ICU Management & Practice, Volume 21 - Issue 2, 2021
An overview of the potential of POCUS on clinical decision making at the bedside and the need to add it as a new diagnostic tool by intensive care physiotherapists.
Introduction
Intensive care physiotherapists often rely on standard assessment tools, such as measures of physiological function (arterial blood gases), adequacy/quality of lung aeration through lung auscultation and the portable chest radiograph to guide clinical decision making at the bedside (Hanekom et al. 2007). However, the reduced diagnostic accuracy of the chest radiograph and lung auscultation when compared with lung ultrasound (Xirouchaki et al. 2011; Hansell et al. 2021) may have significant impact on physiotherapists clinical decision making at the bedside (Xirouchaki et al. 2014), which must be addressed. The main reasons to add point-of-care ultrasound (POCUS) as a new diagnostic tool to the standard assessment by intensive care physiotherapists include the increasing evidence-base for its excellent diagnostic accuracy and real-time bedside non-invasive monitoring capabilities (Via et al. 2012; Volpicelli et al. 2012).
Relevance of POCUS to Physiotherapists for Clinical Decision Making in Chest Physiotherapy
The chest radiograph is commonly used to both identify lobar collapse and establish the response to therapeutic interventions. The chest radiographic resolution of acute lobar collapse to intensive care physiotherapy ranges from 60% when the physiotherapy intervention includes patient re-positioning (collapsed lobe uppermost), airway suctioning and manual lung hyperinflation compared with only 8% resolution when the physiotherapy intervention includes manual lung hyperinflation and airway suctioning (Stilleret al. 1990; Stiller 1996; Stiller 2013). We however, propose that before we can select the most appropriate physiotherapy interventions, we must select the most appropriate diagnostic pathologies for therapeutic intervention. The reduced diagnostic accuracy of the chest radiograph to detect lobar collapse/consolidation compared to the gold standard of CT scan (Xirouchaki et al. 2011; Hansell et al. 2021), indicates that these earlier intensive care physiotherapy trials (Stiller 1996) may have included patients with other conditions such as pleural effusions, not expected to respond to intensive care physiotherapy. Hence, physiotherapists use of a less than optimal diagnostic tool may lead to ineffective and or inappropriate chest physiotherapy treatments (Templeton and Palazzo 2007; Patman et al. 2009; Leech et al. 2015).
Another issue that clinicians face is that the routine daily chest radiograph may no longer be the norm for intensive care, with on-demand imaging becoming a more common strategy (Lakhal et al. 2012). Hence, unless the acute lobar collapse causes clinical deterioration (e.g. arterial desaturation) then a chest radiograph may not be ordered and remain undetected. But more importantly, as the portable chest radiograph is less accurate than point of care lung ultrasound for the detection of lung collapse/consolidation, pleural effusion, pulmonary oedema or pneumothorax (Xirouchaki et al. 2011), clinicians need to address this challenge.
POCUS shows high diagnostic accuracy for detecting pulmonary oedema with a sensitivity and specificity of 88% and 90%, respectively (Maw et al. 2019). In patients with acute respiratory failure, POCUS has a sensitivity and specificity ranging from 91 to 100% and 78 to 100%, respectively, to detect lung consolidation (Hew et al. 2015). For diagnosing pleural effusion and pneumothorax, accuracy of lung ultrasound is over 90% and 98%, in terms of sensitivity and specificity, respectively (Alrajhi et al. 2012; Yousefifard et al. 2016). So, POCUS should be of great interest to the physiotherapist to rule in pulmonary conditions which may benefit from chest physiotherapy (e.g. lung consolidation) or rule out non-indication or contra-indication for chest physiotherapy (e.g. pleural effusion, pneumothorax).
POCUS is also useful for the evaluation of diaphragmatic function and mechanical ventilation weaning suitability (Zambon et al. 2013). The physiotherapist could use diaphragm ultrasound to detect diaphragm dysfunction during the spontaneous breathing trials which may be predictive of extubation failure (Le Neindre et al. 2021). Interventions such as inspiratory muscle training (IMT) improve not only inspiratory muscle strength but may also reduce weaning time from mechanical ventilation (Elkins and Dentice 2015; Bissett et al. 2016; Vorona et al. 2018; Ahmed et al. 2019; Worraphan et al. 2020). Hence, diaphragmatic ultrasound could be used for the assessment of the effects of IMT (Dres et al. 2017).
The assessment of the chest physiotherapy efficacy is challenging, and POCUS may provide useful information on the patient’s response to therapeutic interventions and is indeed the purpose of a current trial (http://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=376222).
Indeed, as POCUS is a repeatable, non-invasive and radiation-free tool it allows a real time assessment of therapies which aim to improve alveolar recruitment. Previous studies have demonstrated the capacity of POCUS to detect changes in lung aeration during alveolar recruitment by positive-end expiratory pressure, antibiotic therapy or haemodialysis (Bouhemad et al. 2010; Bouhemad et al. 2011; Noble et al. 2009). Hence, we should be able to extrapolate that POCUS could assist the physiotherapist to monitor the impact of a chest physiotherapy intervention on lung recruitment (Cavaliere et al. 2011).
Not surprisingly, physiotherapists now advocate for the use of POCUS (Le Neindre et al. 2016; Hansell et al. 2021), especially to guide physiotherapy clinical decision making (Leech et al. 2015; Hayward and Janssen 2018; Hayward et al. 2020; Vieira et al. 2020).
Further Perspectives
The challenge we face is to try to incorporate new potentially more accurate and appropriate diagnostic tools into our clinical and research practice. A current international trial by Le Neindre et al.
(https://clinicaltrials.gov/ct2/show/NCT02881814) may provide guidance and impetus for physiotherapists to incorporate POCUS into clinical decision making for respiratory physiotherapy in intensive care. However, one of the key issues that must be addressed is how we best define and deliver the optimal training programmes to skill physiotherapists to become competent in POCUS (Tutino et al. 2010; Cuca et al. 2013; Hulett et al. 2014; Greenstein et al. 2017; Williamson et al. 2017; Arbelot et al. 2020). There are many other current issues around the role of physiotherapy within critical care (Ntoumenopoulos et al. 2018) (e.g. 24/7 access, respiratory versus rehabilitation focus, limited physiotherapy staffing to patient ratios, skill-mix), and hence it will be a challenge for our clinicians to feasibly incorporate another diagnostic tool with busy clinical caseloads. However, with POCUS, we have the potential for the more accurate diagnoses of conditions such as lung collapse/consolidation (as distinct from pleural effusions), to enable the more appropriate delivery of interventions and monitoring the response to therapy. This may allow physiotherapists to prioritise patients with indications for chest physiotherapy, and reduce less appropriate interventions which are time-consuming and have the potential for patient harm (Leech et al. 2015). Such tools will also enable us to determine the prevalence of acute pulmonary conditions such as lobar collapse and an understanding of its potential impact on patient outcome, in addition to the role of physiotherapy. This should expand our understanding of the pulmonary conditions that may optimally be managed through physiotherapy and hence question some of the current evidence-based recommendations (Stiller 2013).
Case Report Summary
Here we detail a case report managed in intensive care to highlight the limitations of utilising standard assessment tools such as the portable chest radiograph for physiotherapy and medical clinical decision making.
This subject, a 48-year-old male (170 cm, weight 73 kg, BMI 25.25), underwent a heart and lung transplant via median sternotomy. The subject’s admission APACHE II score was 7 and relevant past medical history included severe congenital cardiac disease, with a ventricular septal defect, severe pulmonary hypertension and atrial fibrillation, complicated by a recent cerebrovascular accident with limited residual limb weakness. The subject's total intensive care length of stay was 61 days, comprising of invasive mechanical ventilation for 8.2 days and 13 hours of non-invasive ventilation. During the ICU stay, the subject required a total of 88 sessions of physiotherapy that predominantly included chest physiotherapy such as postural drainage, manual chest wall techniques, airway suctioning, saline lavage (during intubation and mechanical ventilation) and once the patient was extubated frequent multiple nasopharyngeal suctioning interventions were required due to weak ineffective coughing. The subject’s total hospital length of stay was 114 days.
Considering the prolonged ICU-stay requiring intensive daily physiotherapy, for the purposes of this manuscript we have selected key clinical events (day after surgery) and two key physiotherapy assessments/interventions (out of the total of 88 physiotherapy interventions), that highlight the role of POCUS and clinical decision making by physiotherapy and the medical team.
Physiotherapy assessment/intervention day after surgery (intubated and ventilated)
The day after heart-lung transplantation the chest radiograph was reported by radiology (Figure 1) as peri-hilar airspace opacification and minor blunting of left costophrenic angle which may represent a small effusion.
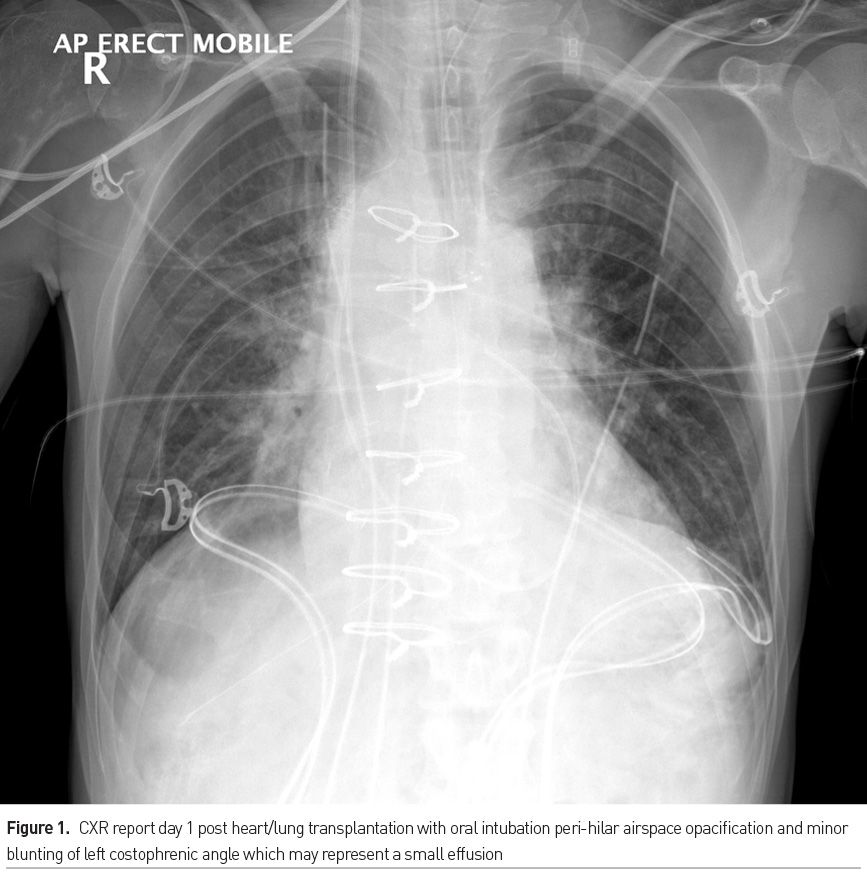
However, the POCUS examination indicated due to hypoxaemia was undertaken by the physiotherapist on the same day after surgery (https://www.youtube.com/watch?v=nm0AWms9_EM) and demonstrated significant right lower lobe consolidation (tissue-like pattern arising from the visceral pleura with complete lobar consolidation, hyperechoic areas within the consolidation indicative of air bronchograms and anechoic linear forms surrounding by hyperechoic lines suggestive of fluid bronchograms). These POCUS findings were not in keeping with the chest radiograph findings and influenced the physiotherapist to provide more aggressive patient re-positioning into left side-lying and manual chest physiotherapy techniques and endotracheal airway suctioning to assist secretion clearance.
The subject was extubated 4 days after surgery but required reintubation after 10 hours due to respiratory failure and secretion retention. The subject then remained on mechanical ventilation for further 4 days and was then successfully re-extubated.
Physiotherapy assessment/interventions after endotracheal extubation
Three days after the successful second extubation (11 days after surgery), the physiotherapist reported on clinical examination with lung auscultation the subject had good breath sounds throughout associated with fine inspiratory crackles in the lower lobes. The chest radiograph was reported by radiology as minor bilateral lower lobe atelectasis (Figure 2). The subject also reported significant physical fatigue associated with haemodialysis leading to increased difficulty clearing airway secretions. The subject also required high flow oxygen therapy via nasal prongs (FiO2 0.3 at 40 Lpm).
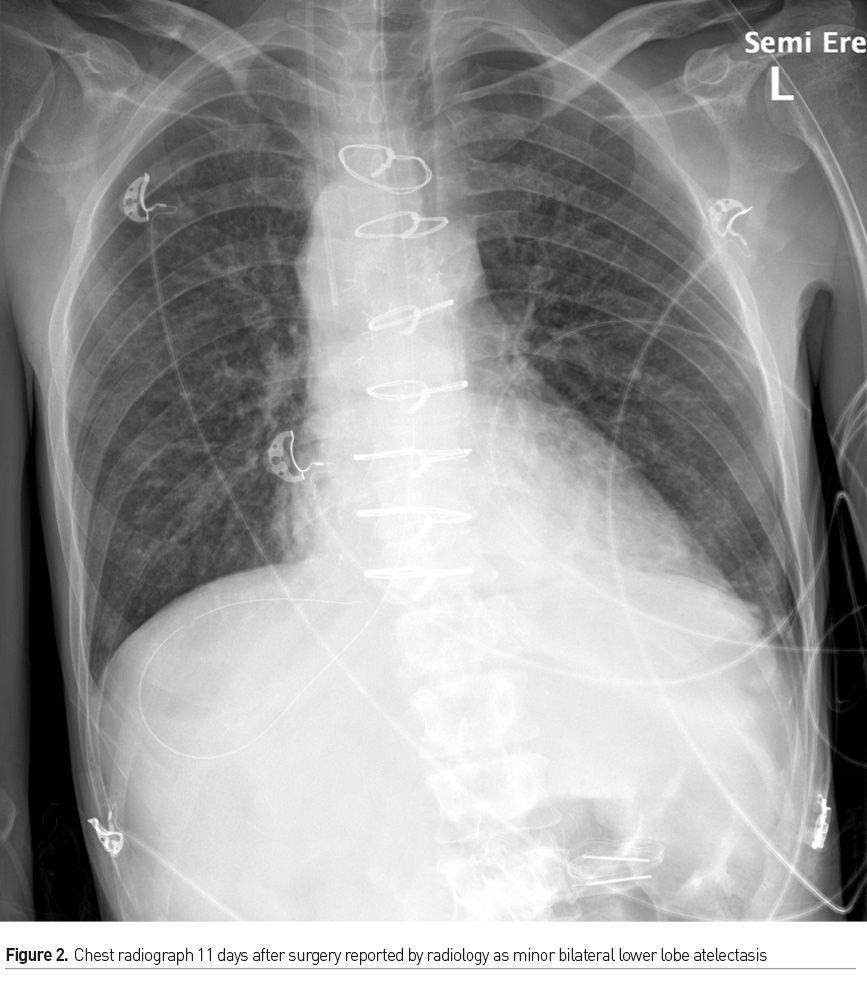
The POCUS examination on the same day 11 days after surgery however demonstrated dense left lower lobe hypoechoic consolidation (https://www.youtube.com/watch?v=JrH7pf5n3UQ) with complex effusion with swirling hyperechoic particulate matter noted during respiration. The physiotherapists on this same day provided four chest physiotherapy interventions including nasopharyngeal airway suctioning during the day up to the early evening (1900 hrs, late shift) due to concerns with secretion retention presumably as a result of the dense left lower lobe consolidation evident on the POCUS examination and weak ineffective cough, with the nasopharyngeal suctioning productive of large volumes of tenacious secretions.
Nineteen days after surgery the subject was reviewed by physiotherapy during the haemodialysis session (out of the ICU), due to concerns about secretion retention and an ongoing respiratory review with the chest radiograph on this day (Figure 3) radiology report as small bilateral effusions.
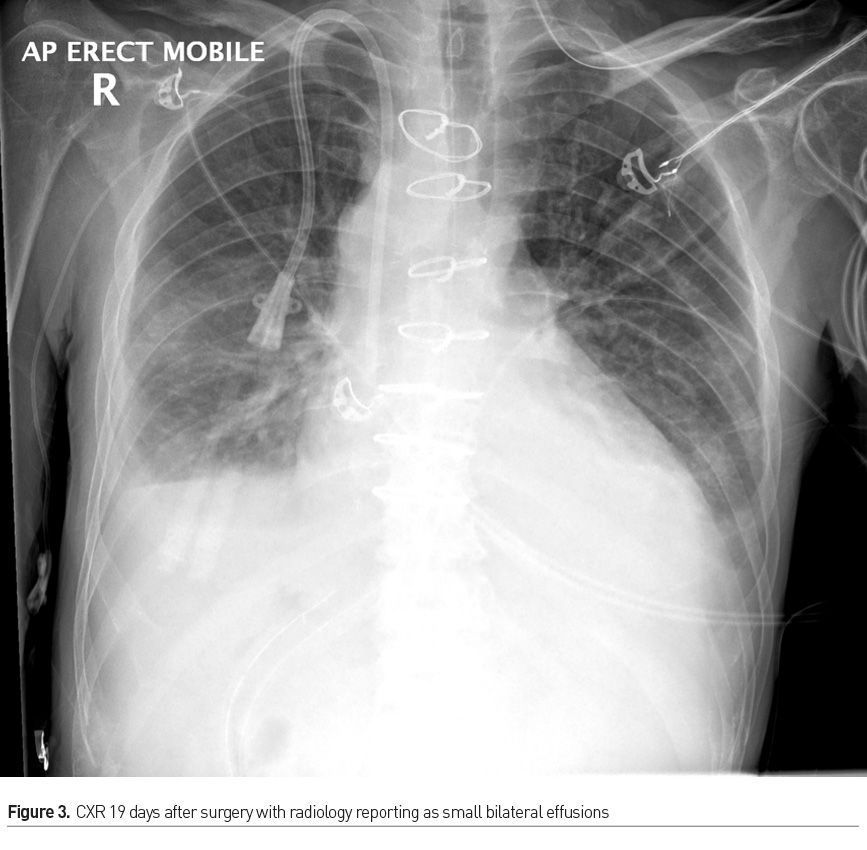
POCUS was undertaken by the physiotherapist during this assessment on day 19 after surgery and they had identified moderate to large sized anechoic bilateral pleural effusions that approximated 4 cm in transverse depth (https://www.youtube.com/watch?v=mQnj1xFtixs; https://www.youtube.com/watch?v=D9Aqhj3uYFE). The physiotherapy treatment required at this stage still included nasopharyngeal suctioning that was productive of moderate creamy purulent secretions and the ICU medical team was updated about these POCUS findings of pleural effusions.
On day 21 after surgery the ICU team ordered a CT scan of the thorax (Figure 4) which had confirmed the POCUS findings of pleural effusions on day 19 after surgery (https://www.youtube.com/watch?v=mQnj1xFtixs; https://www.youtube.com/watch?v=D9Aqhj3uYFE). The following day on day 22 after surgery, bilateral chest drains were inserted by the medical team for the drainage of these pleural effusions.

In summary, the physiotherapist-initiated POCUS assessments led to changes in physiotherapy management leading to more aggressive chest physiotherapy intervention, especially on the findings on Day 1 and 11 after surgery where the ultrasound demonstrated dense right (Day 1) and left lower lobe (Day 11) consolidation, which did not concur with the same day chest radiograph findings. In addition, physiotherapist-initiated POCUS identified significant pleural effusions (later confirmed by CT scan) that resulted in a change of medical management. Of note also vocal cord dysfunction was identified by both laryngeal ultrasound (Fukuhara et al. 2018) performed by the physiotherapist that concurred with the simultaneous fibreoptic endoscopic evaluation of speech by the speech and language pathologist on Day 43 after surgery. We surmised that the vocal cord dysfunction (severe loss of sensation of vocal cords) may have facilitated the passage of the nasopharyngeal suction catheter past the vocal cords for secretion clearance by physiotherapy.
For POCUS to be adopted by physiotherapists within intensive care (Ntoumenopoulos and Hough 2014), there are a few challenges ahead. Current international recommendations for training in point of care ultrasound, advocate a combination of theory with mentored bedside training (Volpicelli et al. 2012). A recent study reported that in addition to preliminary theory and practical based training, at least 25 lung ultrasound examinations supervised by an expert are required for novice clinicians (including non-physicians) to acquire the basic skills for diagnosing normal lung aeration, interstitial-alveolar syndrome, and consolidation in emergency and critically ill patients (Arbelot et al. 2020).
Beyond the potential for POCUS to discern whether chest physiotherapy is indicated, it may also be of use to non-invasively assess the effect of the interventions, such as patient re-positioning, manual or ventilator hyperinflation to recruit collapsed lung (Cavaliere et al. 2011), rather than patients having to undergo repeated exposures to radiation with sub-standard diagnostic tools such as the chest radiograph. The challenges to be faced include the provision of adequate training, mentoring and support from experienced mentors for physiotherapists to acquire POCUS skills. Support from the wider multidisciplinary teams within ICU may be an ideal means to initiate this kind of support. Further research must also identify the impact of POCUS on physiotherapists clinical decision making, the ability of POCUS to determine the effect of the various physiotherapy interventions on lung re-aeration and weaning from mechanical ventilation if clinicians are to be encouraged to adopt this new and evolving diagnostic skill.
Conflict of interest
None. 
*Patient consent was obtained for the use of clinical information and images/videos.
References:
Ahmed S, Martin DA, Smith BK (2019) Inspiratory Muscle Training in Patients with Prolonged Mechanical Ventilation: Narrative Review. Cardiopulm Phys Ther., 30(1): 44-50.
Alrajhi K, Woo MY, Vaillancourt C (2012) Test characteristics of ultrasonography for the detection of pneumothorax: a systematic review and meta-analysis. Chest, 141(1931-3543 (Electronic)): 703-708.
Arbelot C, Neto FLD, Gao Y et al. (2020) Lung Ultrasound in Emergency and Critically Ill Patients: Number of Supervised Exams to Reach Basic Competence. Anesthesiology, 132(4): 899-907.
Bissett BM, Leditschke IA, Neeman T et al. (2016) Inspiratory muscle training to enhance recovery from mechanical ventilation: a randomised trial. Thorax, 71(9): 812-819.
Bouhemad B, Brisson H, Le-Guen M et al. (2011) Bedside ultrasound assessment of positive end-expiratory pressure-induced lung recruitment. Am J Respir Crit Care Med., 183(3): 341-347.
Bouhemad B, Liu ZH, Arbelot C (2010) Ultrasound assessment of antibiotic-induced pulmonary reaeration in ventilator-associated pneumonia. Crit Care Med., 38(1): 84-92.
Cavaliere F, Biasucci D, Costa R et al. (2011) Chest ultrasounds to guide manual reexpansion of a postoperative pulmonary atelectasis: a case report. Minerva Anestesiol., 77(7): 750-753.
Cuca C, Scheiermann P, Hempel D et al. (2013) Assessment of a new e-learning system on thorax, trachea, and lung ultrasound. Emerg Med Int., 2013: 145361.
Dres M, Goligher EC, Heunks LMA et al. (2017) Critical illness-associated diaphragm weakness. Intensive Care Med., 43(10): 1441-1452.
Elkins M, Dentice R (2015) Inspiratory muscle training facilitates weaning from mechanical ventilation among patients in the intensive care unit: a systematic review. J Physiother., 61(3): 125-134.
Fukuhara T, Donishi R, Matsuda E et al. (2018) A Novel Lateral Approach to the Assessment of Vocal Cord Movement by Ultrasonography. World J Surg., 42(1): 130-136.
Greenstein YY, Littauer R, Narasimhan M et al. (2017) Effectiveness of a Critical Care Ultrasonography Course. Chest, 151(1): 34-40.
Hanekom SD, Faure M, Coetzee A (2007) Outcomes research in the ICU: an aid in defining the role of physiotherapy. Physiother Theory Pract., 23(3): 125-135.
Hansell L, Milross M, Delaney A et al. (2021) Lung ultrasound has greater accuracy than conventional respiratory assessment tools for the diagnosis of pleural effusion, lung consolidation and collapse: a systematic review. J Physiother., 67(1): 41-48.
Hayward S, Smith M, Innes S (2020) Diagnostic thoracic ultrasound imaging - An exploration of respiratory physiotherapists' interest and use in clinical practice: A national survey. Ultrasound, 28(1): 14-22.
Hayward SA, Janssen J (2018) Use of thoracic ultrasound by physiotherapists: a scoping review of the literature. Physiotherapy, 104(4): 367-375.
Hew M, Corcoran JP, Harriss EK et al. (2015) The diagnostic accuracy of chest ultrasound for CT-detected radiographic consolidation in hospitalised adults with acute respiratory failure: a systematic review. BMJ Open 5(2044-6055 (Electronic)): e007838
Hulett CS et al. (2014) Development and preliminary assessment of a critical care ultrasound course in an adult pulmonary and critical care fellowship program. Ann Am Thorac Soc 11(2325-6621 (Electronic)): 784-788.
Lakhal K et al. (2012) Chest radiographs in 104 French ICUs: current prescription strategies and clinical value (the RadioDay study). Intensive Care Med 38(11): 1787-1799.
Le Neindre A et al. (2016) Thoracic ultrasound: Potential new tool for physiotherapists in respiratory management. A narrative review. J Crit Care 31(1): 101-109.
Le Neindre A et al. (2021) Diagnostic accuracy of diaphragm ultrasound to predict weaning outcome: A systematic review and meta-analysis. Int J Nurs Stud 117(1873-491X (Electronic)): 103890.
Leech M et al. (2015) Physiotherapist-initiated lung ultrasound to improve intensive care management of a deteriorating patient and prevent intubation: a case report. Physiother Theory Pract: 1-5.
Maw AM et al. (2019) Diagnostic Accuracy of Point-of-Care Lung Ultrasonography and Chest Radiography in Adults With Symptoms Suggestive of Acute Decompensated Heart Failure: A Systematic Review and Meta-analysis. JAMA Netw Open 2(2574-3805 (Electronic)): e190703.
Noble VE et al. (2009) Ultrasound assessment for extravascular lung water in patients undergoing hemodialysis. Time course for resolution. Chest 135(6): 1433-1439.
Ntoumenopoulos, G et al. (2018) Secretion clearance strategies in Australian and New Zealand Intensive Care Units. Aust Crit Care 31(4): 191-196.
Ntoumenopoulos G, Hough J (2014) Diagnostic thoracic ultrasound within critical care. J Physiother 60(2): 112.
Patman S et al. (2009) Physiotherapy does not prevent, or hasten recovery from, ventilator-associated pneumonia in patients with acquired brain injury. Intensive Care Med 35(2): 258-265.
Stiller K (2013) Physiotherapy in intensive care: an updated systematic review. Chest 144(3): 825-847.
Stiller K et al. (1990) Acute lobar atelectasis. A comparison of two chest physiotherapy regimens. Chest 98(6): 1336-1340.
Stiller K et al. (1996) Acute lobar atelectasis: a comparison of five physiotherapy regimens. Physio Theory and Practice 12: 197-209.
Templeton M, Palazzo MG (2007) Chest physiotherapy prolongs duration of ventilation in the critically ill ventilated for more than 48 hours.Intensive Care Med 33(11): 1938-1945.
Tutino L et al. (2010) Time needed to achieve completeness and accuracy in bedside lung ultrasound reporting in intensive care unit. Scand J Trauma Resusc Emerg Med 18: 44.
Via G et al. (2012) Lung ultrasound in the ICU: from diagnostic instrument to respiratory monitoring tool. Minerva Anestesiol 78(11): 1282-1296.
Vieira R et al. (2020) Lung ultrasound as a tool to guide respiratory physiotherapy. J Clin Ultrasound 48(7): 431-434.
Volpicelli G et al. (2012) International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med 38(4): 577-591.
Vorona S et al. (2018) Inspiratory Muscle Rehabilitation in Critically Ill Adults. A Systematic Review and Meta-Analysis. Ann Am Thorac Soc 15(6): 735-744.
Williamson JP et al. (2017) Thoracic ultrasound recognition of competence: A position paper of the Thoracic Society of Australia and New Zealand. Respirology 22(2): 405-408.
Worraphan S et al. (2020) Effects of Inspiratory Muscle Training and Early Mobilization on Weaning of Mechanical Ventilation: A Systematic Review and Network Meta-analysis. Arch Phys Med Rehabil 101(11): 2002-2014.
Xirouchaki N et al. (2014) Impact of lung ultrasound on clinical decision making in critically ill patients. Intensive Care Med 40(1): 57-65.
Xirouchaki N et al. (2011) Lung ultrasound in critically ill patients: comparison with bedside chest radiography. Intensive Care Med 37(9): 1488-1493.
Yousefifard M et al. (2016) Screening Performance Characteristic of Ultrasonography and Radiography in Detection of Pleural Effusion; a Meta-Analysis. Emerg (Tehran) 4(2345-4563 (Print)): 1-10.
Zambon M et al. (2013) Ultrasound in critically ill patients: focus on diaphragm. Intensive Care Med 39(5): 986.








