ICU Management & Practice, Volume 21 - Issue 1, 2021
Introduction
Patients admitted to Intensive Care Units (ICU) often require respiratory support. Orotracheal intubation is one of the most frequent procedures performed in ICU (Lascarrou et al. 2017; Roux et al. 2014; Martin et al. 2020).When performed in critically ill patients, intubation is a challenging issue as it may be associated with life-threatening complications in up to one third of cases (Jaber et al. 2006; De Jong et al. 2013b). Severe hypoxaemia occurring during intubation procedure can result in cardiac arrest (Mort 2004; De Jong et al. 2018), cerebral anoxia, and death (Cook et al. 2010). Difficult intubation is known to be associated with life-threatening complications (De Jong et al. 2013b; De Jong et al. 2014a; Jaber et al. 2006; Jaber et al. 2010; Martin et al. 2011; Driver et al. 2018).The failure of first-attempt intubation appears a major factor for developing life-threatening complications related to intubation (De Jong et al. 2020).
In this setting, the place of videolaryngoscopy for intubation procedure in critically ill patients remains debated in the past years (Jaber et al. 2019; Mosier et al. 2020). However, the recent COVID-19 pandemic highlighted the potential usefulness of videolaryngoscopy to reduce intubation provider contamination (El-Boghdadly et al. 2020; Cook et al. 2020; Patwa et al. 2020). Is videolaryngoscopy the new gold standard for intubation during and after the COVID-19 crisis?
What are the Videolaryngoscopes?
Videolaryngoscopes were first proposed to improve airway management through improved glottis visualisation, aiming to reduce incidence of difficult intubation in the operating room. Then, their use was extended to airway management in other settings. These devices contain a miniaturised camera aimed at the tip of the blade to indirectly visualise the glottis.
Videolaryngoscopes differ in design, blade type and technical configuration. Three main categories of videolaryngoscopes exist according to the type of blade. First, the Macintosh blade-shaped optical laryngoscopes have Macintosh blades combined with video technology. The glottis can be seen either directly or via a video screen. Second, the anatomically shaped blades without a tube guide have anatomically shaped, giving a view of the glottis without the need to flex or extend the neck, providing only an indirect view of the glottis, with the need to use a preshaped stylet into the tracheal tube. Third, the anatomically shaped blade with a tube guide do not necessitate a preshaped stylet.
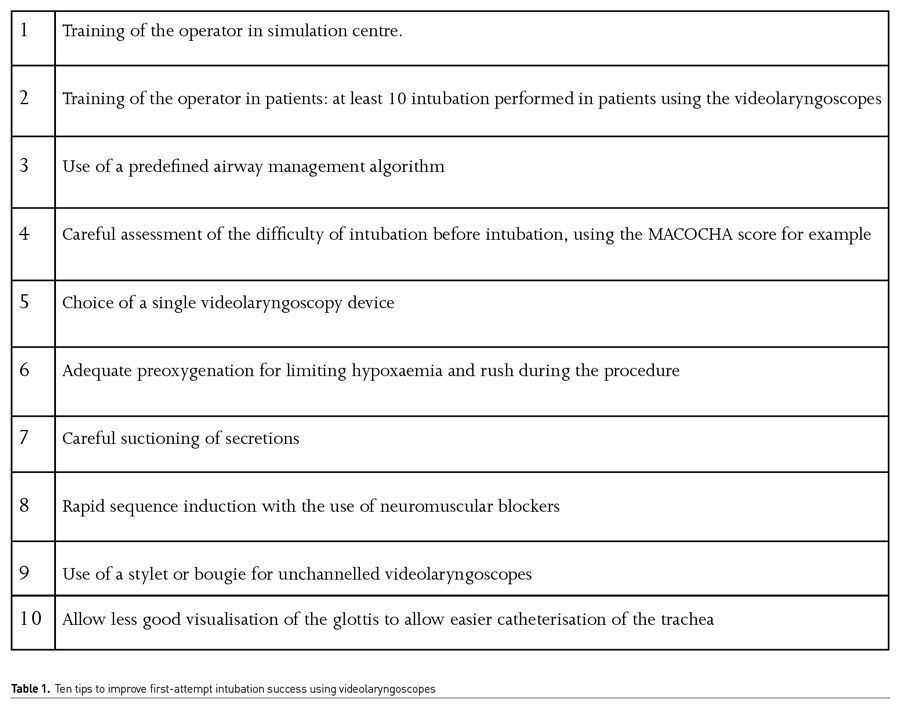
Despite the better visualisation of the glottis, the main challenge when using videolaryngoscopes remains to insert the tube into the trachea. In other terms, achieving a 100% percentage of glottis opening (POGO) view (corresponding to a Cormack-Lehane grade 1 in direct laryngoscopy) during videolaryngoscopy does not guarantee successful intubation, as the tube has to pass a sharp angle to enter the larynx. Table 1 presents ten tips to improve first-attempt intubation success using videolaryngoscopes.
What are the Data in Literature?
In the ICU setting in the 2010’s, it has been suggested that videolaryngoscopes could help to reduce difficult intubation rate (Kory et al. 2013; Lakticova et al. 2013). In a before-after study reporting a quality improvement process using a videolaryngoscope in an airway management algorithm (De Jong et al. 2013a), the systematic use of a combo videolaryngoscope for intubation significantly reduced the incidence of difficult intubation and/or difficult laryngoscopy (De Jong et al. 2013a). In the multivariate analysis, the "standard laryngoscopy" group was an independent risk factor for difficult intubation and/or difficult laryngoscopy. In addition, in the subgroup of patients with difficult intubation predicted by the MACOCHA score (De Jong et al. 2013b), the incidence of difficult intubation was much higher in the "standard laryngoscopy" group (47%) than in the "combo videolaryngoscope" group (0%).
These results were confirmed in 2014 by a systematic review and meta-analysis establishing that use of videolaryngoscopes for intubation in ICU could reduce the rate of difficult intubation (De Jong et al. 2014b). Videolaryngoscopy improved difficult intubation, first-attempt success, Cormack 3/4 grades, oesophageal intubation, and did not modify severe hypoxaemia, severe cardiovascular collapse, and airway injury, when compared with direct laryngoscopy. However, in 2016, Lascarrou et al. (2017) showed in a large multicentre randomised controlled trial that videolaryngoscopy compared with direct laryngoscopy did not improve first-pass orotracheal intubation rates and was associated with higher rates of severe life-threatening complications.
Several meta-analyses (Arulkumaran et al. 2018; Zhao et al. 2017; Huang et al. 2017) were then published, with conflicting results regarding the superiority of the videolaryngoscopes over direct laryngoscopy for intubation in critically ill patients. The disparities between included trials were however considerable, with high heterogeneity.
A prospective observational study that compares the use of direct laryngoscopy with a conventional Macintosh blade to the C-MAC® videolaryngoscope (Karl-Storz) (Dey et al. 2020), among operators that had performed, at least, 50 intubations in clinical simulation with the videolaryngoscope, was recently performed. In the videolaryngoscope group, there was a higher first-attempt intubation rate than in the conventional Macintosh blade group.
What May Explain the Discrepancies in Literature?
One of the most important point is the use of a stylet to preshape the endotracheal tube, described in Figure 1. In the study of Lascarrou et al.( 2017), it was used in less than 20% of cases. Using a preshaped endotracheal tube with a stylet may have potential advantages over conventional endotracheal tube and can help to increase success of intubation using videolaryngoscopy (Apfelbaum et al. 2013; Jaber et al. 2020; Sorbello and Hodzovic 2020).
The expertise of operators is also very important when assessing the results of published observational and randomised studies. In the study of Lascarrou et al. (2017), it is worth noting that more than 80% of the operators were non-expert. The experience required to attain 90% probability of optimal performance with videolaryngoscopes has been evaluated (Cortellazzi et al. 2015). At least 75 attempts with videolaryngoscopes were required to achieve that level of proficiency (Cortellazzi et al. 2015).
A team recently implemented the McGrath MAC videolaryngoscope (Medtronic) as part of a quality improvement initiative (Amalric et al. 2020). They positioned the videolaryngoscope as the first-line laryngoscope for every intubation in critically ill patients to reinforce skill training. In the multivariate analysis, the absence of dedicated videolaryngoscopy expertise, junior status, and the presence of coma were independent risk factors of first-attempt failure. They reported for the first time in the critically ill that specific videolaryngoscopy skill training, assessed by the number of previous videolaryngoscopies performed, was an independent factor of first-attempt intubation success. There was an increase of the first-attempt procedure success rate according to the operators’ level of expertise. Having performed more than 15 videolaryngoscopies was associated with a first-pass success rate of 87%.
That is why training and education are essential, through clinical simulation and practice with cadaveric specimens, to secure the implementation of these new techniques in critically ill patients.
What were the Expert Positions Before the COVID-19 Pandemic?
The clinical practice guidelines for the management of the critically ill patient’s difficult airway published by the Difficult Airway Society (DAS) in 2018 (Higgs et al. 2018) suggest the use of videolaryngoscopes in the presence of a difficult airway or as a rescue strategy when the direct laryngoscope has failed. Similarly, the expert guidelines on intubation and extubation in intensive care from the Société Francaised’ Anesthésie et de Réanimation (SFAR) and the Société de Réanimation de Langue Francaise (SRLF) published in 2017 (Quintard et al. 2017) have included the videolaryngoscope in the algorithm for the airway management as the first option in the intubation of patients who score ≥ 3 in the MACOCHA score (De Jong et al. 2013b), and as the rescue strategy when intubation with the direct laryngoscopy fails.
What are the Expert Positions During the COVID-19 Pandemic?
The COVID-19 pandemic has further highlighted the place of videolaryngoscopy during intubation in ICU, in order to limit the contamination of the intubating provider. International guidelines recommend using video laryngoscopy where available to increase the distance between the patient and intubating provider, and to perform intubation by the most experienced operator (Cook et al. 2020; Patwa et al. 2020). If using a bougie or a stylet, the operator is advised to be careful when removing it so as not to spray secretions on the intubating team (Cook et al. 2020).
What About the Future of Videolaryngoscopy in the ICU?
Future trials will better define the role of videolaryngoscopy in ICU, especially with respect to appropriate use of airway adjuncts as stylets. First pass intubation success rate alone has demonstrated to be an accurate primary outcome, strongly associated with the occurrence of complications during intubation procedure (De Jong et al. 2020). The expertise of operator will be a major confounding factor to take into account when designing future randomised clinical trials.
Conclusion
Videolaryngoscopy in critically ill patients should be widely used, after appropriate formation and training of intubator providers. Further studies are still needed before being able to perform recommendations to implement videolaryngoscopy for first-attempt intubation of ICU patients.
Conflict of interest
Dr De Jong reports receiving consulting fees from Medtronic. Pr. Jaber reports receiving consulting fees from Drager, Medtronic, Baxter, Fresenius-Xenios, and Fisher & Paykel. Dr Aarab has no conflict of interest.
References:
Amalric M, Larcher R, Brunot V et al. (2020) Impact of Videolaryngoscopy Expertise on First-Attempt Intubation Success in Critically Ill Patients. Crit Care Med, 48, E889-E896.
Apfelbaum JL, Hagberg CA, Caplan RA et al. (2013) Practice Guidelines for Management of the Difficult Airway: An Updated Report by the American Society Of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology, 118, 251-270.
Arulkumaran N, Lowe J, Ions R et al. (2018) Videolaryngoscopy Versus Direct Laryngoscopy for Emergency Orotracheal Intubation Outside the Operating Room: A Systematic Review and Meta-Analysis. Br J Anaesth., 120:712-724.
Cook TM, El-Boghdadly K, Mcguire B et al. (2020) Consensus Guidelines for Managing the Airway in Patients With COVID-19: Guidelines From The Difficult Airway Society, The Association of Anaesthetists the Intensive Care Society, The Faculty of Intensive Care Medicine and the Royal College of Anaesthetists. Anaesthesia, 75:785-799.
Cook TM, Scott S Mihai R (2010) Litigation Related to Airway and Respiratory Complications of Anaesthesia: An Analysis of Claims Against the NHS in England 1995-2007. Anaesthesia, 65:556-63.
Cortellazzi P, Caldiroli D, Byrne A et al. (2015) Defining and Developing Expertise in Tracheal Intubation Using a Glidescope ((R)) for Anaesthetists With Expertise in Macintosh Direct Laryngoscopy: An In-Vivo Longitudinal Study. Anaesthesia, 70:290-5.
De Jong A, Clavieras N, Conseil M et al. (2013a) Implementation of a Combo Videolaryngoscope for Intubation in Critically Ill Patients: A Before-After Comparative Study. Intensive Care Medicine, 39:2144-52.
De Jong A, Jung B, Jaber S (2014a) Intubation In The ICU: We Could Improve our Practice. Crit Care, 18:209.
De Jong A, Molinari N, Conseil M et al. (2014b) Video Laryngoscopy Versus Direct Laryngoscopy for Orotracheal Intubation in the Intensive Care Unit: A Systematic Review and Meta-Analysis. Intensive Care Medicine, 40:629-39.
De Jong A, Molinari N, Terzi N et al. (2013b) Early Identification of Patients at Risk for Difficult Intubation in the Intensive Care Unit: Development and Validation of the Macocha Score in a Multicenter Cohort Study. Am J Respir Crit Care Med., 187:832-9.
De Jong A, Rolle A, Molinari, N et al. (2018) Cardiac Arrest and Mortality Related to Intubation Procedure in Critically Ill Adult Patients: A Multicenter Cohort Study. Crit Care Med, 46, 532-539.
De Jong A, Rolle A, Pensier J et al. (2020) First-attempt success is associated with fewer complications related to intubation in the intensive care unit. Intensive Care Med, 46, 1278-1280.
Dey S, Pradhan D, Saikia P et al. (2020) Intubation in the Intensive Care Unit: C-MAC video laryngoscope versus Macintosh laryngoscope. Med Intensiva, 44, 135-141.
Driver BE, Prekker ME, Klein LR et al. (2018) Effect of Use of a Bougie vs Endotracheal Tube and Stylet on First-Attempt Intubation Success Among Patients With Difficult Airways Undergoing Emergency Intubation: A Randomized Clinical Trial. JAMA, 319, 2179-2189.
El-Boghdadly K, Wong DJN, Owen R et al. 2020. Risks to healthcare workers following tracheal intubation of patients with COVID-19: a prospective international multicentre cohort study. Anaesthesia, 75, 1437-1447.
Higgs A, McGrath BA, Goddard C et al. (2018) Guidelines for the management of tracheal intubation in critically ill adults. Br J Anaesth, 120, 323-352.
Huang HB, Peng JM, Xu B et al. (2017) Video Laryngoscopy for Endotracheal Intubation of Critically Ill Adults: A Systemic Review and Meta-analysis. Chest.
Jaber S, Amraoui J, Lefrant JY et al. (2006) Clinical practice and risk factors for immediate complications of endotracheal intubation in the intensive care unit: a prospective, multiple-center study. Critical care medicine, 34, 2355-2361.
Jaber S, De Jong A, Pelosi P et al. (2019) Videolaryngoscopy in critically ill patients. Crit Care, 23, 221.
Jaber S, Jung B, Corne P et al. (2010) An intervention to decrease complications related to endotracheal intubation in the intensive care unit: a prospective, multiple-center study. Intensive care medicine, 36, 248-255.
Lascarrou JB et al. (2017) Video Laryngoscopy vs Direct Laryngoscopy on Successful First-Pass Orotracheal Intubation Among ICU Patients: A Randomized Clinical Trial. Jama, 317, 483-493.
Martin LD et al. (2011) 3,423 emergency tracheal intubations at a university hospital: airway outcomes and complications. Anesthesiology, 114, 42-48.
Martin M et al. (2020) Nationwide survey on training and device utilization during tracheal intubation in French intensive care units. Ann Intensive Care, 10:2.
Patwa A et al. (2020) All India difficult airway association (AIDAA) consensus guidelines for airway management in the operating room during the COVID-19 pandemic. Indian J Anaesth, 64:S107-s115.
Quintard H et al. (2017) Intubation and extubation of the ICU patient. Anaesth Crit Care Pain Med, 36:327-341.
Roux D et al. (2014) Acquiring procedural skills in ICUs: a prospective multicenter study*. Crit Care Med, 42:886-95.
Sorbello M, Hodzovic I (2020) Tracheal Tube Introducers (Bougies), Stylets and Airway Exchange Catheters. In: Kristensen MS & Cook T (eds.) Core Topics in Airway Management. 3 ed. Cambridge: Cambridge University Press.
Zhao BC et al. (2017) Video laryngoscopy for ICU intubation: a meta-analysis of randomised trials. Intensive Care Med, 43 :947-948.









