ICU Management & Practice, Volume 16 - Issue 1, 2016
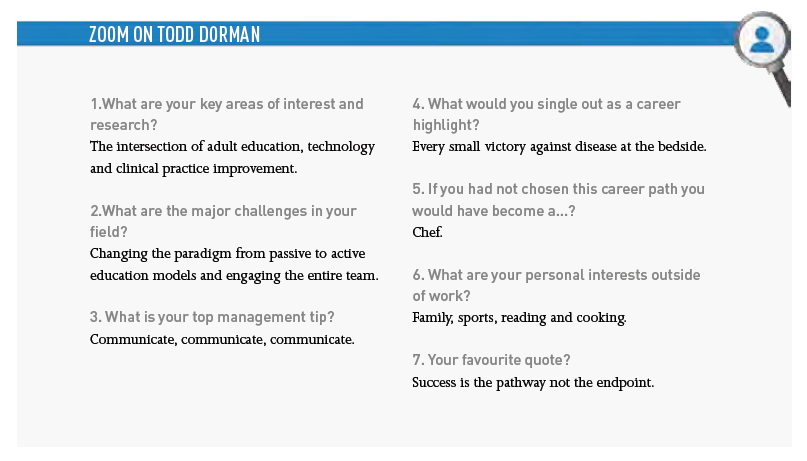
Todd Dorman takes office as President of the Society of Critical Care Medicine (SCCM) in February 2016. He is Professor of Anesthesiology and Critical Care Medicine and Vice Chair for Critical Care Services, Department of Anesthesiology/Critical Care Medicine; Senior Associate Dean for Education Coordination; Associate Dean for Continuing Medical Education at Johns Hopkins University School of Medicine. In addition he holds Joint Appointments in Internal Medicine, Surgery and the School of Nursing. He is a long-standing and valued member of the Editorial Board of ICU Management & Practice.
As you take office as President of the Society of Critical Care Medicine, what are your priorities?
I have some personal interests that I want to ensure we make progress on. These are all derived from our strategic plan, which in conjunction with our mission statement helps guide what the foci for the SCCM will be.
- For patients, the THRIVE initiative (sccm.org/Research/Quality/thrive/Pages/default.aspx) recognises that the impact of critical illness does not end at ICU discharge. It is critical that we learn what happens in our survivors so that we can facilitate their progress as well as identify opportunities to improve care during critical illness in manners that mitigate negative long-term consequences.
- The focus on sepsis in resource-limited countries is also aimed at patients and is being conducted in partnership with the European Society of Intensive Care Medicine (ESICM).
- The SCCM partnership with the Critical Care Societies Collaborative (CCSC) is focused at our own team members. We hope to advance our knowledge regarding burnout and post-traumatic stress disorder (PTSD), and thus help mitigate the occurrence of these harmful outcomes that drain our teams of experience and expertise. Interprofessional education is critical to this goal as ICUs function as integrated teams. Education by and for the team is essential to building resilience as well as for the correct execution of care in a complex environment. Interprofessional education is not simply people from different fields in the room together, but it is individuals from across the fields represented on the team interacting and learning together frequently through joint problem solving.
You recently published a paper about the implications of the U.S. Affordable Care Act for intensive care (Dogra and Dorman 2015). Please summarise your thoughts.
The Affordable Care Act will likely impact ICUs in many ways. ICUs will need to think more longitudinally about care and thus ICUs will start to think more about what happens after ICU discharge. This is but one reason why focusing at Post-Intensive Care Syndrome through the THRIVE initiative is important. Data collection and demonstration of quality outcomes will be required to negotiate reimbursements, so data-driven management strategies for the unit and the team will be important. Soft admissions will be eliminated. Clinicians will have to learn the difference between “want” and “need” and focus solely on “need” as wasted cost will not be tolerated.
What are your thoughts on how and how much clinicians from other disciplines should be involved in critical care?
Our focus should be on the competencies of the individuals. Our patients and their families deserve someone who is competent and present. We continue to have open discussions with a variety of professional societies that interface with critically ill and injured patients.
Is intensive care education fit for purpose? Is there sufficient education for the ‘soft’ skills intensivists need – management, team working, leadership etc.?
Presently there is little data specifically in the ICU environment. This is an area ripe for academic pursuit.
What are your top tips on maintaining a great team?
- Results at the pace of relationships;
- Taking the time to get to know the team members;
- Spending valuable time in the course of care not just in care. For instance, having lunch when on service with team members helps build the depth and breadth of the relationship;
- Running rounds in a true team fashion where everyone’s opinion is truly valued is critical;
- Finally, being open to feedback is not only a marker of professionalism, but helps build trust.
You have observed that a major challenge in critical care is changing the paradigm from passive to active education models and engaging the entire team. Could you expand on that?
Most physicians were taught in a passive education style. The material is presented, and you are merely supposed to digest it, incorporate it and change when appropriate. This approach contributes to the common belief that it takes more than 15 years for new information to highly penetrate care decision-making. We need our faculty taught to be active teachers that use active instructional designs. In addition, the ICU team functions as a team and so interprofessional education is required. Such education should use active approaches and be more about team problem solving, team involvement in simulation, etc. These approaches will lead to faster improvements in care, more durable change and more satisfied teams.
Can medical education be a value centre? How do you measure effectiveness of continuing medical education?
Continuing medical education (CME) provides value at many levels. There are now numerous critical reviews that have demonstrated the educational value of accredited CME as well as the potential for impact on patient care. Physicians have historically believed that when they finished training they were experts. In fact, when they finish training they are proficient. They can develop into an expert over the subsequent years through experience and ongoing active education. For instance, meaningful personal reflection is critical in the development of an expert. I bring this issue up, as under the historic model, CME was really there to serve as an awareness phenomenon. It has only really been in the last 5-7 years that CME has taken on the challenge of being integrated into quality and safety programmes and to academically assess its impact at the patient level. The early studies are quite promising in this regard. So where CME outcomes used to be participation rates and satisfaction scores, the outcomes that are now focused on include physician performance and patient/population outcomes. I should point out that historic approaches to things like Grand Rounds should not be expected to be associated with changes in practice or performance. Such sessions are much more about awareness of information, as they typically do not use active teaching or learning principles.
Could computer-assisted education be helpful in disseminating information to difficult-to reach patients?
Mobile availability will likely be the format that reaches the most. Many resource-limited environments do not have access to standard networks, but the population does have a mobile device. Such systems can facilitate delivery of actionable information to patients and can also serve as a portal for simple data collection from the patient and/or their family
References:
Dogra AP, Dorman T (2015) Critical care implications of the Affordable Care Act. Crit Care Med, Nov 12. [Epub ahead of print] PubMed







