ICU Management & Practice, Volume 16 - Issue 4, 2016
To initiate, maintain and advance a quality improvement programme in your intensive care unit consumes large amounts of time and energy. There are many advantages for quality management in joining an intensive care registry; the most important is access to precisely defined data for comparative audit.
Intensive Care Registries
Joint collection of information about intensive care patients, their treatment and outcomes began in the 1950s with the aim of communicating and exchanging experiences (Norlander et al. 1961). From these early attempts several initiatives to collect and analyse comprehensive sets of information from a large number of intensive care units (ICUs) emerged, with a focus initially to document and learn from daily practice. Registries then developed from collecting data from discharged patients’ charts to collect more reliable data that were defined in advance. The relevance of registries grew by moving from information that was accumulated at the ICU level to individual patient-level data. While sketchy data that characterised ICUs by describing levels of activity (i.e. number of admissions, length of stay, workload etc.) were useful at the start, registries holding detailed individualised information on consecutive patients (i.e. characteristics, diseases, interventions, outcomes) for long periods of time became powerful tools, which generated important observations from the ‘real world’ (Goldfrad and Rowan 2000). Over the years the scope of registries has expanded and the current agenda of many include issues of performance and accountability, often in partnerships with national intensive care societies or similar professional bodies with the general purpose to improve intensive care quality (for a collection of registries see icuregswe.org/registries).
Intensive Care
Quality
A commonly applied framework to define intensive care quality uses five domains (www.qualitymeasures.ahrq.gov). These are the classical three domains of the Donabedian model (structure, process and outcome) (Donabedian 1978) and two additional domains: access to intensive care and patient experience. Structure indicators represent organisation, resources and equipment; process indicators are about the process of care between caregiver and patient, what we do or fail to do for patients and their families; and outcome indicators represents the results that we achieve at the patient level. Access to intensive care is the ability to provide timely and appropriate care. Patient experience in the context of intensive care may not only include patients’ experiences but also include family members’ observations. The structure, process, access and experience domains must be linked to a clinically relevant set of outcomes. Collectively they determine the value of intensive care, since value may be defined as a given outcome divided by the cost associated with the particular outcome. This relationship provides a link between quality and value of care (Murphy et al. 2015).
Management of
Intensive Care Quality
Goodwill and enthusiasm of bedside physicians and nurses are important but not sufficient for improvement of intensive care quality. ICU directors and leaders who foster and enhance professional collaboration, authentic communication and transparent governance are instrumental for effective teamwork and delivery of high quality care. Numerous practices and tools that improve intensive care have been described, some operational in the ICU microsystem (close to the patient) others at the organizational level (Guidet et al. 2016). The critical first step to most approaches is measurement. However, as Deming pointed out, collecting a profusion of figures and turning out volumes of records is not quality management (Deming 1972). Measurements, commonly used to construct quality indicators, must fit into an ICU quality improvement programme with the purpose of helping us understand, control and improve the processes and systems within which we work. A good quality measure must be important, valid, reliable, responsive, interpretable and feasible (Curtis et al. 2006). The relative emphasis of these properties may vary across cultural and medical contexts, as suggested by the differing choices and priorities of quality indicators among countries and between individuals (Flaatten 2012; Rhodes et al. 2012).
How Can Registries
Support Quality Management?
Initiating, maintaining or advancing a local improvement programme consumes large amounts of time and energy. Joining an intensive care registry reduces the burden for an ICU and is associated with a number of important advantages. The efforts that are needed to educate staff, identify targets for improvement, select appropriate metrics, acquire necessary data, and analyse the data may be shared with other ICUs within the registry. This can be done without abandoning local priorities; it may instead stimulate local quality improvement work.
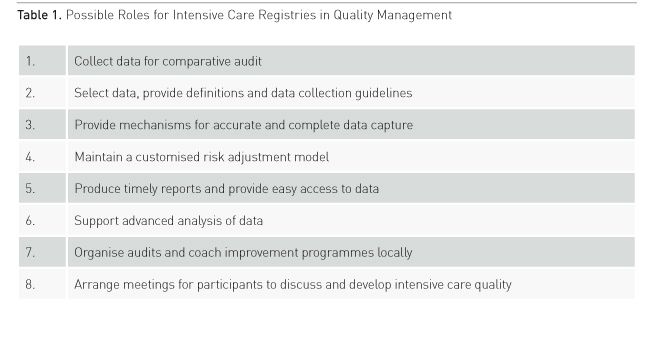
A few areas wherein participation in a registry may be particularly helpful are discussed briefly below and outlined in Table 1.
Data for Comparison
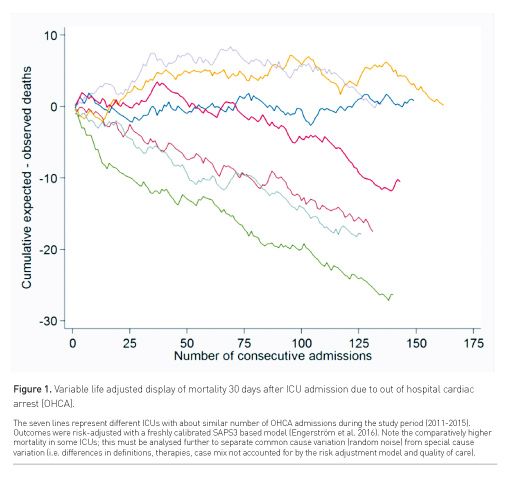
The need for quality improvement in your ICU is best understood if there are data available about comparative performance (Figure 1). Hence the most important undertaking of a registry is to support collection of precisely defined data from a group of ICUs. The hard work that is needed to establish routines and methods in an ICU for timely and sustainable data collection is often underestimated. Many registries offer a kick start by giving help to create an infrastructure for viable data collection for newcomers; this is useful to increase the chances of success.
Data Selection and Definitions
Intensive care is at an advantage in that it is an environment rich in data and has a quite common and clearly defined principal outcome measure (death). An important role of registries is to harmonise selection of variables. However, data collection, whether for use locally or within a registry, must be selected to fit into a carefully considered plan for quality improvement. The recording of information without a specific purpose may otherwise lead to poor data quality and registration fatigue. If there is a need for more extensive recording, the basic dataset may be accompanied by time-limited collection
of more extended datasets focusing on specific areas, e.g. treatment and outcomes of a carefully characterised elderly population. Variables should preferably be oriented toward a set of outcomes that matters to patients and families. However, collection of such information, which may include health-related quality of life and long-term survival, requires that we expand our ability to capture data in patients’ disease trajectories in other parts of the care delivery system than the ICU. For management of intensive care quality the duration of follow-up must balance between what is most affected by care in the ICU, least affected by varying administrative policies (i.e. discharge to terminal care facilities), practically feasible for caregivers and most relevant for patients.
An important and helpful function that is provided by registries is to develop dictionaries and guidelines for data collection. These contain explicit and detailed definitions of variables as well as explicit rules for deciding how variables must be recorded, and they are regularly updated to fit changing circumstances.
Data Accuracy and Coverage
To be able to provide meaningful analyses registries must have mechanisms in place that aid and confirm that imported data are valid, accurate and that coverage is complete. Ensuring complete coverage, i.e. that every patient that meets registry entry criteria is recorded, is particularly important to reduce the risk of selection bias. Validation of individual records includes looking for missing, unusual and invalid data, while validation at the ICU level means checking for unusual patterns, duplication and inconsistencies. The methods used by intensive care registries are usually also designed to help participating ICUs to identify and correct errors in their system for local data collection. Besides, registries may coordinate schemes for monitoring of accuracy and coverage by verification of patient records with source data. This is usually done after selecting a random number of records to be analysed with use of specific protocols, either internally by ICU staff or externally by an assessor visiting from the registry or another ICU.
Case-Mix Adjustment
A challenge for comparative audit of intensive care is that patients of all ages receive intensive care for a variety of disorders and symptoms; any effect of variation in intensive care quality on outcomes may be hidden by differences in patient demographics, underlying health status, acute conditions and severity of illness (collectively referred to as ‘case mix’). Comparing outcomes must take case mix into account and stratify or adjust for factors and circumstances that relate to the patient, comorbidities, acute disease and treatment before admission to ICU. Fortunately, intensive care has a history of using case mix adjusted models (usually risk adjustment models of in-hospital death) for benchmarking and audit of performance. An important mission for a registry is to maintain a validated, customised and updated risk adjustment model (Harrison et al. 2015; Engerström et al. 2016). Adjusting for risk is not only necessary for measuring outcomes accurately, but also for improving them. Understanding the link between risk factors and outcomes of critical illness is important for advancing intensive care.
Data Feedback and Access
Intensive care registries facilitate discussion and learning by producing reports that display relevant comparisons between member ICUs. If this is done with short report cycles, dataquality will most likely benefit from the frequent input of data from participating ICUs. Access to data must allow identification of participants to be useful for comparative audit. Transparent control of registries helps to build trust between participants leading to an environment where openness and sharing of information become powerful factors for delivery of high quality care. Ideally, information for comparative audit should be open and identifiable per ICU to facilitate comparisons. This has been the case in Sweden for more than a decade, where the open web portal of the Swedish Intensive Care Registry allows detailed analysis of frequently updated information (portal.icuregswe.org). The willingness to measure and share results, also when suboptimal, must be tied together with a communication strategy that includes readiness to educate media and the lay public.
Data Analysis
Best use of the registry is to allow data to be analysed locally by the ICU, in addition to centralised regular production of reports. An added advantage of local analysis is that data are often of better quality if those collecting them are involved in using and analysing them. Registries usually have skills and the infrastructure to perform complex and expanded analyses when asked for by member ICUs. Such analyses may include checking performance of the risk adjustment model and analysing associations between patient and care characteristics, and outcomes.
Local Audit and Improvement Programmes
Many registries arrange and support clinical audit with the overall aim to establish and improve intensive care quality. Organisation of site visits by peers or regular audits involving similar sized neighbouring ICUs may be an initial step in an improvement process (Martin and Braun 2014). The science of improving healthcare involves a systems approach, as well as applying specific knowledge in areas such as workplace psychology, practice-based learning and sources of variation. Numerous specific methods and tools are available (i.e. Breakthrough methodology, Clinical microsystem, Plan-DoStudy-Act [PDSA] cycle). Registries with expert knowledge in improvement science should be given the lead to avoid wasting of resources, energy and enthusiasm locally.
Conclusion
To develop, implement, evaluate and sustain a quality improvement programme in the ICU is an important and demanding undertaking. The work can be made easier by joining an intensive care registry. Mature registries have resources and knowledge that go beyond collection of well-defined data for comparative audit; they provide analyses, feedback reports, and a structure in which ICUs discover and discuss the findings in order to improve treatment and organisation. While improving clinical outcomes may be considered a competitive advantage in some healthcare models, sharing results and best practices is in the interest of the critically ill patients that we all serve.
References:
Curtis JR, Cook DJ, Wall RJ et al. (2006) Intensive care quality improvement: A “howto” guide for the interdisciplinary team. Crit Care Med 34(1): 211-218.
Deming WE (1972) Report to management. Quality Progress 5(7): 2-3,41.
Donabedian A. (1978) The quality of medical care. Science 200(4344): 856-864.
Engerström L, Kramer AA, Nolin T et al. Comparing time-fixed mortality prediction models and their effect on ICU performance metrics using the Simplified Acute Physiology Score 3. Crit Care Med 2016 Aug 2 [Epub ahead of print].
Flaatten H. (2012) The present use of quality indicators in the intensive care unit. Acta Anaesthesiol Scand 56(9): 1078-1083.
Goldfrad C, Rowan K. (2000) Consequences of discharges from intensive care at night. Lancet, 355(9210): 1138-1142.
Guidet B, Valentin A, Flaatten H. (2016) Quality management in intensive care. A practical guide. Cambridge University Press, Cambridge, UK.
Harrison DA, Ferrando-Vivas P, Shahin J et al. Ensuring comparisons of health-care providers are fair: development and validation of risk prediction models for critically ill patients. Health Serv Deliv Res 3(41): 1-119.
Martin J, Braun J-P. (2014) Qualitätsmanagement in det Intensivmedizin. Anaesthetist 63(2): 163-172.
Murphy DJ, Ogbu OC, Coopersmith CM. (2015) ICU director data. Using data to assess value, inform local change, and relate to the external world. Chest 147(4): 1168-1178.
Norlander OP, Bjork VO, Crafoord C et al. (1961) Controlled ventilation in medical practice. Anaesthesia, 16(3): 285-307.
Rhodes A, Moreno RP, Azoulay E et al. (2012) Prospectively defined indicators to improve the safety and quality of care for the critically ill patients: a report from the Task Force on safety and Quality of the European Society of Intensive Care Medicine (ESICM). Intensive Care Med 38(4): 598-605.







