What is point-of-care ultrasound?
Point-of-care ultrasound (POCUS) describes the use of ultrasound to extend the physical examination of patients at the bedside, guiding diagnosis and management. POCUS covers an array of ultrasound modules, including echocardiography, lung ultrasound, abdominal ultrasound etc.
The use of ultrasound has undeniably extended far beyond the walls of the radiology department, being utilised in more acute medical specialties such as emergency medicine and critical care. POCUS scans are different from those performed by radiologists or sonographers. These scans tend to be take place at the bedside in non-acute situations and are requested to answer very specific, detailed questions. POCUS scans are performed in order to answer questions, usually in a binary way i.e. yes or no. For an overview of POCUS and critical care, there has been a recent review in a previous edition of this journal (Zaidi and Koenig 2018).
There are numerous training resources available to clinicians, but crucially, the number of nationally-recognised accreditation programmes remains small. It is important to emphasise that clinicians must operate within their own competencies. The use of POCUS does not replace the need for thorough history taking, clinical examination and acumen. Instead, it enhances the clinician’s ability to diagnose and manage critically ill patients. There is ongoing debate on whether POCUS will replace the stethoscope (Wittenberg 2014).
POCUS in shock - an integrated approach
Encountering the shocked patient is a common occurrence in the ED and the intensive care unit (ICU). Other articles in this issue have already covered the definition and types of shock. It must be emphasised that different types of shock may co-exist in the same patient e.g. the septic patient may be shocked due to distributive/vasodilatatory shock or cardiogenic shock. POCUS allows the clinician to more accurately identify the type and/or coexistence of the different types of shock and hence target management strategies accordingly.
A perceived weakness of comprehensive radiology or echocardiography scans is that they are often performed in isolation. As mentioned above, POCUS is performed by the bed space and the key to making these diagnoses is the ability to examine clinically, followed closely by ultrasound.
The key modules in the diagnosis and management of shock are the examination of the cardiovascular and respiratory system i.e. heart and lungs.
Focused echocardiography is probably the most established POCUS module. The key questions to be answered are:
- Is the left ventricle (LV) dilated or impaired?
- Is the right ventricle (RV) dilated or impaired?
- Is the inferior vena cava (IVC) collapsing?
- Is there a pericardial effusion?
- Is/are there pleural effusion(s)?
The complexity of the examination and the techniques used are obviously operator-dependent. However, there is broad consensus that basic transthoracic echocardiography should be a core competency for every critical care clinician.
Despite being a relatively new module, lung ultrasound has expanded exponentially since the work of Lichtenstein and colleagues (Lichtenstein and Mezière 2008). Once used only to assess for pleural effusions, superior to chest radiographs, our understanding and hence utilisation of this module has expanded to include a much broader range of diagnoses. A recent systematic review and meta-analysis concluded that lung ultrasound was superior to chest radiographs in terms of sensitivity, with similar specificity, hence challenging it as a first-line diagnostic tool (Winkler et al. 2018).
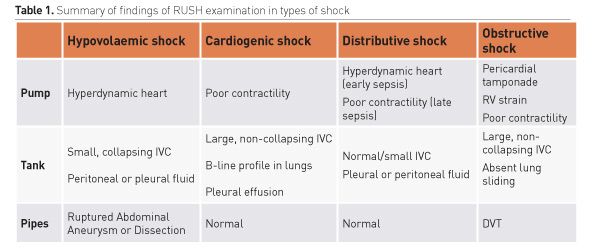
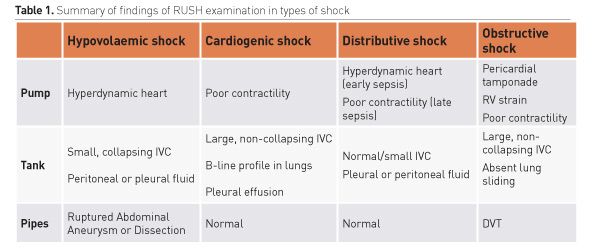
The Rapid Ultrasound for Shock and Hypotension (RUSH) protocol (Perera 2010) was designed so that emergency physicians could carry out a structured, easy-to-perform ultrasound examination (under two minutes). It requires an examination of the heart, intravascular filling status and large arteries/veins or simply Pump, Tank and Pipes respectively. Table 1 summarises the ultrasonographic findings for the various types of shock using RUSH. As mentioned, it must be remembered that the various types can co-exist in the same patient.
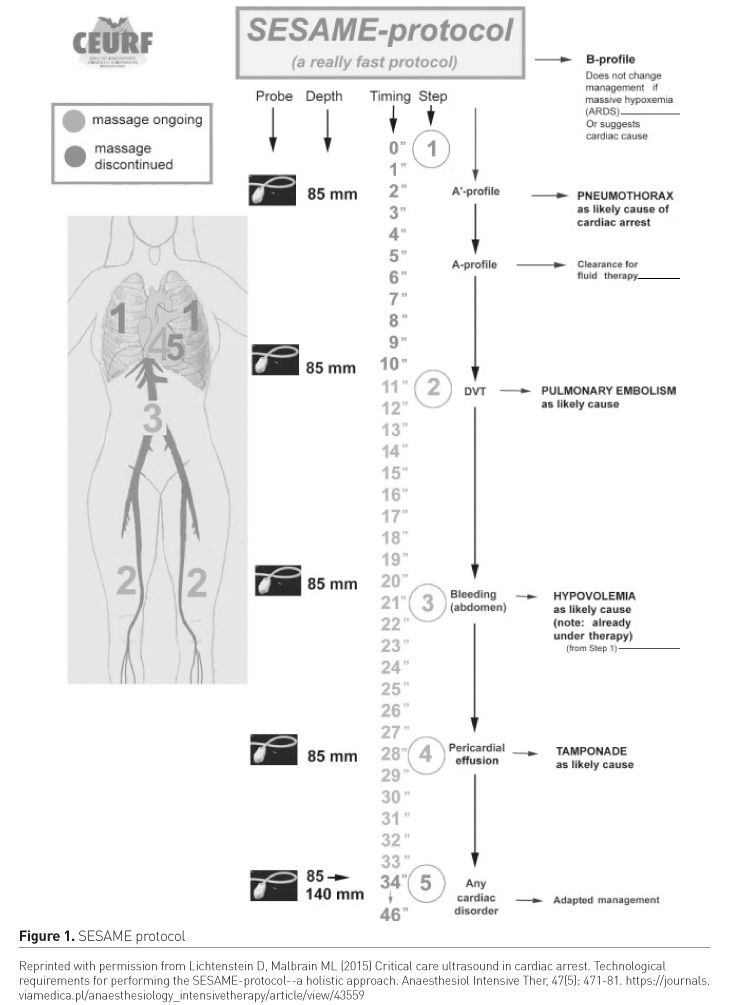
The RUSH protocol is by no means the only integrated POCUS-based protocol; others include the SESAME (abbreviated from SESAMOOSIC Sequential Echographic Scanning Assessing Mechanism or Origin of Shock of Indistinct Cause) (Figure 1, Lichtenstein and Malbrain 2015) and the Abdominal and Cardiothoracic Evaluation with Sonography in Shock (ACES) protocols. Such integrated approaches form a significant part of most POCUS curricula and courses in emergency medicine and critical care.
In addition to its diagnostic prowess, POCUS can also be used to assess response to therapy such as fluid administration in the context of the shocked patient. Dynamic measures such as the velocity-time integral measured in the aortic outflow tract have been shown to be a useful measure of fluid responsiveness (Miller and Mandeville 2016).
Integrating POCUS into daily practice
POCUS, like any other monitoring device, has not been shown to improve patient outcomes without being coupled with an appropriate management strategy. The recently published SHoC-ED trial (Atkinson et al. 2018) failed to show any mortality benefit when shocked patients were managed using a POCUS-centric approach compared to standard care. The reasons are probably multifactorial, but this should act as a word of caution to the enthusiastic practitioner.
The best time to perform a POCUS examination is when the patient requires it. The convenience does come at the cost of taking up clinician time and interrupting the workflow of the day and ward round; this interruption is particularly relevant since not all clinicians are currently competent in POCUS. With clinicians’ time increasingly being stretched, a way of balancing the inherent benefits of POCUS and drawbacks is crucial. Ultimately, different ICUs adopt different techniques based on staffing, working shift patterns, experience and availability of POCUS practitioners, number of ICU/ high dependency unit (HDU) beds, workload and ready access to a suitable ultrasound machine. There is unlikely to be a single best method and the most practical and realistic way of incorporating POCUS into the working culture, training and patient care on the ICU is probably a combination of all three.
What the future may hold
There is broad consensus that basic POCUS should be part of core competencies for intensivists. Consensus and expert statements published in 2011 (Expert Round Table on Ultrasound in ICU 2011) have led to the development of national accreditation programmes to support colleagues in developing and maintaining this skillset. Comparisons of these programmes highlight a degree of variability between them and consensus is needed to better define these competencies to ensure high-quality training and ultimately improve patient care.
Supporting improved access to training, technology continues to advance in order to make POCUS machines more accessible and portable. Earlier ultrasound machines were often bulky, not very portable and were considered cumbersome to use. The newer machines of several manufacturers can now fit into the palm of your hand e.g. Philips LumifyTM and Sonosite IVIZTM. Some of these probes are plugged into the clinician’s smartphone and utilise the screen of the device. Early versions of such portable ultrasound machines had variable image quality and functionality as a trade-off to size but again, more modern devices have closed this gap.
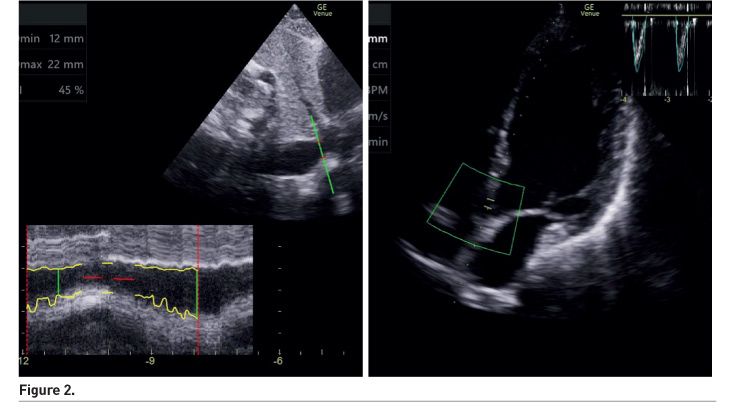
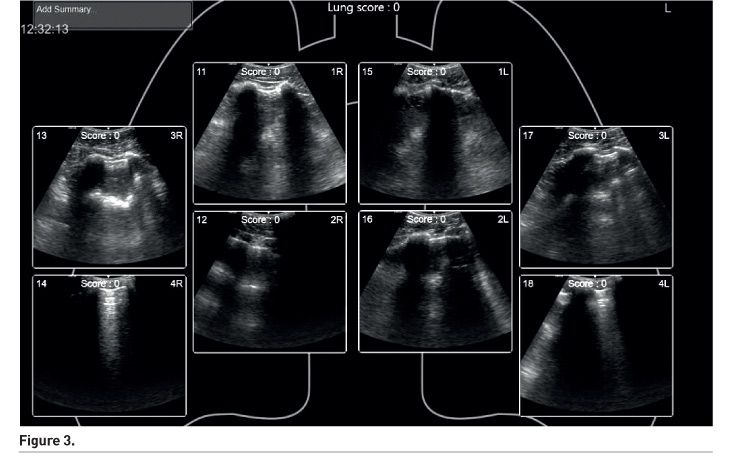
Image acquisition is only one part of the ability to make the diagnosis and formulate a management plan. Image interpretation is an integral part of the training process and competency assessment. Artificial intelligence (AI), as seen in other industries has also started to ‘invade’ healthcare. Several manuscripts on the use of AI to interpret scans for signs of malignancies have been published. Extrapolating from this example, machines such as the GE VenueTM have built-in software in order to facilitate measurements of cardiac output and interpret lung ultrasound findings (Figure 2 and 3). These AI systems are meant to aid and not replace the human clinician.
Conclusion
Shock is a common, complex clinical condition with several classical types that may co-exist. POCUS techniques offer a powerful diagnostic and management tool which is within the skillset of intensivists after appropriate training.
Conflict of interest
Adrian Wong and Jonathan Wilkinson have both trialled various ultrasound devices from different manufacturers. JW has self-funded a portable ultrasound device for his own personal use in his clinical work. AW and JW declare that they have no financial conflict of interest.