ICU Management & Practice, Volume 16 - Issue 3, 2016
Many patients presenting to the hospital emergency department do not need to stay overnight. Ambulatory emergency care (AEC) may optimise identification and management of such patients by delivering streamlined, efficient patient care within one working day. This may improve clinical outcomes, patient experience and lower costs.
At James Paget University Hospital, the acute medicine unit (AMU) was organised into two units. The Emergency Assessment and Discharge Unit (EADU) immediately reviewed and treated patients who were likely to need therapies and investigations as an inpatient. The Ambulatory Emergency Care (AEC) unit served patients with fewer needs. As the AEC service could not keep up with demand, the hospital management redesigned the patient management streams and established a new unit, the Ambulatory Care Unit (AmbU) where point-of-care testing (POCT) was a core component of the new service.
Process Redesign
The project team included hospital staff, with industry partner support and sponsorship from Abbott Point-of-Care, Radiometer® and Operasee Limited.
The redesign process comprised (Figure 1):
1. Demand and Process Activity Mapping to understand how the current system worked and to identify an evidence-based, ideal future state of the service, which could fulfil demand. This identified leverage points on which to focus, such as POCT, to catalyse change.
2. Failure Mode Effect Analysis (FMEA), a step-by-step approach to identifying all possible failures in a design, process, product or service. FMEA was used to get input from multiple stakeholders to identify, quantify, prioritise and resolve potential issues in terms of how severe they might be, how often they might occur and how they could be detected.
To reach the goal of reduced length of stay (LoS), the new service implemented the following:
• POCT, including the i-STAT® System*;
• Appropriate treatment/discharge planning;
• Early senior clinical decision maker input;
• Condition-specific management algorithms.
POCT fulfilled over 85% of patient diagnostic needs in the AEC setting. The i-STAT® System was used for a variety of common tests, with the following cartridges used most widely:
• CHEM8+ to test blood electrolytes, basic haematology parameters and TCO2;
• CG4+ to test lactate and blood gases;
• PT/INR to test prothrombin time.
In addition the CELL-DYN Emerald® analyser was used for full blood count testing and the Radiometer® AQT90 FLEX for D-dimer tests.
Improved LoS
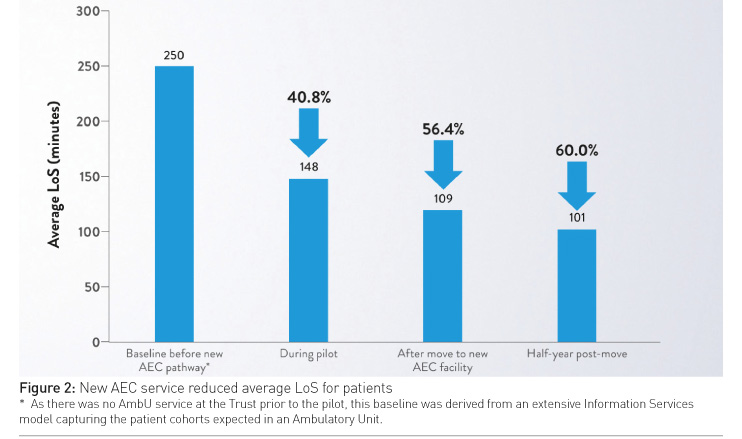
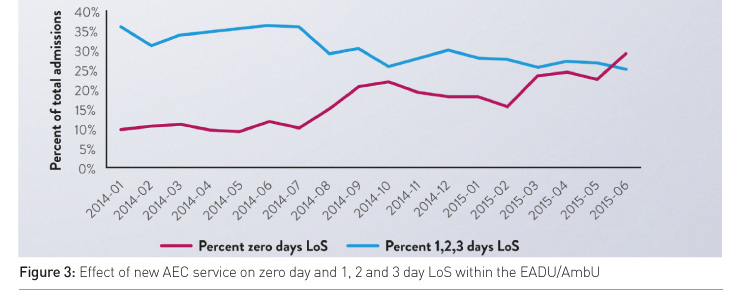
The new AEC pathway started in August 2014 (Monday through Friday, 08:30–18:30). The three-month pilot led to dramatic improvements in patient flow and reductions in LoS (Figure 2). These improvements continued after the pilot and after the AmbU moved into a newly built space located within the AMU with additional staff to support the extended service (Figure 2). Emergency care was improved as a result of the new outpatient AEC service, in both the EADU and the AmbU. The rate of patients going home on the same day increased and the rate of patients admitted for 1, 2 or 3 days decreased, demonstrating that fewer patients required overnight stays. The reduced LoS was achieved despite the patient admission rate remaining constant (Figure 3).
Cost Benefit > £1 million
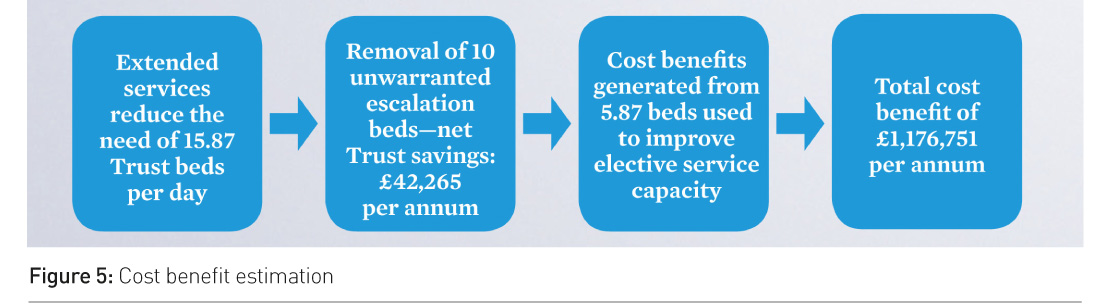
Following the pilot’s success, a business case was approved to provide 7-day AEC services, with operational hours extended from 08:30– 18:30 to 08:00–21:30. It was calculated that the extended AEC services would save 15.87 Trust beds per day within the EADU (Figure 4).
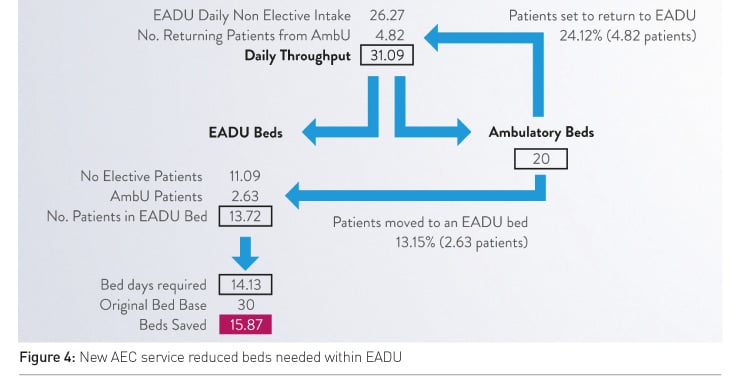
Despite the decrease in overnight stays, which reduced Trust income, but represented a £557,146 saving for the Clinical Commissioning Group, and the cost of providing the service (increased staffing and POCT diagnostics, etc.), it was estimated that implementation of the service would result in a net Trust saving of £42,265 per year in the acute setting— through the safe removal of 10 unwarranted escalation beds. The remaining capacity (approximately 5.87 beds) could be used to improve elective service capacity. This equates to a total economic cost benefit of £1,176,751 per annum (Figure 5).
Benefits for
Patients, Staff
Additional POCT benefits experienced at this site included:
• Patient data integration within the hospital information system;
• Senior clinical decision maker review within one hour;
• Static readmission rates;
• Positive patient feedback with 79% “extremely likely” to recommend the service;
• Under 10 minutes to initial review.
In the hospital setting, inefficient triage systems, prolonged radiology and central laboratory turnaround times, along with insufficient/ non-flexible staffing, contribute to inefficient operations and patient queuing. By incorporating process redesign changes, the AmbU has become an integral part of the emergency care system within the JPUH.
Following the pilot, some staff felt that the i-STAT® System gave them more time with the patient. They also felt that it increased their ability to communicate with the patients about their results.
Conclusion
The new AEC service at JPUH concentrated on the implementation of POCT and process redesign. Integrated POCT devices, such as the i-STAT® System (providing multiple traditionally laboratory- associated tests on a portable single platform), are designed to provide rapid diagnostic information that enables faster clinical management decisions. Within the new AEC service, this helped reduce LoS and costs. Other benefits may also be realised when POCT is incorporated into a workflow that allows real-time availability of results, including improved patient satisfaction and clinical outcomes.
The results shown here are specific to one healthcare facility, and may differ from those achieved by other institutions.
For in vitro diagnostic use only
For
intended use and complete product information, visit www.abbottpointofcare.com
© Abbott Point of Care Inc.
i-STAT and CELL-DYN Emerald are registered trademarks of the Abbott Group of Companies in various jurisdictions. POCcelerator is a trademark of CONWORX Technology GmbH. Radiometer is a registered trademark of Danaher Medical ApS.
James Paget University Hospital
Great Yarmouth, Norfolk, UK
Catchment
area: 240,000 residents
Emergency admissions per year: 67,000
Abbreviations
AEC ambulatory emergency care
AmbU ambulatory care unit
AMU acute medicine unit
EADU emergency assessment and discharge unit
LoS length of stay
POCT point-of-care testing









