ICU Management & Practice, Volume 17 - Issue 4, 2017
Achieving large-scale behaviour change with the NHS Wales programme
In 2016 NHS Wales
received the Global Sepsis Award, recognising the work throughout the
healthcare system on improving identification and treatment of sepsis, which
has coincided with an apparent reduction in mortality and ICU admissions for
patients with two International Statistical Classification of Diseases and
Related Health Problems (ICD-10) sepsis codes. The main vehicle for change has
been participation of all Welsh healthcare organisations in the 1000 Lives
Rapid Response to Acute Illness Learning Set (RRAILS). This article examines
some of the factors which have been critical in achieving large-scale behavior change
as part of this patient safety programme.
Acute deterioration in Wales
The
National Health Service (NHS) in Wales is a devolved healthcare system serving
a population of 3.1 million via sixteen acute and tertiary hospitals supported
by numerous community hospitals and a single Welsh Ambulance Service.
You might also like:Impact of rapid response teams on ICU
Sepsis and acute kidney injury (AKI) have been appreciated by Welsh Government and NHS Wales as major causes of avoidable harm and death for many years and were the subjects of patient safety alerts in 2014 and 2016 respectively. The treatment of sepsis became a ‘Tier 1’ priority for NHS Wales in 2013.
Measuring the incidence and burden of sepsis is difficult due to issues of definition and data capture. Scaling the findings of a large meta-analysis (Fleischmann et al. 2016) for the population of Wales gives an incidence of between 8000-13,000 per annum with an associated mortality of between 2200-2300.
These estimates accord both with extrapolation from an inspection of UK critical data (Daniels 2011a) and a retrospective review of mortality within one Welsh hospital (Robinson 2013). The latter study estimated sepsis to be responsible for approximately 15% of hospital deaths.
The ‘Size of sepsis in Wales study’ (Szakmany et al. 2016) found a prevalence of sepsis and severe sepsis in Welsh acute hospitals of 5.5% with associated mortality at 90 days of 31%.
Although AKI is acknowledged to be a common feature of sepsis the extent of co-existence is unclear. However, a comprehensive system of AKI electronic alerts introduced in 2015 has enabled the quantification of AKI in Welsh hospitals. The incidence reported from the alert system is greater than 4000 patients each month whilst analysis has found an associated mortality of 25.6% (Holmes et al. 2016).
Changing behaviour at scale
The
main vehicle for improvement for acute deterioration in NHS Wales has been the
active participation of all Health Boards and Trusts in the 1000 Lives
Improvement Service Rapid Response to Acute Illness Learning Set (RRAILS).
RRAILS was launched in 2011 with the purpose of introducing the National Early
Warning Score (NEWS), sepsis screening and implementation of the Sepsis 6 care
bundle.
In 2016 NHS Wales received the Global Sepsis Award from the Global Sepsis Alliance with a citation from Professor Dr. Konrad Reinhart and Dr. Carl
Flatley that reads:
Your tremendous efforts in our common fight against sepsis
are a shining example and an inspiration for other sepsis initiatives around
the world showing what can be done with outstanding commitment and great
passion.
We believe that there are several distinct features of the RRAILS programme in NHS Wales that have enabled achievement of this success, which are discussed below.
Focus on reliability—right treatment, every patient, every time
The landmark study by McGlynn et al. (2003) demonstrated that what they referred to as the “defect rate in technical quality of American healthcare” stood at 45%, whilst a UK study (Burnett et al. 2012) found reliability rates in simple healthcare procedures at 82-87%. The implications of these findings are that healthcare systems are poor at achieving consistency in delivery of the basic elements of healthcare and that this level of reliability would be unacceptable in many industries and certainly in those where safety is critical.
The report Time to Intervene? (National Confidential Enquiry into Patient Outcome and Death [NCEPOD] 2012) demonstrated that the consequences of this poor process reliability in the recognition, escalation and response to acute deterioration resulted in a high rate of avoidable mortality.
The originators of the concept of Safety II argue that “Safety management should .... move from ensuring that ‘as few things as possible go wrong’ to ensuring that ‘as many things as possible go right’” (Hollnagel et al. 2015). The focus of the RRAILS programme has therefore been on making things go right as often as possible and upon improving the rate of ‘always events’ rather than reducing ‘never events’.
To achieve this we have supported clinicians with standardised tools and operating procedures, used human factors principles to encourage implementation and enabled clinical teams to measure their own improvement.
NEWS – a common language of risk
The National Early Warning Score (NEWS) has been advocated by the Royal College of Physicians for adoption in all UK hospitals following evaluation as the early warning score that was the best predictor of death within 24 hours (Prytherch et al. 2010). NEWS was fully implemented in all acute Welsh hospitals by 2013 (the first country to achieve this).
Implementation has enabled the common setting of triggers of 3, 6 and 9 as representative of low, medium and high risk and has enabled stratification of escalation response. However, its primary value has not been that of being a perfect tool—it is not—but rather in its provision of a common language through which clinicians in different geographical and care settings can communicate.
Consequently NEWS has been adopted by the Welsh Ambulance Service, most community hospitals and primary care teams and even in some private care homes.
‘Good enough’ tools enable the whole team
The universal adoption of NEWS meant that a common screening tool could be developed. As of 2012 NHS Wales started to use a standard set of criteria based upon a NEWS of 3 or more plus two or more Systemic Inflammatory Response Syndrome (SIRS) criteria and the suspicion of infection.
As the evidence for SIRS has been downgraded and the definition of sepsis been revised (Singer et al. 2016), this tool has nevertheless continued to play an important part in the escalation process for all acutely ill patients, and it has become apparent that the reason for this is that it has enabled all clinical staff within a two-stage process:
Stage 1: identification mainly falls to the healthcare support workers (HCSW) who perform vital signs observations. The screening tool information has been codified on plastic credit card-sized NEWS cards carried by many staff (Figure 1) and on the observation charts, and so serves to encourage the HCSWs to act quickly to start the escalation process.
Stage 2: diagnosis and decision to treat is strongly aided by the use of NEWS which, recent
evidence indicates, is a better predictor of sepsis than other tools used
outside of critical care (Churpek et al. 2017). We are now able to make a
strong recommendation to treat for sepsis at NEWS of 6 or more in the presence
of infection, based of course on clinical judgement.
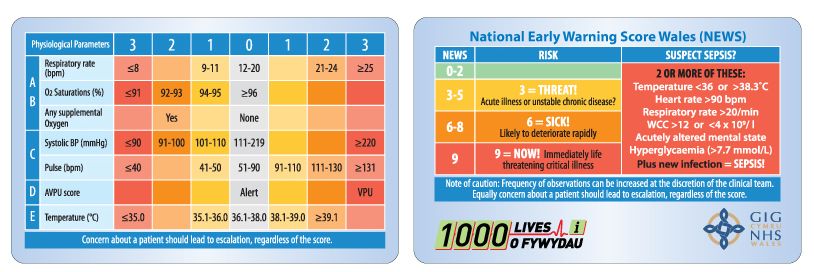
Figure 1. National Early Warning Score (NEWS) card
Always events not never events
One of the notable findings of the report Just Say Sepsis (NCEPOD 2015) was that of improved process and outcome measures where the Sepsis 6 care bundle was used to treat sepsis. Daniels et al. (2011b) found a significant reduction in mortality associated with reliable implementation of the bundle.
The Sepsis 6 care bundle has been adopted as the standard throughout Wales with the documentation in most cases simply consisting of carbon copy forms. Whilst the evidence for most elements of the bundle is now less strong, it has become apparent that its use has an extra ability to drive and motivate completion of sepsis treatment within one hour.
A similar approach has been taken with response to the AKI e-alerts with a four-item care bundle. Preliminary results from a trial involving the Critical Care Outreach Team (CCOT) in instigating the bundle have been promising.
Make it easy and attractive to ‘do the right thing’
The Behavioural Insights Team (BIT), famous for their development of ‘nudge’ theory, uses the acronym EAST (Easy, Attractive, Social and Timely) to describe an approach to achieve behaviour change (Service 2014). The authors argue that in order to encourage a behavior it is necessary to make it easy and attractive to adopt that new behaviour. This has particular relevance in healthcare systems where behaviour change may have been traditionally attempted by ‘top-down’ diktats and punitive performance management.
An important part of the EAST model is the idea of setting the default action. This can be seen to be integral to the standardized recognition, escalation and treatment tools for AKI and sepsis. It is important to emphasise that setting the default should not force clinicians to act against their better judgement, but instead the standard operating procedure should act as a safety net to prevent errors of omission. Thus the dynamic changes from one of opting in to one where deviance from the default should be justified.
Give permission to act
In innovating to achieve behaviour change it is also possible and we believe vital that clinicians are given ‘permission to act’. The RRAILS team has collaborated in the design of several physical tools that fulfil this function including the NEWS Card (Figure 1), Wee Wheel (Figure 2) and KidneySafe Bracelet (Figure 3), which are popular, easy to use and encourage the prevention of AKI and sepsis (Subbe 2015).
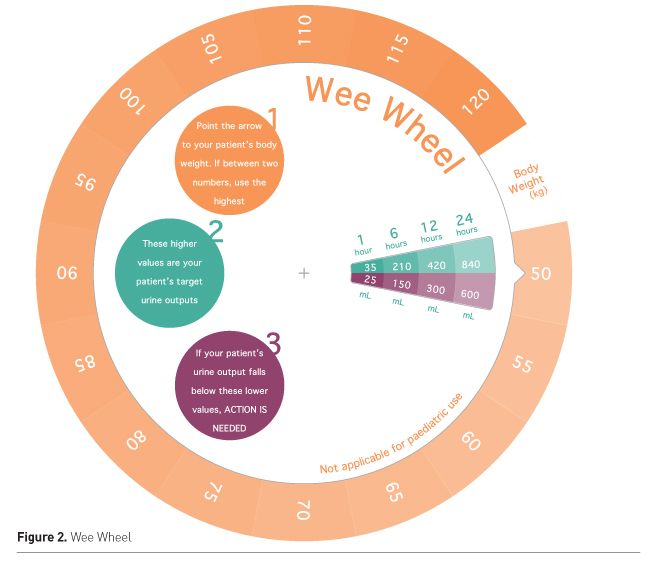
Figure 2. Wee Wheel
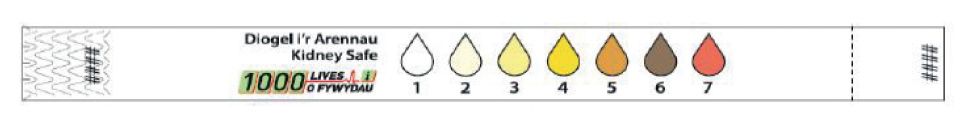
Figure 3. Kidney Safe Bracelet
An important development has been that of the sepsis bag, box or trolley which has been developed and tested by several of the participating Health Boards.
The idea of this innovation is simple and expresses very much the human factors principle of co-locating all the elements needed to complete a procedure, in this case the Sepsis 6, in order to make it far more likely that the procedure will be carried out correctly.
Plot the dots – the importance of measurement
A phrase attributed to the quality improvement expert W.E. Deming is “Without data you’re just another person with an opinion.”
With this in mind, a vital part of the RRAILS programme has therefore been to support frontline clinicians to understand their performance by giving them tools to enable them to develop quick and easy run charts of incidence and compliance with sepsis treatment for display in ward areas.
There has been an intentional move to promote the use of run charts as the means of recording data and, where possible, to record data on an ‘every patient’ rather than sampled basis. The run charts are annotated to enable the teams to appreciate the effect of changes in practice. The run chart establishes a shared narrative and so promotes the feeling of ‘shared mission’ amongst the team.
The literature on so-called high reliability organisations (Weick and Sutcliffe 2007) details how ‘sensitivity to operations’ or the ability to understand at the highest organizational levels how the core work is progressing is essential. The reporting on the incidence of positive sepsis screening and compliance with Sepsis 6 has fulfilled this criteria to some extent and these measures form part of many organisations’ metrics frameworks.
Programme evaluation
At a national level we were able to look at the incidence of sepsis recorded in hospital stays and subsequent mortality (in and out of hospital), by linking hospital episode data with death certificates.
Hospital
stays were selected by looking for episodes with an ICD-10 diagnostic code for ‘streptococcal
sepsis’ (A40) or ‘other sepsis’ (A41) (Figure 4). We have also looked at coding for
urosepsis and pneumonia to assure ourselves that incidence or mortality was not
simply being coded differently over time, and conferred with clinical coding
colleagues in the national informatics service about possible changes in coding
practice (for example, the change from ‘septicaemia’ to ‘sepsis’ in the 4th
edition of ICD-10).
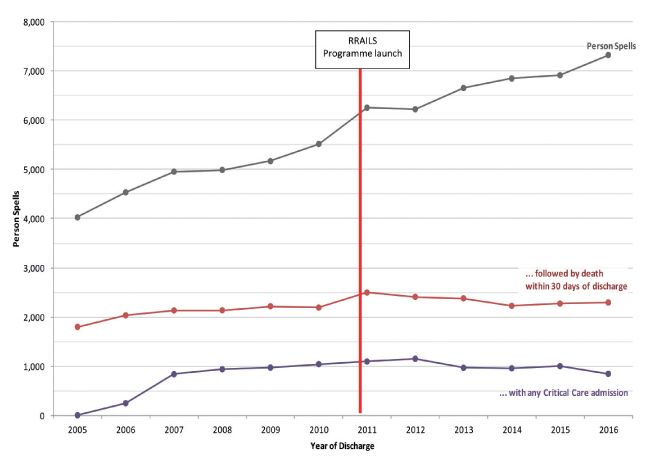
Figure 4. Person spells with any mention of A40-A41
A straightforward inspection of the data reveals a reliable increase in recorded incidence over the last decade. By contrast, the annual number of deaths within 30 days of discharge fell for several years in a row from 2011 onwards and remains lower than 6 years ago.
Meaningful statistical analysis of the mortality rate is complicated by the combination of both likely improved recognition and diagnosis, and possibly genuine increases in incidence. The rate clearly drops enormously, but this is largely due to the increase in recorded incidence. Provider-level data shows more complicated patterns of changing incidence, mortality and critical care admission. Nevertheless we believe that the observed reduction in the crude number of deaths against this backdrop of increasing incidence, and in the context of compelling local data, strongly suggests that hundreds of deaths may have been avoided since the introduction of the programme. Similarly the national data also suggest that critical care admissions of those with sepsis fell slightly after 2012. Given the expected lengths of stay for those with sepsis, this may represent a significant potential saving.
Conclusion
Correlation does not prove causality and we must be cautious about the attribution of improved outcomes to behaviours that have taken place across many different organizations in differing care settings over lengthy timescales.
Nevertheless it seems reasonable to claim that patient safety programmes situated in healthcare economies serving populations of between three and five million and focusing upon standardisation to achieve process reliability, enablement of all clinicians to act, quick and easy measurement and creation of a social movement can be an effective model for improvement.
Acknowledgements
- Abertawe Bro Morgannwg University Health Board
- Aneurin Bevan University Health Board
- Betsi Cadwaladr University health Board
- Cardiff and Vale University Health Board
- Cwm Taf University Health Board
- Hywel Dda University Health Board
- Powys Teaching Health Board
- Public Health Wales
- Velindre NHS Trust
- Welsh Ambulance Services NHS Trust
Conflict of interest
Chris
Hancock declares that he has no conflict of interest. Adam Watkins declares
that he has no conflict of interest.
Abbreviations
AKI acute kidney injury
NEWS National Early Warning Score
RRAILS Rapid Response to Acute Illness Learning Set
References:
Burnett S, Franklin BD, Moorthy K et al. (2012) How reliable are clinical systems in the UK NHS? A study of seven NHS organisations. BMJ Qual Saf, 21: 466-72.
Churpek MM, Snyder A, Han X et al. (2017) Quick sepsis-related organ failure assessment, systemic inflammatory response syndrome, and early warning scores for detecting clinical deterioration in infected patients outside the intensive care unit. Am J Respir Crit Care Med, 195(7): 906-11.
Daniels R (2011a) Surviving the first hours in sepsis: getting the basics right (an intensivist’s perspective). J Antimicrob Chemother, 66(Suppl. 2): ii11-23.
Daniels R, Nutbeam T, McNamara G et al. (2011b) The sepsis six and the severe sepsis resuscitation bundle: a prospective observational cohort study. Emerg Med J, 28: 507-12.
Fleischmann C, Scherag A, Adhikari NK et al. (2016) Assessment of global incidence and mortality of hospital-treated sepsis. current estimates and limitations. Am J Respir Crit Care Med, 193(3): 259-72.
Hollnagel E, Wears RL, Braithwaite J. (2015) From safety-I to safety-II: a white paper. The Resilient Health Care Net.
Published simultaneously by the University of Southern Denmark, University of Florida, USA, and Macquarie University, Australia. [Accessed: 2 October 2017] Available from psnet.ahrq.gov/resources/resource/29228
Holmes J, Rainer T, Geen J et al. (2016) Acute kidney injury in the era of the AKI e-alert. Clin J Am Soc Nephrol, 11(12): 2123-31.
McGlynn EA, Asch SM, Adams J et al. (2003) The quality of health care delivered to adults in the United States. N Engl J Med, 348: 2635—45.
National Confidential Enquiry into Patient Outcome and Death (2012) Time to intervene? A review of patients who underwent cardiopulmonary resuscitation as a result of an in-hospital cardiorespiratory arrest.
London: NCEPOD. [Accessed: 2 October 2017] Available from ncepod.org.uk/2012cap.html
National Confidential Enquiry into Patient Outcome and Death (2015) Just say sepsis! A review of the process of care received by patients with sepsis. London: NCEPOD.
[Accessed: 2 October 2017] Available from ncepod.org.uk/2015sepsis.html
Prytherch DR, Smith GP, Schmidt PE et al. (2010) ViEWS —towards a national early warning score for detecting adult inpatient deterioration. Resuscitation, 81: 932-7.
Robinson G (2013) Providing assurance, driving improvement. Cardiff: 1000 Lives Plus. [Accessed: 2 October 2017] Available from
http://www.1000livesplus.wales.nhs.uk/sitesplus/documents/1011/Providing%20assurance%20driving%20improvement%20WEB.pdfService O, Hallsworth M, Halpern D et al. (2014) EAST: Four simple ways to apply behavioural insights. London: Behavioural Insights Team. [Accessed: 2 October 2017] Available from behaviouralinsights.co.uk/publications/east-four-simple-ways-to-applybehavioural-insights
Singer M, Deutschman CS, Seymour CW et al (2016) The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA, 315(8): 801-10.
Subbe C (2015) Safety = Design Driving safety and signposting risk. London: Betsi Cadwaladr University Health Board for The Health Foundation. [Accessed: 5 October 2017] Available from health.org.uk/sites/health/files/Betsi%20Cadwaladr%20final%20report_website%20version.pdf
Szakmany T, Lundin RM, Sharif B et al. (2016) Sepsis prevalence and outcome on the general wards and emergency departments in Wales: results of a multicentre, observational, point prevalence study. PLoS ONE 11(12): e0167230.
Weick KE, Sutcliffe KM (2007) Managing the unexpected: resilient
performance in an age of uncertainty. 2nd ed. San Francisco: Jossey-Bass.








