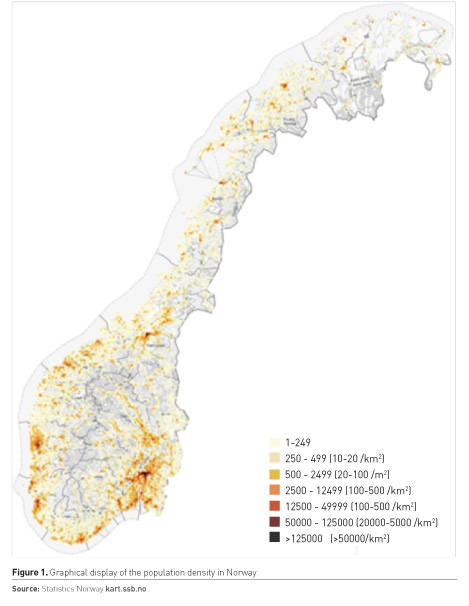
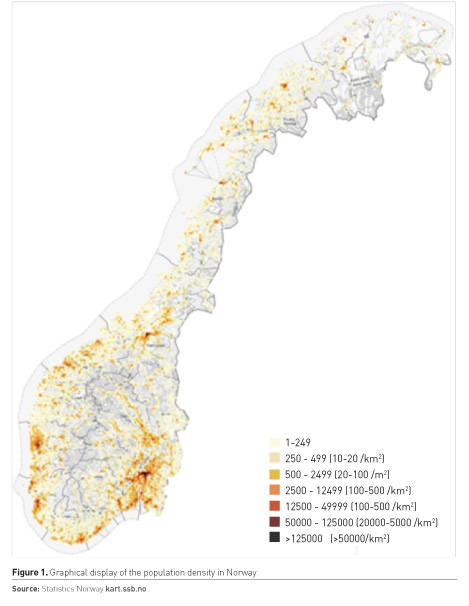
Norway is a rather small country with a population of about 5.3 million. More than half of these inhabitants are located in and around the larger cities, with about a million in the capital region of Oslo. Hence, significant parts of the country are rural, with fjords and high mountains, combined with winter darkness and harsh weather conditions (Figure 1). However, the country is 2500 km long and has approximately 50 hospitals, all part of the national health system. Some of these hospitals are serving large and sparsely populated areas. These hospitals may have rather small post-anaesthesia care units (PACUs) caring for intensive care unit (ICU) patients, but ICU patients in need of more specialised care will in most cases be transferred to the larger hospitals with more complete ICUs by ground or air ambulance. This has had a great influence on how the Norwegian acute healthcare system is organised.
Our country has been blessed with a solid economy based on export of oil, gas and fish, giving the politicians financial resources for reaching their goal of providing the same level of health services for everyone regardless of place of residence. Given the challenging nature of this aim, one may argue that they have succeeded since Norway scores high on parameters like life expectancy and other health-related indicators.
The Norwegian acute healthcare system is based on two key factors:
- A well-developed emergency care system organised in the municipality, and
- A nationally distributed and complete emergency medical system (EMS), with a nationwide medical emergency communication system connecting the emergency communication centres, ground and boat ambulances, in addition to numerous air ambulances (both fixed-wing and rotor-wing). The latter resources are staffed by specially trained nurses and anaesthesiologists.
Norwegian emergency healthcare organisation
According to national regulations, every Norwegian municipality must have a system in place for providing emergency medical care for their residents and also others, e.g. visitors and tourists. This means that the more than 300 municipalities are responsible for the primary healthcare service, including the primary care general practitioners (GPs), and GPs on call 24-7. In addition, they are also responsible for providing out-of-hours services and there are approximately 100 local emergency medical communication centres (LEMC) and 180 local casualty clinics. Because of this system, it is rather uncommon that a patient presents at a hospital emergency department (ED) without being seen by a physician on beforehand. The exception is in some of the emergencies, where ambulances transport severely ill and injured patients directly to the ED. The four regional health authorities are responsible for the secondary and specialised healthcare service through the local hospital trusts. This includes hospitals, ground, boat and air ambulance services, and the emergency medical communication centres (EMCC) (Official Norwegian Reports 2015; Ministry of Health and Care Services 2015) (Figure 1).
Care for acutely ill or traumatised patients is based on a two-tiered system where the municipalities are responsible for the first part and the hospital trusts responsible for the more specialised part of the system. GPs, ambulance personnel and sometimes the anaesthesiologists in the air ambulance system, cooperate in acute pre-hospital responses. Other countries organise their emergency healthcare system differently, many without the involvement of GPs or the primary healthcare services. GPs have an important role in the Norwegian primary care services. One function is the work as a “gatekeeper”, and patients must be admitted to hospital by a doctor. Exceptions are made when ambulance personnel consider the patient to have a life-threatening medical condition, and the patient is transported directly to hospital.
Persons in need of emergency medical care are supposed to call the national emergency telephone number 113, reaching the nearest EMCC (Norwegian Medical Association 2009). The Norwegian EMCCs are staffed with medically trained personnel (nurses and ambulance personnel with emergency medicine experience). They will provide counselling, and alert the appropriate emergency health resources if needed, including dispatch of ambulances, on-call GPs and air ambulance. The EMCCs use a national priority dispatch system as a decision tool (the Norwegian Index for Medical Emergencies) to classify medical problems into three different levels of responses represented by colour codes (Norwegian Medical Association 2009). Health authorities regulations require 90% of all emergency phone calls to EMCCs to be answered within 10 seconds (Ministry of Health and Care Services 2015). If inhabitants suspect an acute (but not life-threatening) condition in need of medical care they are supposed to call the nearest LEMC via the national number 116117. Like the EMCC, the LEMC are staffed with nurses. National regulations require that LEMC should answer 80% of phone calls within 2 minutes (Ministry of Health and Care Services 2015). A digital and restricted nationwide medical communication network is used for communication between the LEMCs, EMCCs and the other cooperating resources
*.
The medical emergency responses are divided into three levels:
Acute or red responses in presumably life-threatening situations, where the GP on call and ambulance is immediately dispatched (Official Norwegian Reports 2015). Approximately 25% of all contacts with EMCCs are due to acute responses, while only 3% of the contacts to LEMCs lead to an acute response (Haaheim et al. 2014; Morken et al. 2016).
Urgent or yellow responses in potentially life-threatening situations, where an ambulance may be dispatched or the patient referred to a local GP (Official Norwegian Reports 2015). Approximately 36% of the contacts with EMCC lead to an urgent response, while 27% of the contacts to LEMC lead to an urgent response (Haaheim et al. 2014; Morken et al. 2016). Usually the EMCC transfer these calls to a LEMC if the medical problem does not require an ambulance (Norwegian Medical Association 2009).
Non-urgent or green response is when it is presumed that time is of little medical importance and the patient can wait to be examined until a doctor eventually is available (Norwegian Medical Association 2009). Usually, these patients are evaluated by their GP during office hours. Approximately 36% of the contacts with EMCC are due to non-urgent responses, while 70% of the contacts with LEMC are due to non-urgent responses (Haaheim et al. 2014; Morken et al. 2016).
Every year, the more than 500 ambulances perform close to 700,000 missions (130 per 1,000 inhabitants), of which approximately 30% are acute, 40% urgent and 30% non-urgent missions (Statistics Norway 2015). Response time varies, and in 2016, the rural ambulance services reached the patient within 25 minutes in 81% of the missions, while in urban areas, the ambulance reached the patient within 12 minutes in 72% of the missions. The national goal is 90% in both described cases (Helsedirektoratet 2016). In rural parts of Norway, there is a relatively low volume of severely injured or ill patients, and therefore both GPs and ambulance personnel need frequent training to maintain their skills (Official Norwegian Reports 2015; Myklestad et al. 2014; Norwegian National Advisory Unit on Trauma 2015). This type of training is seen as cost-effective skill improvement and is required by regulations (Ministry of Health and Care Services 2015; Utsi et al. 2008).
The Norwegian Intensive Care Registry (intensivregister.no) receives data from about 36 hospitals. In 2016 a total of 13,679 ICU patients, accounting for 15,403 ICU-stays and 62,311 ICU-days were registered. Close to 60% of the stays were at local and central hospitals, while the rest were at the four university hospitals. The median length of stay was 2.0 days (95% CI=2.0-2.2), and the overall 30-day mortality was 23%.
As can be expected with many rural hospitals, a number of patients in need for specialised ICU treatment must be transported to the larger ICUs. Hence, there is need for a system for transporting such patients between hospitals, and in Norway this is solved by a national air ambulance system.
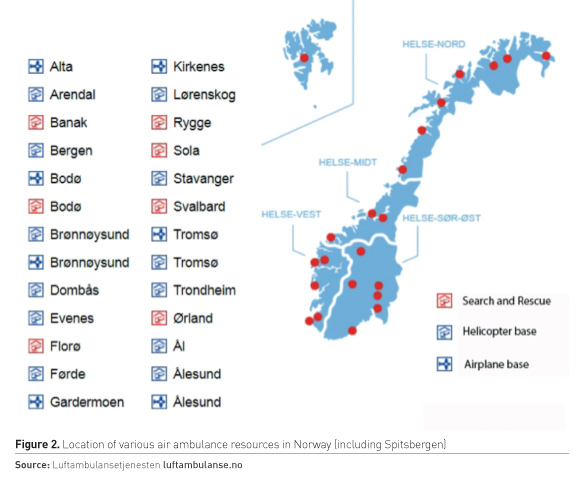
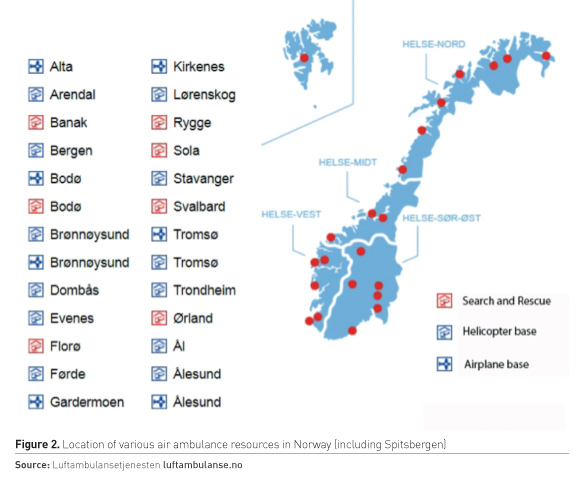
The national air ambulance service consists of 13 physician-staffed ambulance helicopters (on 12 bases), equipped to offer advanced emergency medical treatment outside the hospital and to transport patients directly to a hospital if needed (Norwegian National Air Ambulance Service n.d). In addition, there are seven search and rescue (SAR) helicopters and nine fixed-wing aeroplane air ambulances, which also are part of the national air ambulance system (Figure 2). This service provides an important part of the pre-ICU system, and also has the capability to transport patients on ECMO and intra-aortic balloon pump, and incubators with babies on nitric oxide. In 2016, this service treated approximately 20,000 patients, of whom about 6,000 were transfers between hospitals (Statistics Norway ssb.no).
As one can understand from the above, in a long and sparsely populated country, with challenging geography and weather, the pre-ICU system in Norway is comprehensive and well developed. Nevertheless, there is a constant need for identifying patients in need of ICU care, and also to maintain quality of care at smaller hospitals, which don’t treat seriously ill or injured patients on a regular basis. Team training and simulation has become an important way of compensating for this (Wisborg et al. 2008).
Conflict of interest
Guttorm Brattebø declares that he has no conflict of interest. Øyvind Østerås declares that he has no conflict of interest.
* Nødnett – the Norwegian Emergency Public Safety Network is a separate radio network, built specifically for rescue and emergency users.