ICU Management & Practice, Volume 21 - Issue 3, 2021
Introduction
The SARS-CoV-2 virus responsible for the COVID-19 pandemic has a wide variety of clinical presentations. Age is the most important risk factor for critical illness and a poor prognosis, typically beginning on the seventh day after the onset of symptoms. In a large cohort of symptomatic patients who were followed early during the pandemic, 81% presented with mild disease, 14% had severe disease and 5% became critically ill (Berlin 2020). The most important variables associated with high mortality were age, presence of diabetes, obesity, and severe acute respiratory distress syndrome [ARDS] (Schimdt 2021). Regarding the high mortality associated with ARDS, it is known that adequate programming and manoeuvres to maintain an effective invasive ventilation strategy are significantly associated with a reduction in mortality.
Protective Mechanical Ventilation
In the setting of care of a patient with severe and critical COVID-19, a lung support strategy with invasive mechanical ventilation reaching alveolar protection targets is a priority, currently remaining the most impactful target measure on survival.
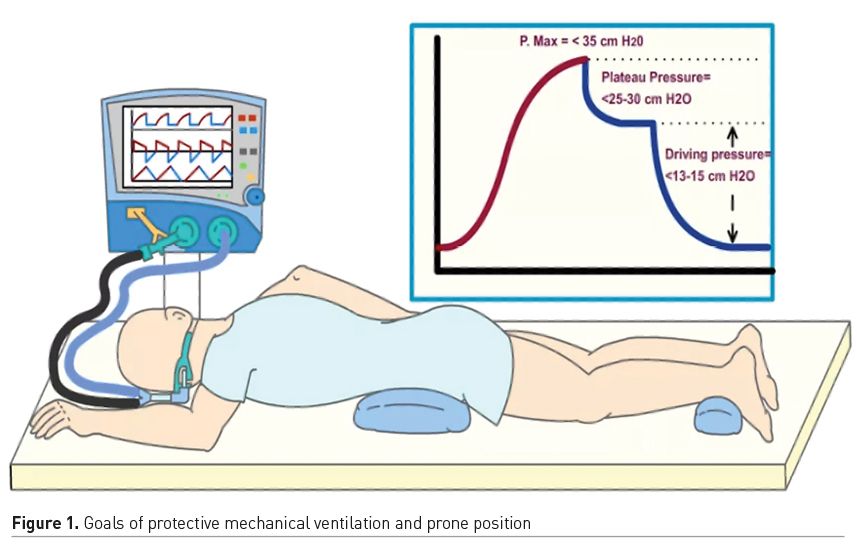
The goals of protective ventilation are decisive in the prognosis and evolution of patients with ARDS, therefore patient care should always be individualised based on their clinical presentation, haemodynamics and other conditions like availability of resources. The WHO proposes to perform protective ventilation in patients with ARDS due to COVID-19. It is critical to maintain a tidal volume (Vt) between 4-8 ml/kg adjusted to predicted weight (Brower 2000), establish a positive pressure at the end of expiration (PEEP), perform plateau pressure (Pp) and drive pressure measurements and keep them under their respective goal, as well as maintain normocapnia and normoxaemia (Figure 1).
The LOV-ED study proposes to perform protective ventilation in the emergency department since results showed a decrease in mortality, shorter stay in the ICU, and days off of mechanical ventilation in the group that was provided with a liberal strategy of ventilatory support. The ARMA study demonstrated that low Vt ventilation in patients with ARDS led to a significant decrease in in-hospital mortality. LUNG SAFE, an observational multicentre study demonstrated that mortality of severe ARDS in the intensive care unit is 46.1%, which is why it emphasises protective ventilation strategies. The ARDS Clinical Trials Network ALVEOLI study included 549 patients, the Lung Open Ventilation Study (LOVS) 983 patients, and the ExPress trial almost 1000 patients. The results of the three studies consistently showed that an indiscriminate increase in PEEP strategy does not change survival in ARDS.
Amato (2015) conducted a retrospective analysis and coined the term driving pressure (Dp) or distending pressure (Pp - PEEP). Decreases in Dp due to changes in ventilator settings were strongly associated with an increase in survival establishing as cut point less than 13 cm H2O. Villar (2017) evaluated the risk of hospital death based on Vt, PEEP, Pp, and Dp for 24 hours under protective ventilation to predict hospital mortality, reproducing what was reported by Amato.
Pelosi (2018) proposes to maintain a strategy with closed lungs and at rest, thus minimising ventilator-induced lung injury (VILI). High PEEP is associated with alveolar overdistension, oedema formation, decrease in lymphatic drainage, and deterioration of right ventricular function, as well as the impact on systemic haemodynamics. Also, a Pp <25-30 cm H2O is associated with a decrease in the proportion of hospital mortality.
It is recommended to start with a Vt of 6 ml/kg and do an inspiratory pause to measure the Pp. If it exceeds 30 cm H2O, the Vt should be decreased until it is 30 cm H20. It is not recommended to lower the Vt less than 4 ml/kg because of the risk of severe hypercapnia and atelectasis. Dp in numbers greater than 13 to 15 cm H2O have been associated with higher mortality (Amato 2015; LUNGSAFE, 2016); however, there are currently no prospective studies supporting Dp as a target of alveolar protection in patients with COVID-19 (despite this lack of evidence, there is a strong recommendation by international guidelines in ARDS produced by SARS-CoV-2 sustained by remaining evidence in all-cause ARDS).
Positive end-expiratory pressure (PEEP) in patients with severe ARDS is recommended at high levels, up to 15 cm H2O of PEEP based on the low PEEP/FiO2 table of the ARDSnet group. Despite the arbitrary method it generated, it has been validated in several ways, remaining as the best supportable way of setting the PEEP. That is why we strongly suggest its use (Table 1).
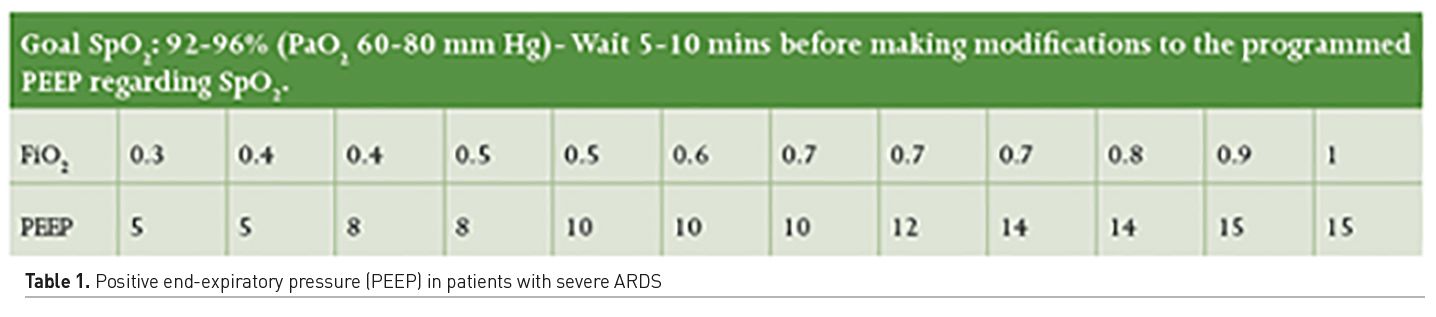
PaO2 and PaCO2 goals in ARDS must be maintained. These goals have been associated with survival within an O2 range by pulse oximetry between 88 to 92-95% (Brower 2000; Papazian 2019). But in severe COVID-19, a target of SpO2 between 92 to 96% is recommended. It is also recommended to keep PaO2 between 60 to 100 mm Hg, as well as maintain strict supervision of PaCO2 levels in order to keep less than 60-80 mm Hg as a secondary target.
Protective ventilation (and thus virtually every patient under mechanical ventilation) should avoid mechanical ventilation-induced injury (VILI). Close monitoring of respiratory system pressures should be performed to avoid barotrauma, with peak pressure (Pmax) less than 35 cm H2O, Pp less than 25 cm H2O, Dp less than 13 cm H2O. With these interventions we can limit the damage and improve the prognosis and survival of patients with ARDS (Figure 1).
Prone Positioning
The first report on prone position (PP) in patients with acute respiratory distress syndrome (ARDS) appeared in 1976 and described a marked improvement in oxygenation. It is now clearly recognised that PP is associated with a significant improvement in oxygenation rates. In various studies in both animals and humans, it has been found that PP can reduce lung injury associated with mechanical ventilation (Figure 1).
ARDS is characterised by disruption of the alveolar-capillary barrier, with an increase in its permeability, alveolar oedema, also associated with depletion of lung surfactant, leading to alveolar instability and alveolar collapse. Lung involvement is heterogeneous, with well-ventilated lung regions, which participate in gas exchange, and in other areas that are collapsed by pressure superimposed by interstitial and alveolar oedema, mechanisms that explain the decrease in lung volume in these patients, thus lower Vt requirements. PP allows these alveolar areas to be recruited, redistributing and homogenising ventilation, decreasing the intrapulmonary shunt, improving oxygenation, ventilation, and lung mechanics. However, the degree of recruitment depends on factors such as the severity of the lung involvement, the pronation time, and the time elapsed from the lung injury to the pronation of the patient.
Patients with COVID-19 with moderate to severe ARDS seem to respond well to invasive ventilation in PP, which makes PP ventilation recommended in international guidelines for the treatment of COVID-19. This is corroborated in two meta-analyses and later in the PROSEVA trial, which showed a beneficial effect of PP in moderate to severe ARDS with an improvement in oxygenation and a reduction in mortality compared to the conventional supine position. PP is therefore one of three therapies that show a positive effect on ARDS mortality, with current volume reduction, and early use of neuromuscular blocking agents (NMBA). Its use in mild to moderate ARDS continues to be discussed, as well as the optimal duration of PP sessions. In the PROSEVA trial, they remained on average 17 hours in PP. A study conducted by Jochmans et al. (2020) showed that the beneficial physiological effects continued with even 16 hours of PP and 24 hours in some patients.
The guide for the treatment of ARDS recommended the use of PP for at least 16 hours a day in patients with moderate-severe ARDS with a PaO2/FiO2 ratio <150. The criteria for responding to mechanical ventilation in PP are an increase of 20% in PaO2/FiO2, 10 mm Hg in PaO2, and 1 mm Hg decrease in PaCO2 at 4 hours after the manoeuvre.
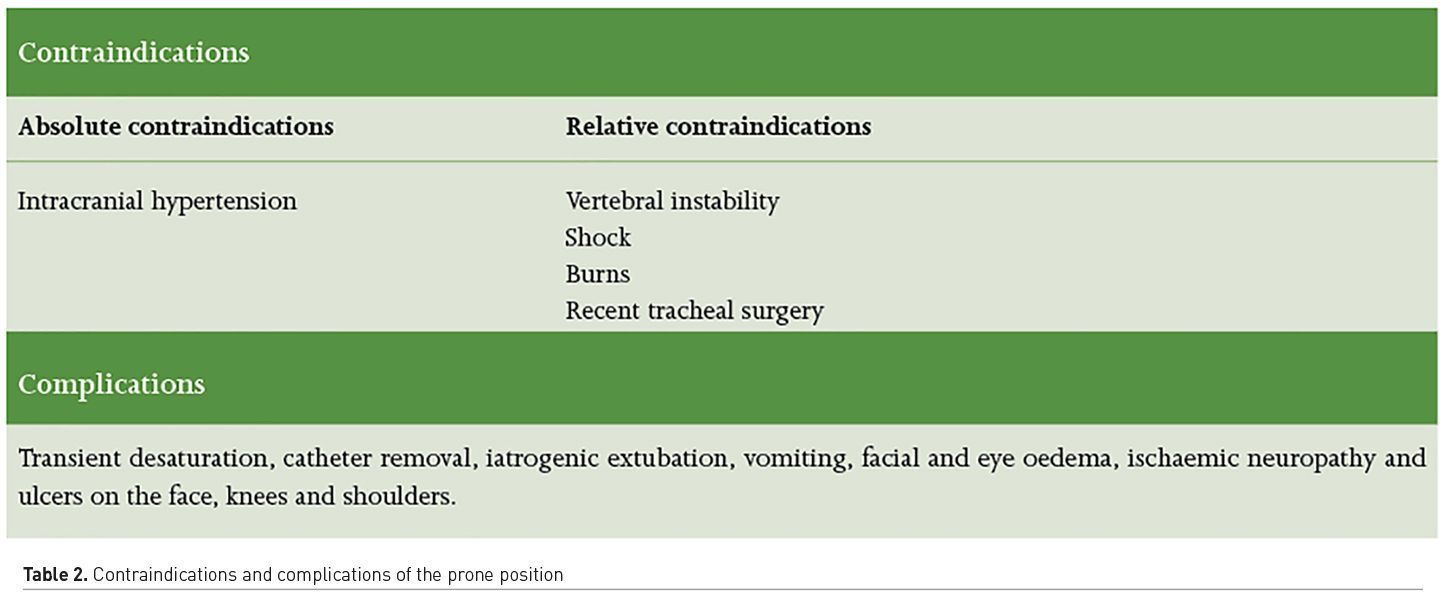
Trained personnel are required to perform the PP of a patient under mechanical ventilation as they can identify its risks and complications. A delay greater than three days to the pronation of a patient with ARDS does not confer any benefit, so this technique should be used before 12 to 72 h of IMV, always based on its indications and contraindications (Table 2). It is suggested to keep patients in the supine position who, after having been pronated, can maintain a PaO2/FiO2 >150 after 4 hours in this position.
Recruitment Manoeuvres
WHO strongly recommends not to routinely perform recruitment manoeuvres. They can be considered in case of hypoxaemia refractory to the previous strategies. To date, there is no described ideal form of alveolar recruitment. A strategy using a lung recruitment manoeuvre and titrated PEEP increased mortality of patients with moderate to severe ARDS (Biasi 2017).
Conclusion
Low Vt with prone ventilation is associated with the greatest reduction in mortality for critically ill adults with moderate to severe ARDS. Reproducible protective ventilation strategies must be carried out to obtain better outcomes (Sud and Mathews 2021).
Conflict of Interest
None.
References:
Acute Respiratory Distress Syndrome Network, Brower RG, Matthay MA, Morris A et al. (2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med, 342(18):1301–8.
Alhazzani W, Alshahrani M, Jaeschke R et al. (2013) Neuromuscular blocking agents in acute respiratory distress syndrome: a systematic review and meta-analysis of randomized controlled trials. Crit Care, 17(2):R43.
Amato MBP, Meade MO, Slutsky AS et al. (2015) Driving Pressure and Survival in the Acute Respiratory Distress Syndrome. N Engl J Med, 19;372(8):747–55.
Berlin DA, Gulick RM, Martinez FJ (2020) Severe Covid-19. N Engl J Med, 17;383(25):2451–60.
Boles JM, Bion J, Connors A et al. (2007) Weaning from mechanical ventilation. Eur Respir J, 29(5):1033–56.
Fuller BM, Ferguson IT, Mohr NM et al. (2017) Lung-Protective Ventilation Initiated in the Emergency Department (LOV-ED): A Quasi-Experimental, Before-After Trial. Ann Emerg Med, 70(3):406-418.e4.
Gattinoni L, Taccone P, Carlesso E et al. (2013) Prone Position in Acute Respiratory Distress Syndrome. Rationale, Indications, and Limits. Am J Respir Crit Care Med, 188(11):1286–93.
Gattinoni L, Carlesso E, Taccone P et al. (2010) Prone positioning improves survival in severe ARDS: a pathophysiologic review and individual patient meta-analysis. Minerva Anestesiol, 76(6):448–54.
Guérin C, Reignier J, Richard JC et al. (2013) Prone Positioning in Severe Acute Respiratory Distress Syndrome. N Engl J Med, 368(23):2159–68.
Higher versus Lower Positive End-Expiratory Pressures in Patients with the Acute Respiratory Distress Syndrome. (2004) N Engl J Med, 22;351(4):327–36.
Jochmans S, Mazerand S, Chelly J (2020) Duration of prone position sessions: a prospective cohort study. Ann Intensive Care, 10(1):66.
Liao X, Wang B, Kang Y (2020) Novel coronavirus infection during the 2019–2020 epidemic: preparing intensive care units—the experience in Sichuan Province, China. Intensive Care Med, 46(2):357–60.
Mathews KS, Soh H, Shaefi S et al. (2021) Study of the Treatment and Outcomes in Critically Ill Patients with Coronavirus Disease (STOP-COVID) Investigators. Prone Positioning and Survival in Mechanically Ventilated Patients With Coronavirus Disease 2019-Related Respiratory Failure. Crit Care Med.
Meade MO, Cook DJ, Guyatt GH et al. (2008) Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA, 299(6):637–45.
Meng L, Qiu H, Wan L et al. (2020) Intubation and Ventilation amid the COVID-19 Outbreak. Anesthesiology, 132(6):1317-1332.
Mercat A, Richard J-CM, Vielle B et al. (2008) Positive End-Expiratory Pressure Setting in Adults With Acute Lung Injury and Acute Respiratory Distress Syndrome: A Randomized Controlled Trial. JAMA,13;299(6):646.
Mora-Arteaga JA, Bernal-Ramírez OJ, Rodríguez SJ (2015) The effects of prone position ventilation in patients with acute respiratory distress syndrome. A systematic review and metaanalysis. Med Intensiva, 39(6):359–72.
Nitta K, Okamoto K, Imamura H et al. (2019) A comprehensive protocol for ventilator weaning and extubation: a prospective observational study. J Intensive Care, 6;7(1):50.
Papazian L, Aubron C, Brochard L et al. (2019) Formal guidelines: management of acute respiratory distress syndrome. Ann Intensive Care, 13;9(1):69.
PelosiP, Rocco PRM, Gama de AbreuM (2018) Close down the lungs and keep them resting to minimize ventilator-induced lung injury. Crit Care22, 72.
Schmidt M, Hajage D, Demoule A et al. (2021) Clinical characteristics and day-90 outcomes of 4244 critically ill adults with COVID-19: a prospective cohort study. Intensive Care Med, 47(1):60–73.
Staff safety during emergency airway management for COVID-19 in Hong Kong. Available from https://alatorax.org/es/biblioteca/staff-safety-during-emergency-airway-management-for-covid-19-in-hong-kong
Sud S, Friedrich JO, Taccone P et al. (2010) Prone ventilation reduces mortality in patients with acute respiratory failure and severe hypoxemia: systematic review and meta-analysis. Intensive Care Med, 36(4):585–99.
Sud S, Friedrich JO, Adhikari NK et al. (2021) Comparative Effectiveness of Protective Ventilation Strategies for Moderate and Severe ARDS: Network Meta-Analysis. Am J Respir Crit Care Med. doi: 10.1164/rccm.202008-3039OC.
Villar J, Martín-Rodríguez C, Domínguez-Berrot AM et al. (2017) A Quantile Analysis of Plateau and Driving Pressures: Effects on Mortality in Patients With Acute Respiratory Distress Syndrome Receiving Lung-Protective Ventilation. Crit Care Med, 45(5):843–50.
World Health Organization (2020) Clinical management of severe acute respiratory
infection SARI) when COVID-19 disease is suspected. Interim guidance. Pediatr Med Rodz, 16(1):9–26.
Yang X, Yu Y, Xu J et al. (2020) Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med, 8(5):475–81.
Ye L, Yang S, Liu C (2020) Infection prevention and control in nursing severe coronavirus disease (COVID-19) patients during the pandemic. Crit Care, 12;24(1):338.












