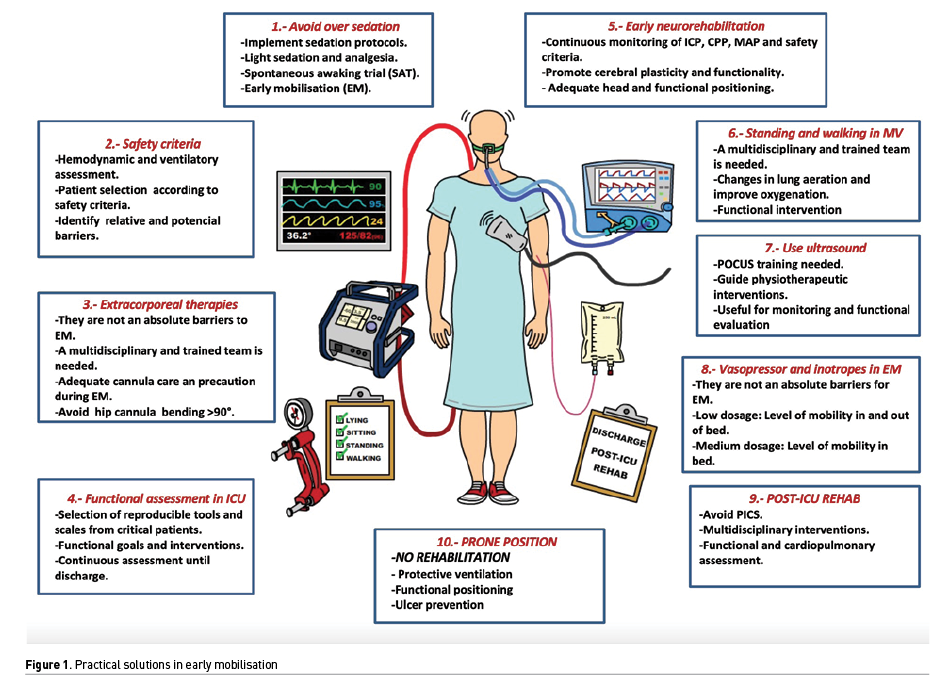
Here are ten overlooked mistakes during early mobilisation in the ICU:
1. Unnecessary, profound and prolonged sedation
Patients undergoing critical illness that require mechanical ventilation or any other invasive procedure require sedatives and analgesic medication. Such pharmacological agents intend to provide comfort, stability and pain management during their stay in the ICU (Reade et al. 2014). Although indications for profound sedation have been precisely listed, numerous patients will still undergo deep sedation without such indication (Oyler et al. 2018; Moreira et al. 2016). Apart from the patients in need of deep sedation (RASS -4/-5), patients should be awake, alert and cooperative (RASS 0/-1) to ensure all the benefits described in the ABCDEF bundle (Devlin et al. 2018). EM plays an essential role in this bundle but inadequate sedation levels are to this day one of the most common barriers for such practice. Profound sedation in patients that can be included in an early mobilisation programme can have a negative impact on the functional progression, perpetuate immobility effects and prolong the length of stay inside the ICU (Hodgson et al. 2021).
2. Lack of individualisation in deciding the start of EM
Many EM protocols establish a need of initiating the rehabilitation process in the first 24 hours of stay inside the ICU (Hodgson et al. 2021). This will not be accomplished in all scenarios. The decision of initiating an EM programme must be based on the clinical status, not the time inside the ICU. In some cases, rehabilitation programmes can start in the very early stages of critical illness (Hodgson et al. 2014a), in some other cases, especially in acute respiratory distress syndrome (ARDS), instability in critically ill patients can maintain for even weeks. Nevertheless, in neurocritical patients, the early start of the rehabilitation process does impact the functional outcomes of the patient and is a race against time (Hernández et al. 2021). Decision making inside the ICU is an individual process for every patient and rehabilitation cannot be seen as a strict-time protocol.
3. Immobility during extracorporeal support: ECMO and CRRT
Extracorporeal support (ES) is more and more commonly seen in ICUs these days. Extracorporeal membrane oxygenation (ECMO) and continuous renal replacement therapy (CRRT) are some of the most popular among the utilisation of ES therapies. ECMO configurations are mainly split into two categories: veno-venous (VV) ECMO which provides oxygenation support when conventional treatment fails in severe ARDS and veno-arterial (VA) ECMO that is used in patients who require haemodynamic support due to numerous cardiac centred pathologies (Shekar et al. 2020). Also, CRRT can be seen during ICU stay in patients that have or develop kidney injury. Any of these therapies have to be applied through vascular access catheters or cannulas that can limit mobility in such patients which commonly translates to prolonged immobility due to the fear of catheter removal during mobilisation (Abrams et al. 2022a). Nevertheless, enough documentation on secure practices in such therapies has been available for some years now, especially in well-coordinated and experimented ICU personnel. Hence, it has been described that patients undergoing extracorporeal therapies have a high risk of developing functional deterioration, muscle mass loss and post-intensive care syndrome (PICS) (Hayes et al. 2018). EM must be used as a prevention strategy to avoid these negative outcomes derivative from immobility.
EM is a safe practice in extracorporeal therapies, but special care and knowledge must be taken into consideration before and during mobilisation especially with ECMO cannulas. If femoral access has been established, a hip flexion >90° must be avoided (Raurell et al. 2021), as well as continuous monitorisation in ECMO pressures (mainly the extraction pressure which should be the only negative pressure), precaution with stitches in the cannula attaching it to the patient’s leg and ensuring cannulas are maintained in place. ECMO parameters (FiO2, revolutions or CO2 sweep) may be modified by the perfusion team to provide a safer exercise tolerance, but no clear evidence has been reported for such matter (Mossadegh 2017). Similar to the previous statement, no evidence has been documented in the consideration of patient self-induced lung injury (P-SILI) as a limitation for mobilisation practices. Hence, monitorisation of tidal volume (TV) and respiratory rate (RR) is recommended during exercise intervals, as well as oxygenation and respiratory drive. It’s important to mention that physiological response to exercise should raise these levels as a normal response. Nonetheless, protective ventilation has to be maintained during these intervals. CRRT tends to have fewer complications during mobilisation due to the smaller catheters needed. The correct functioning of the machine should be checked, the pressures being needed, as well as the haemodynamic response to exercise. Extracorporeal therapies are a big challenge for the whole ICU personnel, including rehabilitation, and a meticulous evaluation of clinical stability in patients during such therapies is key for safe exercise practices (Abrams et al. 2022b).
4. Interventions without functional objectives
Throughout critical illness, patients must receive EM. This intervention has to have functional goals and for this matter, the implementation of tools that evaluate the patient’s level of functionality is needed, otherwise poor or no evaluation will result in an inadequate exercise prescription (Parry et al. 2017). Some of the most common and useful tools are the Medical Research Council Sum Score (MRC-SS), handgrip strength through dynamometry (Piva et al. 2019), ICU Mobility Scale (IMS) (Tipping et al. 2016; Hodgson et al. 2014b) and the Chelsea Critical Care Physical Assessment Tool (CPAx) (Corner et al. 2016). The use of such tools will encourage taking patients to their maximum level of functionality and can guide the next steps towards higher functionality levels. Recent studies have correlated the success in the weaning process with greater scores in MRC and handgrip strength. A frequent mistake during EM is underestimating the patient’s capacity to accomplish higher mobility and functional levels. This can perpetuate immobility and waste time with interventions that have no real benefit. For example, why should a physiotherapist decide to move passively (with no effort applied by the patient) the patient’s arms if the patient is capable of doing it themselves? Shouldn’t the patient be encouraged to actively move and develop strength through exercise? Overload and progression of muscle strength are essential pillars of any exercise applied to the human body. Also, a common approach during EM is centred on strengthening peripheral muscles and excluding some essential components of the human body biomechanics: core musculature, antigravitational muscles and proprioception.
5. Delayed rehabilitation in the neurocritical patient
A common neurocritical phrase used among professionals is “brain is time”. In acute brain injuries, we run against time in every aspect, including the rehabilitation process. Brain plasticity in the early stages of such pathologies must be taken as an advantage to promote functionality and avoid the permanent establishment of physical and mental impairments. Better outcomes have been found in patients battling critical illness due to a neurological diagnosis when they start their rehabilitation process in the early stages of the pathology’s course (Olkowski et al. 2017). A particular group of patients among the neurological pathologies are patients with stroke. Large studies have found the need for initiating rehabilitation after 24 hours of symptoms appearing. In some other cases, patience will reward; in patients with an elevation in intracranial pressure (ICP) such as cerebral haemorrhage or traumatic brain injury, physical interventions should wait until surgical or pharmacological interventions have overpowered the bleed or reason for high ICP (Hernandez et al. 2021; Kumar et al. 2020).
Mobilisation in the neurocritical patient is safe and has no impact on the variation of mean arterial pressure (MAP), ICP or cerebral perfusion pressure (CPP) (Zink et al. 2021). Some interventions may even be an alternative for high ICP management such as early verticalisation of patients, which is known to be safe and can be done even while being mechanically ventilated (Lachance et al. 2021). Also, early ambulation is related to a reduction in the risk of vasospasm in subarachnoid haemorrhage. Precaution in head positioning, as well as functional positioning and segment alignments, is a fundamental practice for these patients at any stage of their stay in the ICU.
6. Absence of verticalisation or ambulation during mechanical ventilation
Patients in need of mechanical ventilation must not be condemned to bed rest or low mobility levels during this period. Patients capable of maintaining an upright position and with enough strength (gained or never lost) to stand up should be submitted to training intervals that include verticalisation, standing up, marching in place or ambulation (Raurell et al. 2021). In order to achieve such high levels of mobility in these patients the cooperation of a multidisciplinary team must be established into the routine care (Yang et al. 2021; Miranda et al. 2017). Benefits have been reported in these interventions such as greater lung aeration, easier diaphragmatic pull and neurological stimulation (Hickmann et al. 2021; Hernandez et al. 2021). A simplistic view of the weaning process will avoid professionals to believe that a mechanically ventilated patient can’t walk. To think that weaning is merely a muscular issue and does not involve a whole systemic approach (airway integrity, lung parenchyma, cardiac functionality, neurologic status, electrolytic balance, among others) is an obsolete and easy way of conducting therapeutic decisions towards failure. Nonetheless, an immense mistake would be to delay the extubating procedure once the patient is ready for it. Something important to mention is that weakness among respiratory muscles is more common than peripheral musculature weakness; this also explains the reason for finding patients undergoing severe respiratory muscle weakness being able to walk (Dres et al. 2017).
7. Excluding POCUS
Many pulmonary centred interventions are traditionally guided through auscultation, but this tool has a low sensibility and specificity in the evaluation of such clinical scenarios. Ultrasound evaluation has gained the power to the point it has become the fifth cornerstone of physical exploration (Narula et al. 2018). Physiotherapists and rehabilitation staff have to integrate ultrasound evaluation into their daily basis (Hayward et al. 2018; Hayward et al. 2020; Arnold et al. 2020; Hansell et al. 2021; Vieira et al. 2020). Pulmonary, diagrammatic and muscular ultrasound can guide interventions and decision making in clinical scenarios such as non-invasive mechanical ventilation, utilisation of positive expiratory pressure (PEP) device, inspiratory muscle training (IMT), verticalisation, hyperinflation, lung expansion therapies, among others (Bertolone et al. 2021; Leech et al. 2015). Hence, it is a remarkable tool during the weaning process of mechanical ventilation through diaphragmatic, lung and cardiac evaluation. Muscular evaluation can also be accomplished through echography by measuring muscle thickness and the Heckmatt scale. Finally, some interesting findings can be made during such evaluation, findings that can even put the patient at risk. Pneumothorax, pleural effusions, cardiac tamponade, high ICP and other life-threatening situations have been found during the physiotherapeutic evaluation and these could have gone unnoticed if echography was not available (Ntoumenopoulos et al. 2021; Le Neindre et al. 2016).
8. Vasoactive and inotropic medication as a barrier for early mobility
Some of the everyday pharmacological agents used in the treatment of critical illness are vasoactive and inotropic drugs. These drugs are mainly used for shock treatment and the optimisation of haemodynamics and must not be considered a contraindication for the start of an EM programme but should definitely be a precaution in the decision making of such start (Hodgson et al. 2014a). Secure and feasible practices have been reported during the administration of such drugs, although these practices can only be implemented in patients undergoing moderate to low dosages of these agents. Haemodynamic monitoring before and during the implementation of EM in patients receiving vasoactive and/or inotropic agents is fundamental, not only for the identification of haemodynamic stability but also the cardio-circulatory response to exercise (Jacob et al. 2021).
9. Poor post-ICU follow up
When a patient is discharged from the ICU the main objective should be to reincorporate the patient back into his/her social role. This starts with assuring the patient is able to execute basic life activities such as hygiene care, movement and ambulation, talking, eating, etc. The process of reincorporation will eventually evolve in the need of developing more complex motor and mental skills and will finish with the individual's complete independence (Colbenson et al. 2019). During this process functional, mobility, independence and cardiopulmonary evaluations have to be done and will guide future interventions or discharge from the rehabilitation programme (Inoue et al. 2019). Continuing with rehabilitation after ICU discharge will have a direct impact on the patient’s quality of life and recovery from impairments established due to critical illness. Patient follow-up after ICU discharge is part of the finishing with what started as a critical illness; failing to give a proper follow-up after discharge will only highlight the lack of interest in the patient’s future (Nakanishi et al. 2021; Rousseau et al. 2021).
10. Mobilisation during prone position
The prone position is a widely known strategy in the treatment of ARDS. This strategy is used to optimise mechanical ventilation and improve oxygenation (Guérin et al. 2017; Johnson et al. 2021). Prone positioning translates into severe ARDS, severe oxygenation impairment and is one of the few absolute contraindications of EM (Raurrell et al. 2021; Hodgson et al. 2014a). During this phase, EM or any other physiotherapeutic strategy must be held up, except correct segment alignment, prevention of pressure ulcers and protective ventilation. No evidence has been provided that recommends EM during prone position in severe ARDS.
Conflict of Interest
None.
References:
Abrams D, Madahar P, Eckhardt CM et al. (2022a) Early Mobilization during Extracorporeal Membrane Oxygenation for Cardiopulmonary Failure in Adults: Factors Associated with Intensity of Treatment. Annals of the American Thoracic Society. 19(1):90-98.
Abrams D, Madahar P, Eckhardt CM et al. (2022b). Early mobilization during extracorporeal membrane oxygenation for cardiopulmonary failure in adults: factors associated with intensity of treatment. Ann Am Thorac Soc. 19:90–98.
Arnold MJ, Jonas CE, Carter RE (2020) Point-of-Care Ultrasonography. American family physician. 101(5):275-285.
Bertolone DT, De Colle C, Rozza F et al. (2021) Lung ultrasound: a narrative review and proposed protocol for patients admitted to Cardiac Rehabilitation Unit. Monaldi archives for chest disease = Archivio Monaldi per le malattie del torace, 10.4081/monaldi.2021.1753. Advance online publication.
Colbenson GA, Johnson A, Wilson ME (2019) Post-intensive care syndrome: impact, prevention, and management. Breathe. 15(2):98-101.
Corner EJ, Handy JM, Brett SJ (2016) eLearning to facilitate the education and implementation of the Chelsea Critical Care Physical Assessment: a novel measure of function in critical illness. BMJ open. 6(4):e010614.
Devlin JW, Skrobik Y, Gélinas C et al. (2018) Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU. Critical care medicine. 46(9):e825-e873.
Dres M, Dubé BP, Mayaux J et al. (2017). Coexistence and Impact of Limb Muscle and Diaphragm Weakness at Time of Liberation from Mechanical Ventilation in Medical Intensive Care Unit Patients. American journal of respiratory and critical care medicine. 195(1):57–66.
Guérin C (2017) Prone positioning acute respiratory distress syndrome patients. Ann Transl Med. 5(14):289.
Hansell L, Milross M, Delaney A et al. (2021) Lung ultrasound has greater accuracy than conventional respiratory assessment tools for the diagnosis of pleural effusion, lung consolidation and collapse: a systematic review. Journal of physiotherapy. 67(1):41-48.
Hayes K, Holland AE, Pellegrino VA et al. (2018) Acute skeletal muscle wasting and relation to physical function in patients requiring extracorporeal membrane oxygenation (ECMO). Journal of critical care. 48:1-8.
Hayward SA, Janssen J (2018) Use of thoracic ultrasound by physiotherapists:a scoping review of the literature. Physiotherapy. 104(4):367-375.
Hayward S, Smith M, Innes S (2020) Diagnostic thoracic ultrasound imaging - An exploration of respiratory physiotherapists' interest and use in clinical practice: A national survey. Ultrasound. 28(1):14-22.
Hernandez S, Kittelty K, Hodgson CL (2021) Rehabilitating the neurological patient in the ICU: what is important? Current opinion in critical care. 27(2):120-130.
Hickmann CE, Montecinos-Munoz NR, Castanares-Zapatero D et al. (2021) Acute Effects of Sitting Out of Bed and Exercise on Lung Aeration and Oxygenation in Critically Ill Subjects. Respir Care. 66(2):253-262.
Hodgson CL, Schaller SJ, Nydahl P et al. (2021) Ten strategies to optimize early mobilization and rehabilitation in intensive care. Critical care. 25(1):324.
Hodgson CL, Stiller K, Needham DM et al. (2014a) Expert consensus and recommendations on safety criteria for active mobilization of mechanically ventilated critically ill adults. Critical care. 18(6):658.
Hodgson C, Needham D, Haines K et al. (2014b) Feasibility and inter-rater reliability of the ICU Mobility Scale. Heart & Lung:The Journal of Acute and Critical Care. 43(1):19-24.
Inoue S, Hatakeyama J, Kondo Y et al. (2019) Post-intensive care syndrome: its pathophysiology, prevention, and future directions. Acute medicine & surgery. 6(3):233-246.
Jacob P, Surendran PJ, Aleef EM et al. (2021) Early Mobilization of Patients Receiving Vasoactive Drugs in Critical Care Units: A Systematic Review, Journal of Acute Care Physical Therapy. 12(1):37-48.
Johnson NJ, Luks AM, Glenny RW (2017) Gas Exchange in the Prone Posture. Respiratory care. 62(8):1097-1110.
Kumar MA, Romero FG, Dharaneeswaran K (2020) Early mobilization in neurocritical care patients. Current opinion in critical care. 26(2):147-154.
Lachance BB, Chang W, Motta M et al. (2021) Verticalization for Refractory Intracranial Hypertension: A Case Series. Neurocritical care. 10.1007/s12028-021-01323-z. Advance online publication.
Leech M, Bissett B, Kot M, Ntoumenopoulos G (2015a) Lung ultrasound for critical care physiotherapists:a narrative review. Physiotherapy research international: the journal for researchers and clinicians in physical therapy. 20(2):69-76.
Le Neindre A, Mongodi S, Philippart F, Bouhemad B (2016) Thoracic ultrasound:Potential new tool for physiotherapists in respiratory management. A narrative review. Journal of critical care. 31(1):101-109.
Miranda Rocha AR, Martinez BP, Maldaner da Silva VZ et al. (2017) Early mobilization:Why, what for and how? Medicina intensive. 41(7):429-436.
Moreira FT, Serpa Neto A (2016) Sedation in mechanically ventilated patients-time to stay awake? Annals of translational medicine. 4(19):382.
Mossadegh, C. (2017). Monitoring the ECMO. Nursing Care and ECMO. Springer Link.
Nakanishi N, Liu K, Kawakami D et al. (2021) Post-Intensive Care Syndrome and Its New Challenges in Coronavirus Disease 2019 (COVID-19) Pandemic: A Review of Recent Advances and Perspectives. Journal of clinical medicine. 10(17):3870.
Narula J, Chandrashekhar Y, Braunwald E (2018) Time to Add a Fifth Pillar to Bedside Physical Examination: Inspection, Palpation, Percussion, Auscultation, and Insonation. JAMA cardiology. 3(4):346-350.
Ntoumenopoulos G, Le Neindre A (2021) Intensive Care Physiotherapists Should be Using Point of Care Ultrasound (POCUS). ICU Management & Practice, 21(2):107-111.
Olkowski BF, Shah SO (2017) Early Mobilization in the Neuro-ICU: How Far Can We Go? Neurocritical care. 27(1):141-150.
Oyler DR, Bernard AC (2018) Analgesia, Sedation, and Delirium in the ICU. Surgical Critical Care Therapy. 37-52.
Parry SM, Huang M, Needham DM (2017) Evaluating physical functioning in critical care: considerations for clinical practice and research. Critical care. 21(1):249.
Piva S, Fagoni N, Latronico N (2019) Intensive care unit-acquired weakness: unanswered questions and targets for future research. F1000Research, 8, F1000 Faculty Rev-508.
Raurell-Torredà M, Regaira-Martínez E, Planas-Pascual B et al. (2021) Early mobilisation algorithm for the critical patient. Expert recommendations. Enfermeria intensive. 32(3):153-163.
Reade MC, Finfer S (2014) Sedation and delirium in the intensive care unit. The New England journal of medicine. 370(5):444-454.
Rousseau AF, Prescott HC, Brett SJ et al. (2021) Long-term outcomes after critical illness:recent insights. Crit Care 25, 108.
Shekar K, Buscher H, Brodie D (2020) Protocol-driven daily optimisation of venovenous extracorporeal membrane oxygenation blood flows:an alternate paradigm? Journal of thoracic disease. 12(11):6854-6860.
Vieira R, Segura-Grau E, Magalhães J et al. (2020) Lung ultrasound as a tool to guide respiratory physiotherapy. Journal of clinical ultrasound. 48(7):431-434.
Yang R, Zheng Q, Zuo D et al. (2021) Safety Assessment Criteria for Early Active Mobilization in Mechanically Ventilated ICU Subjects. Respiratory care. 66(2):307-315.
Zink EK, Kumble S, Beier M et al. (2021) Physiological Responses to In-Bed Cycle Ergometry Treatment in Intensive Care Unit Patients with External Ventricular Drainage. Neurocritical care. 35(3):707-713












