ICU Management & Practice, Volume 16 - Issue 3, 2016
There is a significant gender imbalance in positions of leadership in intensive care medicine. This complex problem requires action to ensure high quality and sustainable leadership for our specialty in the future.
Despite an increasing proportion
of women in the medical specialty workforce, there are few female doctors in
positions of leadership in intensive care medicine (ICM). This article
explores reasons for this gender imbalance, the implications for our
specialty and potential solutions. We focus particularly on the situation in
Australasia, but present data from other regions where possible to
demonstrate that this is a widespread concern.
Where is the Balance?
In most developed countries at least half of medical school graduates are women; this has been the case for many years (Amrein et al. 2011; Filardo et al. 2016; Bismark et al. 2015). Despite this, several specialties, including ICM, continue to attract more male than female doctors.
In Australia in 2014 16.6% of ICM specialists and 35.6% of ICM trainees were women (Australian Institute of Health and Welfare 2014). In the USA in 2013, 24.3% of physicians and 33.1% of trainees in critical care medicine were women (Association of American Medical Colleges 2014). In the UK in 2012, female doctors comprised 26% of the full-time equivalent intensive care specialist workforce (Centre for Workforce Intelligence 2015).
This gender imbalance is more
marked in positions of leadership in intensive care medicine. In Australia
and New Zealand women make up only 10.5% of Clinical Directors of ICUs
accredited by the College of Intensive Care Medicine of Australia and New
Zealand (2016).
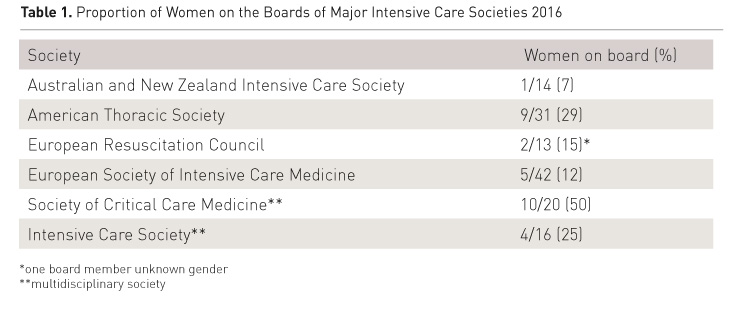
Female representation on the boards of major intensive care societies is also low (Table 1). Board membership is a key position of influence, as these societies set the academic and political agenda for intensive care medicine.
A similar pattern emerges in academic intensive care medicine. Amrein and colleagues (2011) found that women comprised 17.5% of the editorial boards of the five highest-ranked critical care journals. This was the lowest of all examined specialties, including orthopaedic surgery. Metaxa (2013) reported that between 6 and 14% of speakers at the four largest international intensive care conferences were women. Of six major Australasian specialties, intensive care medicine had the lowest percentage (8-18%) of female speakers at its annual college conferences (Modra et al. 2016).
Overall, female intensivists are not rising to positions of leadership, nor are they participating equally in the academic discourse in ICM.
It may be argued that the small number of women in leadership positions is not only expected but acceptable, given the low proportion of women within the intensive care workforce. However, in many cases female representation in positions of leadership falls short of female workforce participation (Amrein et al 2011). In addition, gender imbalance at a leadership level tends to perpetuate workforce gender imbalance, as aspiring female intensivists have few role models. Finally, we believe that increasing the number of female leaders will result in a more innovative and responsive leadership for the specialty.
See Also:ICU Admittance: Does Gender Matter?
Why Is It So?
Gender Bias
Gender biases arise from gender schemas: non-conscious hypotheses about sex differences that inform our expectations and evaluations of men and women (Valian 1998). Men and women hold the same gender schemas and use them to efficiently negotiate a complex social world. The World Economic Forum (WEF) (2016) concluded that gender bias is a leading cause of the persistent gender gap in health outcomes, economic and political participation and educational attainment.
Gender schemas lead to measurable biases against women in professional settings even when appraised against apparently objective criteria. Wennerås and Wold (1997) assessed the non-blinded peer review process for scientific grants in Sweden, using multiple regression analysis of the relation between applicants’ scientific productivity and the subjectively assigned ‘competence’ score. They found that a female applicant needed the equivalent of three additional first-author publications in Nature to obtain the same score as a male applicant. Moss-Racusin and colleagues (2012) demonstrated that men were more likely than women to be appointed to a hypothetical science faculty position, despite the male and female candidates having identical CVs.
In academic medicine Jena and colleagues (2015) report that female medical faculty members are “...substantially less likely than men to become full professors, even after adjusting for factors such as experience, specialty and research productivity.” This echoes findings that male academic physicians are promoted more quickly and receive larger salaries than female academic physicians, even after adjusting for potential confounders such as academic productivity or work hours (Jena et al 2016; Jagsi et al 2012; Nonnemaker 2000).
Bismark and colleagues (2015) explored the under-representation of women in leadership in Australian hospitals and health care organisations by interviewing male and female doctors in formal leadership roles. The majority of interviewed leaders attributed the imbalance to ‘substantial gender barriers’ including unconscious bias and a ‘club culture’, as well as structural barriers such as rigid career pathways.
The effect of gender bias is likely to be more marked in informal selection processes, such as invitations to speak at conferences or chair a committee.
The male gender schema is more congruent with the role of leader than the female gender schema: men ‘look’ more like leaders than women (Valian 1998). Women are often evaluated negatively when they display leadership qualities like assertiveness (Eagly and Karau 2002). On average female doctors receive higher salaries than male doctors when they work in traditionally female specialties such as paediatrics, and men earn more than women in male-dominated specialties such as emergency medicine (Baker 1996). Intensive care medicine is a specialty rich in technology and procedures so it is possible that the role of intensivist is more congruent with the male gender schema: men ‘look’ more like intensivists.
Bullying and Sexual Harassment
Sexual harassment and discrimination are extreme manifestations of gender bias. The College of Intensive Care Medicine of Australia and New Zealand undertook a survey of fellows and trainees regarding their experiences of bullying, discrimination and harassment in the workplace. Twelve percent of respondents reported discrimination in the past year and the prevalence of discrimination reports was twice as high among female respondents than male respondents. Three percent of respondents reported sexual harassment, and the prevalence of sexual harassment reports was three times higher among women than men (Venkatesh 2016). These problems could certainly deter women from pursuing a career in ICM.
Parental Leave
Parental leave and caring responsibilities impede the career progression of female doctors far more than male doctors. Women bear the majority of career breaks for parental leave and are more likely to work part-time (Buddeberg-Fisher et al. 2010). In addition, postgraduate specialty training often coincides with the time many people wish to have children. Some trainees have difficulty obtaining parental leave or returning to accredited training positions after their leave (de Costa et al. 2013). The impact of family responsibilities on career advancement is amplified in ICM because of the significant out-of-hours commitment required of intensivists.
Why Does it Matter?
Why should we pursue improved gender balance in intensive care medicine? It’s about ensuring high-quality and sustainable leadership in ICM for the future.
We cannot attract the highest quality leaders by recruiting from only half the pool of intensivists. The changes needed to redress the current gender imbalance—workplace flexibility and an inclusive, respectful culture—will improve working conditions for all intensivists, contributing to a stable workforce.
There is good reason to believe that improved gender balance in ICM could lead to improved patient care. Studies from the business world show that increasing the number of women on a company’s board leads to increased profit, after controlling for variables such as company size and governance structure (Smith et al. 2006; Vafaei et al. 2015). The World Economic Forum (2014) reports a correlation between female participation in the workforce and politics, and national economic competitiveness. We should consider our own ‘business case’ for diversity— measuring patient outcomes instead of profit.
Men and women bring different experiences to a leadership team, and this can expand the range of problems and possible solutions considered by the group (Vafaei et al. 2015). For example, male and female scientific journal reviewers make different editorial decisions, leading to greater variety in published material (Amrein 2011, citing Wing et al. 2010). This broadening of horizons could lead to innovative research questions and problem solving strategies. Crucially, this argument does not rest upon an expectation that women bring certain ‘feminine’ characteristics to leadership roles. Rather, diversity itself leads to decision-making that is more representative of the community served (WEF 2016).
The final answer is simple: it’s about fairness. Women should have equal access to becoming clinicians, researchers and leaders in this exciting specialty.
Solutions
Gender imbalance in ICM is a complex problem —here we outline possible solutions. Overall, creating a culture that supports gender balance will be more effective than trying to mentor individual women to succeed despite persistent systemic barriers (de Vries 2011).
Cultural Change
The first step towards enacting cultural change is to improve awareness of the problem. Regularly auditing and publishing data on female representation in all facets of intensive care medicine will increase the visibility of gender imbalance in our profession (Bonomo 2016). Gender bias training, including simple ‘self tests’ such as that developed by Project Implicit, can increase awareness of how gender bias affects us all (Project Implicit 2011).
All intensive care medicine institutions must have a ‘zero tolerance’ approach to sexist behaviour. This should be set out in easily accessible guidelines, with clear consequences for inappropriate behaviour regardless of the status of the perpetrator within the profession (Expert Advisory Committee to the Royal Australasian College of Surgeons 2015).
Overcoming Gender Bias
To minimise the impact of gender biases on leadership appointments, transparent and formal selection processes should be used (Bismark et al. 2015). Selection panels should be ‘blinded’ to gender wherever possible, for example by removing names from CVs in the initial selection process. Introducing the double-blinded peer review process led to an increase in the publication of scientific papers written by women (Budden 2008).
Another solution is to set gender-based targets or quotas for the proportion of women appointed to leadership positions, speaking at conferences or granted research funding (Bonomo 2016). The World Economic Forum (2016) reports that setting targets for recruitment and retention of female employees is a crucial strategy to improve female representation across all industries.
Quotas are controversial: some argue they undermine equality and discredit the women appointed to designated female positions. However, the measurable impact of gender biases on women’s professional advancement demonstrates that the ‘level playing field’ does not actually exist. Even in apparently objective selection processes, men are slightly more likely to be selected simply because they are male. There is evidence that aiming to appoint employees on merit alone amplifies rather than diminishes the effect of covert gender bias in the selection process (Castilla and Benard 2010). Quotas address covert bias by overtly making women more likely to be selected for some positions.
Structural Change
Structural change in the workplace is crucial for women’s integration and advancement in the workforce (World Economic Forum 2016). This includes transparent parental leave schemes accessible to men and women, workplace flexibility through flexible hours and part-time appointments. A key challenge for ICM is incorporating these changes whilst ensuring continuity of patient care.
On-site childcare in the workplace and at conferences could improve female participation, and encourage the integration of family and professional responsibilities for both mothers and fathers.
Mentoring
Mentoring and leadership training can help nurture the careers of individual women (WEF 2016). Mentoring programmes should be carefully tailored to support women, as gender biases can also affect mentoring relationships. For example, men are more likely than women to receive strategic career advice and to be recommended for career opportunities as a result of a mentoring relationship (de Vries 2011).
Advocacy initiatives
Deliberate efforts must be made to nominate or encourage talented women to apply for leadership roles, including positions on boards, committees or speaker engagements (Bonomo 2016). Initiatives such as Australia’s Women in Intensive Care MedicineNetwork can help women to develop effective professional networks and to advocate for key structural change. These initiatives must actively engage men in the change process.
Conclusion
Intensive care medicine prides itself on being a dynamic specialty, committed to continuous improvement and understanding of the crucial role of human factors in delivering effective patient care. Despite this, there is a persistent gender imbalance in the leadership of ICM. To ensure the sustainability and quality of ICM leadership in the future, we must commit to urgently redressing this imbalance through cultural change, workplace structural reforms, advocacy and mentoring.
Conflict of
Interest
All authors are members of the Women in Intensive Care Medicine network, an organisation dedicated to improving the gender balance in intensive care medicine in Australasia through research, advocacy and networking.
Acknowledgements
The authors gratefully
acknowledge the assistance of Professor Imogen Mitchell in the preparation of
this manuscript.
Abbreviations
CV curriculum vitae
ICM intensive care medicine
WEF World Economic Forum
Contact details
Women in Intensive Care Medicine
Website: http://intensivecarenetwork.com/about/win/
Email: [email protected]
Twitter:@womenintensive
References:
American Thoracic Society (2016) [Accessed: April 2016] Available from: thoracic.org/about/governance/board-of-directors.php
Amrein K, Langmann A, Fahrleitner-Pammer A et al. (2011) Women underrepresented on editorial boards of 60 major medical journals. Gend Med, 8(6): 378-87.
PubMed ↗
Association of American Medical Colleges, Centre for Workforce Studies (2014) Physician specialty data book. [Accessed 23 May 2016] Available from
members.aamc.org/eweb/upload/Physician%20Specialty%20Databook%202014.pdf
Australian Institute of Health and Welfare (2014) Medical practitioners
overview 2014 tables, Canberra. [Accessed: May 2016] Available from
aihw.gov.au/workforce/medical/2014/additional
Australia and New Zealand Intensive Care Society (2016) [Accessed: June 2016] Available from anzics.com.au/about-us
Baker LC (1996) Differences in earnings between male and female physicians. N Engl J Med, 334(15): 960-4.
PubMed ↗
Bismark et al (2015) Reasons and remedies for under-representation of women in medical leadership roles: a qualitative study from Australia, BMJ Open, 5:e009384.
PubMed ↗
Bonomo Y, Zundel S, Martin JH. (2016) Addressing unconscious bias for female clinical academics, Intern Med J, 46(4): 391-3.
PubMed ↗
Buddeberg-Fischer B, Stamm M, Buddeberg C et al. (2010) The impact of gender and parenthood on physician’s careers – professional and personal situation seven years after graduation. BMC Health Serv Res, 10:40.
PubMed ↗
Budden AE, Tregenza T, Aarssen LW, Koricheva J, Leimu R and Lortie CJ. (2008) Double-blind review favours increased representation of female authors. Trends Ecol Evol, 23(1): 4-6.
PubMed ↗
Castilla EJ, Benard S (2010) The paradox of meritocracy in organizations, Administrative Science Quarterly, 55: 543-76.
Article ↗
Centre for Workforce Intelligence. (2015) In-depth review of the anaesthetics and intensive care medicine workforce. London: Centre for Workforce Intelligence. [Accessed May 2016] Available from cfwi.org.uk/publications/in-depth-review-of-the-anaesthetics-and-intensive-care-medicine-workforce/@@publication-detail
College of Intensive Care Medicine of Australia and New Zealand. (2016) General accredited units; paediatric accredited units. [Accessed: 28 May 2016] Available from cicm.org.au/Hospitals/Accredited-Sites-Accordion/Accredited-Units
De Costa CM, Permezel M, Farrell LM et al. (2013) Integrating parental leave into specialist training: experience of trainees and recently graduated RANZCOG fellows. Med J Aust, 199(5): 359-62.
PubMed ↗
De Vries, J. (2011) Mentoring for change. Melbourne: LH Martin Institute, University of Melbourne; Universities Australia Executive Women.. [Accessed: May 2016] Available from lhmartininstitute.edu.au/documents/publications/2011uaewmentoringforchange.pdf
Eagly AH, Karau SJ (2002) Role congruity theory of prejudice toward female leaders. Psychol Rev, 109(3):573–98.
PubMed ↗
Expert advisory group on discrimination, bullying and sexual Harassment advising the Royal Australasian College of Surgeons (2015) Report to RACS. Melbourne: Royal Australasian College of Surgeons. [Accessed: 5 May 2016] Available from surgeons.org/media/22045685/EAG-Report-to-RACS-Draft-08-Sept-2015.pdf
European Resuscitation Council (2016) [Accessed: June 2016] Available from erc.edu/index.php/committee/en
European Society of Intensive Care Medicine (2016)[Accessed: April 2016] Available from esicm.org/about/structure-and-organisation/council
Filardo G, da Graca B, Sass DM et al. (2016) Trends and comparison of female first authorship in high impact medical journals: observational study (1994-2014), BMJ, 352: i847.
PubMed ↗
Intensive Care Society (2016) [Accessed: April 2016]
Available from ics.ac.uk/about-us/council-and-committee-pages/council
Jena AB, Khullar D, Ho O et al. (2015) Sex differences in academic rank in US medical schools in 2014. JAMA, 314(11): 1149-58.
PubMed ↗
Jagsi R, Griffith KA, Stewart A et al. (2012)Gender differences in the salaries of physician researchers, JAMA, 307(22): 2410-7.
PubMed ↗
Metaxa V. (2013) Is this (still) a man’s world? Crit Care, 1(1)7: 112.
PubMed ↗
Modra LJ, Austin DE, Yong SA et al. (2016) Female representation at Australasian specialty conferences Med J Aust, 204(10): 385.
PubMed ↗
Moss-Racusin CA, Dovidio JF, Brescoll VL (2012) Science faculty’s subtle gender biases favour male students, Proc Natl Acad Sci USA, 109 (41): 16474-9.
PubMed ↗
Nonnemaker L. (2000) Women physicians in academic medicine: new insights from cohort studies, N Engl J Med, 342(6), 399-405.
PubMed ↗
Project Implicit (2011) [Accessed: June 2016] Available from
https://implicit.harvard.edu/implicit/takeatest.html
Smith N, Smith V and Verner M. (2006) Do women in top management affect firm performance? A panel study of 2,500 Danish firms, International Journal of Productivity and Performance Management, 55(7): 569-93.
Article ↗
Society of Critical Care Medicine (2016) [Accessed: June 2016]
Available from sccm.org/About-SCCM/Leadership/Pages/Council-Members.aspx
Tesch BJ, Wood HM, Helwig AL et al. (1995) Promotion of women physicians in academic medicine. Glass ceiling or sticky floor? JAMA, 273(13):1022-5.
PubMed ↗
Vafaei A, Ahmed K and Mather P. (2015) Board diversity and financial performance in the top 500 Australian firms. Australian Accounting Review, 25(4): 413–27.
Article ↗
Valian V. (1998) Why so slow? The advancement of women, Cambridge, MA:
MIT Press.
Venkatesh B. (2016 June) Results from the CICM Bullying and Harassment Survey. Presentation at the Annual Scientific Meeting of the College of Intensive Care Medicine of Australia and New Zealand, Adelaide, Australia.
Wennerås C, Wold A (1997) Nepotism and sexism in peer-review. Nature,
387(6631): 341-3.
World Economic Forum (2016) The industry gender gap: women and work in the fourth industrial revolution. Geneva: World Economic Forum. [Accessed: 23 May 2016] Available from www3.weforum.org/docs/WEF_FOJ_Executive_Summary_GenderGap.pdf
World Economic Forum (2014) The global gender gap report 2014. Geneva: World Economic Forum. [Accessed: 23 May 2016] Available from www3.weforum.org/docs/GGGR14/GGGR_CompleteReport_2014.pdf









