ICU Management & Practice, Volume 21 - Issue 3, 2021
Introduction
Tracheal intubation in critically ill patients is among the most commonly performed and high-risk procedures (Russotto et al. 2019). Until now, information on peri-intubation adverse events was limited to data from single-centre, national level or retrospective studies.
In 2018 we launched the INTUBE study, a large international prospective observational study aiming at collecting data on peri-intubation adverse events in critically ill patients. In this third anniversary update we are pleased to describe our journey and our findings from the primary analysis recently published in JAMA (Russotto et al. 2021).
In INTUBE study, we enrolled critically ill patients undergoing in-hospital tracheal intubation. Each site collected data on a series of consecutive intubations in critically ill patients performed in ICU, emergency department and wards. In this regard, INTUBE study is unique in focusing on critical illness rather than on the procedure location.
We excluded patients undergoing intubation to receive general anaesthesia, patients intubated during cardiopulmonary resuscitation for cardiac arrest and out-of-hospital intubation. One hundred ninety-seven centres from 29 countries across five continents joined the INTUBE family, making this the first study providing data not only from Europe, US and Australia but also from Asia, South America and Africa. A total of 2964 patients were finally enrolled. The primary reason for intubation was respiratory failure in 52.3% of patients, followed by neurological impairment in 30.5% and cardiovascular instability in 9.4%. The primary outcome of the study was the composite of cardiovascular instability, severe hypoxaemia and cardiac arrest. Secondary outcomes included incidence of aspiration of gastric contents, difficult intubation, airway injuries and ICU mortality.
Key Findings and Discussion
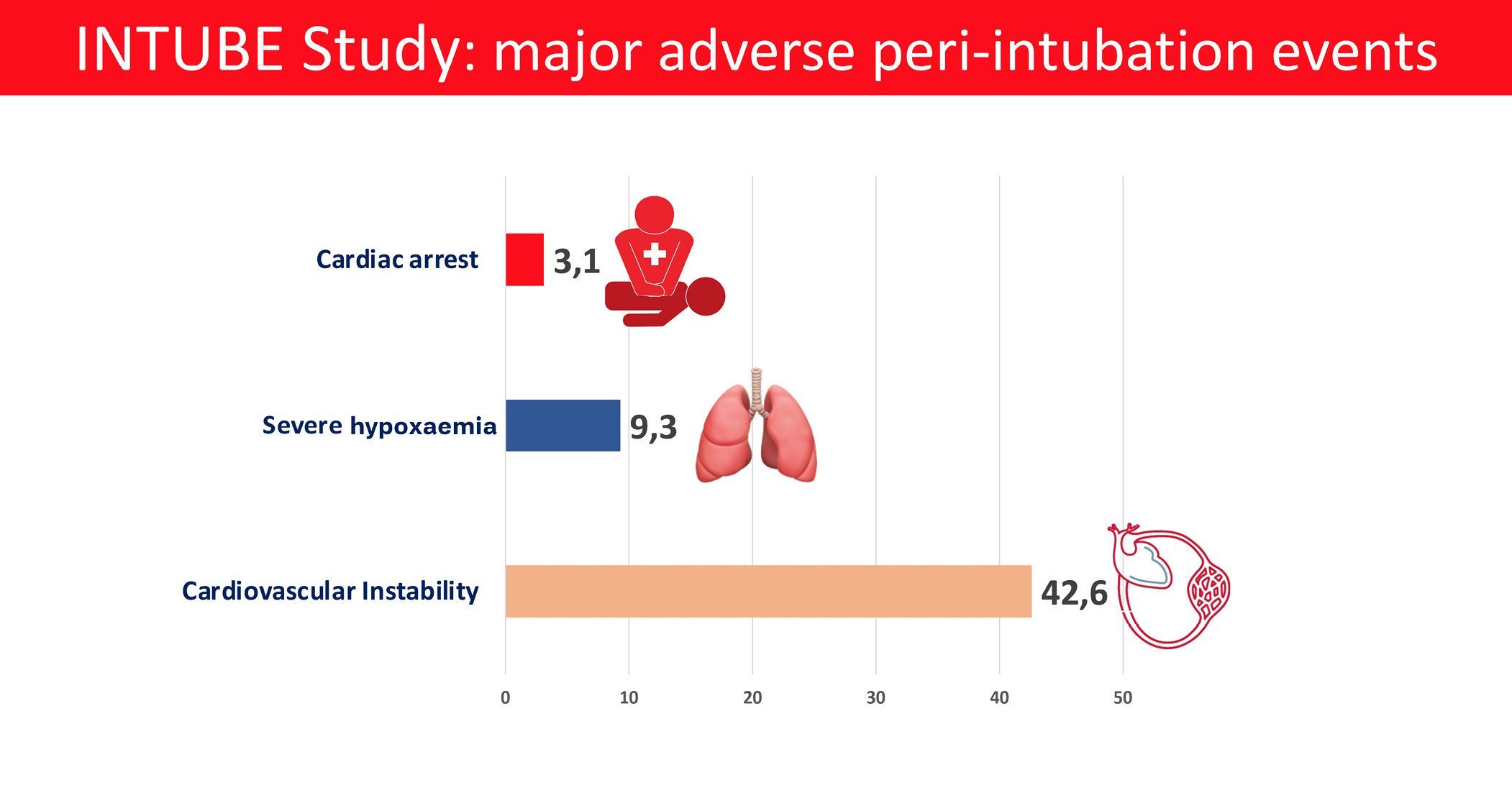
Among the study patients, 45.2% experienced at least one major adverse peri-intubation event. The predominant event was cardiovascular instability, observed in 42.6% of patients. Severe hypoxaemia and cardiac arrest were observed in 9.3% and 3.1% of patients respectively. First-pass intubation success was achieved in approximately 80% of patients, a second attempted intubation was necessary for 16%, while 4% of patients required more than two attempts. First pass intubation failure was associated with an increased risk of adverse events.
Patients experiencing major adverse events were at higher risk of both ICU (adjusted OR 1.52, 95% CI 1.26 – 1.83) and 28-day mortality (adjusted OR 1.44, 95% CI 1.19 – 1.74) after adjustment for underlying disease severity.
Important information has emerged from the description of the intubation procedure. The leading preoxygenation method was bag-valve mask, used in approximately 60% of patients, while noninvasive ventilation was used in only 12% of patients and continuous positive airway pressure in approximately 2% of patients. High-flow nasal cannula were used in approximately 5% of patients. Moreover, apnoeic oxygenation was seldom used (10% of patients).
The “haemodynamically friendly” agents ketamine and etomidate were used in 14% and 18% of patients respectively, while propofol, used in 40% of patients, represented the most frequently used induction agent. When administered to patients with underlying haemodynamic instability, propofol was associated with a significantly higher incidence of cardiovascular collapse compared to etomidate.
Videolaryngoscopy has been used as a first-choice method in 17% of patients, in most cases when an anticipated difficult airway was detected.
Another striking observation was the use of waveform capnography as elective method to confirm successful intubation in only 25.6% of overall patients. In 70% patients who had undergone oesophageal intubation, capnography was not used. Although the study was not able to detect a direct association between the waveform capnography underuse and patients’ related outcomes, this observation is of concern. Indeed, it came after 10 years from the publication of the National Audit Project 4 in UK which reported how the majority of catastrophic airway adverse events were associated with either an underuse or misinterpretation of capnography (Cook et al. 2011). The INTUBE study highlights how many recently investigated interventions (e.g., noninvasive ventilation for preoxygenation, apnoeic oxygenation, videolaryngoscopy), are poorly applied in daily clinical practice.
Conclusion
The INTUBE study highlights the high number of major adverse events associated with intubation of critically ill patients. The finding that cardiovascular instability constitutes the leading adverse event underlines the need for future research to optimise peri-intubation haemodynamics to make tracheal intubation in the critically ill a safer procedure.
Conflict of Interest
None.
Key Points
- Tracheal intubation in critically ill patients is among the most commonly performed and high-risk procedures.
- The INTUBE study enrolled critically ill patients undergoing in-hospital tracheal intubation.
- INTUBE study is unique in focusing on critical illness rather than on the procedure location.
- The INTUBE study highlights the high number of major adverse events associated with intubation of critically ill patients.
- Cardiovascular instability constitutes the leading adverse event.
References:
Cook TM, Woodall N, Harper J, Benger J; Fourth National Audit Project. (2011) Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society, II: intensive care and emergency departments. Br J Anaesth., 106(5):632-642. doi:10.1093/bja/aer059
Russotto V, Myatra SN, Laffey JG (2019) What’s new in airway management of the critically ill. Intensive Care Med., 2019;45(11):1615-1618. doi:10.1007/s00134-019-05757-0
Russotto V, Nainan Myatra S, Laffey JG et al. (2021) Intubation practices and adverse peri-intubation events in critically ill patients from 29 countries. JAMA. 325(12):1164-1172. doi:10.1001/jama.2021.1727










