ICU Management & Practice, Volume 21 - Issue 4, 2021
Among 1,841 very old ICU patients with respiratory failure, although women had higher age and frailty, males had higher 30-day mortality assessed one month after ICU admission. Particularly in light of the ongoing pandemic, male patients appear to be at significantly higher risk for worse outcomes than females.
Introduction
Demographic change does not stop at the intensive care unit (ICU). Among all ages, the very old ICU patients (VIP) are a fast-expanding subgroup (Flaatten et al. 2017a). For Europe, approximately 24.4 million people older than 85 years in 2040 are expected. But this development is not limited to Europe; it has been assumed that worldwide the percentage of patients older than 60 years will rise from approximately 12% in 2013 to 21% in 2050 (Leblanc et al. 2017). This demographic shift already has an impact on the admission rates of VIP in ICU in the past decade (Ihra et al. 2012). This observation has potential major impact on hospital, ethical issues, and the health economy. VIPs are generally patients at risk; large prospective trials found a 30-day-mortality of 42% (de Lange et al. 2019). Within this special group of VIPs, gender differences in treatment outcomes have been reported for many medical conditions (Schiele et al. 2011). However, in this particularly vulnerable high-risk population of ICU patients, the available evidence is heterogeneous (Schoeneberg et al. 2013; Park et al. 2018). Male and female ICU patients differ in baseline characteristics, predisposition to disease, and these differences may influence outcomes (Tibullo and Esquinas 2019; Cillóniz et al. 2019). In very old septic VIPs male sex was an independent negative predictor of prognosis (Cillóniz et al. 2019; Martin et al. 2003). In contrast, female sex was identified as a risk factor for discontinuation or refusal of further ICU treatment (Block et al. 2019), although elderly women have a significantly higher survival after ICU stay than men (Hollinger et al. 2019). A recently published retrospective analysis of 17,146 ICU patients with sepsis found no clinically relevant sex-specific mortality differences (Wernly et al. 2020a). However, in another study of 7,555 very old intensive care patients, male sex was an independent risk factor for an adverse 30-day-mortality but not ICU-mortality (Wernley et al. 2020b).
Currently, it is unclear whether these observations also apply to patients with respiratory failure. This subgroup analysis uses data from two recent large, multinational studies of VIPs to compare male and female patients with regards to crude unadjusted and adjusted baseline characteristics and outcomes (Guidet et al. 2019; Flaatten et al. 2017b; D’Agonstino 2007; Guidet et al. 2020).
Methods
VIP1 and VIP2 were prospective, multicentre studies (ID: NTC03134807, NCT03370692) that recruited very old intensive care patients. VIPs were defined as patients admitted to an ICU and being 80 years or older. The recruitment process differed slightly between the two studies: For VIP1, each participating ICU could include either consecutive patients for three months or the first 20 consecutive patients fulfilling the inclusion criteria (all patients 80 years of age or older). Thus, data were collected between October 2016 and February 2017. For VIP2, VIPs were included from May 2018 to May 2019. In both studies, all experimental protocols were approved by the local institutional and/or licensing committees. Informed consent was obtained from all subjects if not omitted by the ethics vote. This post-hoc analysis of these two prospective trials examines all patients who were admitted for respiratory failure. The primary endpoint of this study was 30-day-mortality. Frailty was assessed by CFS as described previously (Rockwood et al. 2005; Jorm and Jacomb 1989; Katz 1983). Continuous data points are expressed as median ± interquartile range depending on the distribution. Differences between independent groups were calculated using the Mann-Whitney U-test. Categorical data are expressed as numbers (percentage). Chi-square test was applied to calculate differences. Univariable and multivariable logistic regression analysis was performed to assess associations with mortality. Odds ratios (OR) and adjusted odds ratios (aOR) with respective 95% confidence intervals (CI) were calculated. All tests were two-sided, and a p-value of <0.05 was considered statistically significant. Stata 16 was used for all statistical analyses.
Results
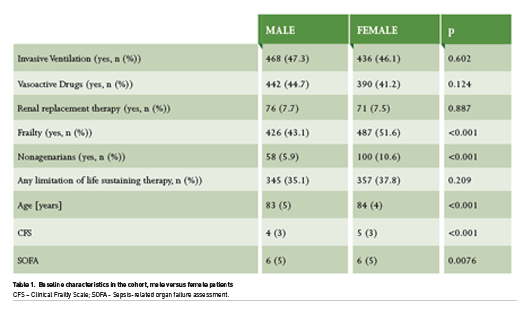
A subgroup of 1,841 patients with respiratory failure (938 male, 903 female) was included. Patient characteristics are summarised in Table 1. In the cohort, the proportion of nonagenarians was significantly greater among women. The mean age was also significantly lower (83±5 years for males versus 84±4 for females, p<0.001). When frailty was used as a binary marker (CFS > 4), significantly more women than men (43.1% in males versus 51.6% in females, respectively, p>0.001) could be classified as frail. Accordingly, the mean CFS was higher in females (4±3 for males, and 5±3 in males, respectively, <0.001). There was no difference in the use of invasive ventilation (47.3% in males versus 46.1% in females, respectively, p=0.602), and vasoactive drugs (44.7% versus 41.2%, p=0.124). Only very few patients needed renal replacement therapy without any difference between both groups (7.7% in males and 7.5% in females, respectively, p=0.887). We found no difference between men and women in the limitation of life sustaining therapy.
30-day-mortality was significantly higher in males (43% vs. 35%; OR 1.16 95% CI 1.06-1.26; p<0.001) in univariate analysis (Figure 1). The association between male sex and increased mortality remained after multivariable adjustment for age, SOFA, and frailty (aOR 1.18 95% CI 1.07-1.29; p=0.001).
.jpg)
Discussion
Male sex is an independent risk factor for mortality in very old intensive care patients with respiratory failure. Our previously published results also show different results depending on the subgroup and collective analysed (Wernly et al. 2020a; Wernly et al. 2020b). Thus, based on current scientific evidence, it might be speculated that the gender influence on mortality manifests itself primarily in elderly men with respiratory failure. It should be noted that not all types of respiratory failure have an infectious aetiology. This analysis shows that elderly male patients with respiratory insufficiency have a significantly worse prognosis than women, regardless of aetiology.
In general, data on gender differences in ICU patients are controversial. In the total cohort, we found male sex to be an independent risk factor for an adverse 30-day-mortality in very old intensive care patients (Wernly et al. 2020b). Our current results are in line with Cillóniz et al. (2019) who analysed 1,238 very old intensive care patients with community-acquired pneumonia. Men were significantly more likely to develop septic courses in this cohort, and male sex was an independent predictor of this in this context. However, in a large retrospective analysis of septic adult ICU patients of all ages, no gender difference was demonstrated (Wernly et al. 2020a). Accordingly, no gender difference was observed in a large cohort study on 25,998 patients without age-restriction for illness-adjusted mortality (Valentin et al. 2003).
It is well known from the literature that women and men are treated differently in the ICU. For example, Block et al. (2019) performed a registry study and used data from the Swedish Intensive Care Registry from 2014 to 2016. They analysed 97,095 patients and found that being female resulted in an increased risk for a treatment limitation of life sustaining therapy (OR 1.18; CI 1.13- 1.23). However, in the present sub-study from the VIP-trials in VIPs with respiratory failure, we could not observe this effect. If these gender differences do exist, the cause remains unclear and needs further exploration. Various explanatory models exist. For example, socioeconomic factors might influence outcomes (Ski et al. 2014). In addition, depending on the genesis of respiratory failure, there also appear to be significant pathophysiological-biochemical differences between the sexes which became especially apparent during the current SARS-CoV-2 pandemic.
It is known that when men are infected with viruses, they have increased susceptibility, different early pathogenesis, and a different balance in immune response and tissue consequences (Scully et al. 2020). It has been observed early that severity of the COVID-19 disease, outcome as well as antibody titers differed (Klein et al. 2020a). In SARS-CoV-2, there exist mechanistic differences between genders including in the expression and activity of angiotensin-converting enzyme 2 (ACE2) as well as in antiviral immunity (Klein et al. 2020b). In mice, it has been described that males are more susceptible to SARS-CoV compared to age-matched female mice. In these in vivo studies, male mice consecutively evidenced higher virus titers, resulting in more vascular leakage, alveolar oedema, and more inflammatory migration of monocytes, macrophages, and neutrophils. Interestingly, these gender-specific effects increased with advancing age, but decreased when female mice received ovariectomy or were treated with an oestrogen receptor antagonist (Channappanavar et al. 2017). In fact, several important mediators of the immune response such as monocytes, macrophages, and neutrophils express surface oestrogen receptors. The activation of these receptors leads to an enhanced production of interferon I and III, resulting in a reduced immune response, increased immune tolerance and antibody production (Mauvais-Jarvis et al. 2020; Suba 2020).
In the human disease course, this might explain why females with severe COVID-19 evidence lower inflammatory biomarkers compared to men (Mussini et al. 2021; Qin et al. 2020). Another centrally involved protein is transmembrane serine protease 2 (TMPRSS2). Together with other proteins, TMPRSS2 plays a crucial role in cell entry of coronaviruses. In fact, the viral surface spike SARS-CoV-2 protein penetrates host cells. TMPRSS2 splits the viral spike protein, which increases viral attachment to cell membranes (Hoffman et al. 2020). Under physiologic conditions, TMPRSS2 is upregulated by androgenic hormones and is primarily expressed in prostate secretory epithelial cells (Afshari et al. 2020). At least for coronaviruses, these gender differences appear to have implications resulting in an increased viral uptake in men (Qiao et al. 2020). Another possible pathogenesis leading to a milder course of respiratory failure in women compared with men appears to be Mas-receptor. In vitro, oestrogen increases the Mas-receptor expression leading to an attenuated endothelial leakage. In vivo, ovariectomy resulted in a decreased Mas-receptor expression and increased pulmonary damage (Erfinanda et al. 2021). Some gender differences in the immunomodulation are additionally dependent on the ageing process [immunoageing] (Gebhard et al. 2020).
These observations may be relevant in the context of currently tested immunomodulatory therapeutic approaches in critically ill COVID-19 patients. In a recent multicentre study, COVID-19 increased the risk of ICU-acquired bloodstream infections. This was possibly attributed to the increased use of anakinra and tocilizumab. Thus, the use of these drugs might be deleterious in elderly COVID-19 patients (Buetti et al. 2021).
Hence, our findings of differences in outcome in elderly patients with respiratory failure was already present before the existence of the SARS-CoV-2 pandemic. This needs further exploration but especially attention during the treatment of ICU patients. However, these findings became even more up-to-date in COVID-19. Currently, a global prospective observational study in 346 ICUs in 43 countries is investigating the outcome of very elderly patients infected with COVID-19 (Jung et al. 2021). We expect this study to provide deeper insights into this topic (NCT04321265, www.vipstudy.org).
In sum of these findings, there should be an awareness that there are gender differences - especially in elderly critically ill patients that affect outcome.
Conclusion
In very old ICU patients with respiratory failure, females evidence higher age and frailty, but male sex is an independent predictor of one month mortality. Particularly considering the ongoing pandemic, gender-specific management both during and after an ICU stay might reduce gender-specific outcomes.
Conflict of Interest
The authors declare that they have no competing interests.
Financial Disclosure Statement
No (industry) sponsorship has been received for this investigator-initiated study.
References:
Afshari A, Janfeshan S, Yaghobi R et al. (2020) Covid-19 pathogenesis in prostatic cancer and TMPRSS2-ERG regulatory genetic pathway. Infect Genet Evol, 88: 104669.
Block L, Petzold M, Syrous AN et al. (2019) Age, SAPS 3 and female sex are associated with decisions to withdraw or withhold intensive care. Acta Anaesthesiol Scand, 63: 1210-1215.
Buetti N, Ruckly S, de Montmollin E et al. (2021) COVID-19 increased the risk of ICU-acquired bloodstream infections: a case-cohort study from the multicentric OUTCOMEREA network. Intensive Care Med.
Channappanavar R, Fett C, Mack M et al. (2017) Sex-Based
Differences in Susceptibility to Severe Acute Respiratory Syndrome Coronavirus Infection. J Immunol, 198: 4046-4053.
Cillóniz C, Dominedo C, Ielpo A et al. (2019) Risk and Prognostic Factors in Very Old Patients with Sepsis Secondary to Community-Acquired Pneumonia. J Clin Med, 8: 961.
D' Agostino RB Jr. (2007) Propensity scores in cardiovascular research. Circulation, 115: 2340-2343.
de Lange DW, Brinkman S, Flaatten H et al. (2019) Cumulative Prognostic Score Predicting Mortality in Patients Older Than 80 Years Admitted to the ICU. J Am Geriatr Soc, 67: 1263-1267.
Erfinanda L, Ravindran K, Kohse F et al. (2021 Oestrogen-mediated upregulation of the Mas receptor contributes to sex differences in acute lung injury and lung vascular barrier
regulation. Eur Respir J, 57.
Flaatten H, de Lange DW, Artigas A et al. (2017a) The status of intensive care medicine research and a future agenda for very old patients in the ICU. Intensive Care Med, 43: 1319-1328.
Flaatten H, De Lange DW, Morandi A et al. (2017b) The impact of frailty on ICU and 30-day mortality and the level of care in very elderly patients (>/= 80 years). Intensive Care Med, 43: 1820-1828.
Gebhard C, Regitz-Zagrosek V et al. (2020) Impact of sex and gender on COVID-19 outcomes in Europe. Biol Sex Differ, 11: 29.
Guidet B, de Lange DW, Boumendil A et al. (2020) The contribution of frailty, cognition, activity of daily life and comorbidities on outcome in acutely admitted patients over 80 years in European ICUs: the VIP2 study. Intensive Care Med, 46: 57-69.
Hoffmann M, Kleine-Weber H, Schroeder S et al. (2020) SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell, 181: 271-280 e278.
Hollinger A, Gayat E, Feliot E et al. (2019) Gender and survival of critically ill patients: results from the FROG-ICU study. Ann Intensive Care, 9: 43.
Ihra GC, Lehberger J, Hochrieser H et al. (2012) Development of demographics and outcome of very old critically ill patients admitted to intensive care units. Intensive Care Med, 38: 620-626.
Jorm AF, Jacomb PA (1989) The Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE): socio-demographic correlates, reliability, validity and some norms. Psychol Med, 19: 1015-1022.
Jung C, Bruno RR, Wernly B et al. (2021) Inhibitors of the renin-angiotensin-aldosterone system and COVID-19 in critically ill elderly patients. Eur Heart J Cardiovasc Pharmacother, 7: 76-77.
Katz S (1983) Assessing self-maintenance: activities of daily living, mobility, and instrumental activities of daily living. J Am Geriatr Soc, 31: 721-727.
Klein SL, Pekosz A, Park HS et al. (2020a) Sex, age, and hospitalization drive antibody responses in a COVID-19 convalescent plasma donor population. J Clin Invest, 130: 6141-6150.
Klein SL, Dhakal S, Ursin RL et al. (2020b) Biological sex impacts COVID-19 outcomes. PLoS Pathog, 16: e1008570.
Leblanc G, Boumendil A, Guidet B (2017) Ten things to know about critically ill elderly patients. Intensive Care Med, 43: 217-219.
Martin GS, Mannino DM, Eaton S et al. (2003) The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med, 348: 1546-1554.
Mauvais-Jarvis F, Klein SL, Levin ER (2020) Estradiol, Progesterone, Immunomodulation, and COVID-19 Outcomes. Endocrinology, 161.
Mussini C, Cozzi-Lepri A, Menozzi M et al. (2021) Better prognosis in females with severe COVID-19 pneumonia: possible role of inflammation as potential mediator. Clin Microbiol Infect, S1198-1743X(1120)30765-30765.
Park J, Jeon K, Chung CR et al. (2018) A nationwide analysis of intensive care unit admissions, 2009-2014 - The Korean ICU National Data (KIND) study. J Crit Care, 44: 24-30.
Qiao Y, Wang XM, Mannan R et al. (2020) Targeting transcriptional regulation of SARS-CoV-2 entry factors ACE2 and TMPRSS2. Proc Natl Acad Sci USA, 202021450.
Qin L, Li X, Shi J et al. (2020) Gendered effects on inflammation reaction and outcome of COVID-19 patients in Wuhan. J Med Virol, 92: 2684-2692.
Rockwood K, Song X, MacKnight C et al. (2005) A global clinical measure of fitness and frailty in elderly people. CMAJ, 173: 489-495.
Schiele F, Meneveau N, Seronde MF et al. (2011) Propensity score-matched analysis of effects of clinical characteristics and treatment on gender difference in outcomes after acute myocardial infarction. Am J Cardiol, 108: 789-798.
Schoeneberg C, Kauther MD, Hussmann B et al. (2013) Gender-specific differences in severely injured patients between 2002 and 2011: data analysis with matched-pair analysis. Crit Care, 17: R277.
Scully EP, Haverfield J, Ursin RL et al. (2020) Considering how biological sex impacts immune responses and COVID-19 outcomes. Nat Rev Immunol, 20: 442-447.
Ski CF, King-Shier KM, Thompson DR (2014) Gender, socioeconomic and ethnic/racial disparities in cardiovascular disease: a time for change. Int J Cardiol, 170: 255-257.
Suba Z, (2020) Prevention and therapy of COVID-19 via exogenous estrogen treatment for both male and female patients. J Pharm Pharm Sci, 23: 75-85.
Tibullo L, Esquinas A (2019) Outcomes difference in non-invasive ventilation in 'very old' patients with acute respiratory failure: occult gender effect? Emerg Med J, 36: 514.
Valentin A, Jordan B, Lang T et al. (2003) Gender-related differences in intensive care: a multiple-center cohort study of therapeutic interventions and outcome in critically ill patients. Crit Care Med, 31: 1901-1907.
Wernly B, Bruno RR, Mamandipoor B et al. (2020a) Sex-specific outcomes and management in critically ill septic patients. Eur J Intern Med.
Wernly B, Bruno RR, Kelm M et al. (2020b) Sex-specific outcome disparities in very old patients admitted to intensive care medicine: a propensity matched analysis. Sci Rep, 10: 18671.












