ICU Management & Practice, Volume 18 - Issue 1, 2018
International Society for Rapid Response Systems joins with the Patient Safety Congress in 2018
The International Society for Rapid Response Systems joins with the Patient Safety Congress in July 2018 to develop new approaches to managing patients at risk of deterioration. Identification and treatment of deteriorating hospital patients is a major safety issue and cannot be managed in isolation. This event will bring the issues of the at-risk and deteriorating patient and patient safety closer together.
The Rapid Response System
The Rapid Response System (RRS) is a primarily clinician-led approach to patient safety across the hospital. It is based on achieving reliable, early identification of at-risk and deteriorating patients and timely delivery of appropriate treatments, with continuous evaluation of processes and outcomes to enable improvement. The impetus for creation of RRSs came from the observation that patients admitted to the ICU from general wards within the hospital suffer far higher mortality than patients admitted from the emergency department or the operating theatre (Goldhill and Sumner 1998). It then became apparent that failures to recognise or act on deterioration are common and a significant contributor to adverse outcomes (McQuillan et al. 1998; Donaldson et al. 2014): among patients triggering a rapid response review in hospitals around the world, 1 in 4 require ICU admission and 1 in 10 die within 24 hours (Bannard-Smith et al. 2016). It has also been found that up to a third of calls for a rapid response actually involve patients at the end of life, so the responding team must be able to provide both aggressive treatments and initiation of end-of-life care (Jones et al. 2013).
New technologies and the EU Nightingale Horizon 2020 project
Early identification of deterioration has been aided by deployment of early warning systems using combinations of vital signs to track patients’ acuity of illness and trigger escalation at designated levels of physiological abnormality; for example, the NHS National Early Warning Score, which is formally endorsed as the means to identify acutely ill patients in all hospitals in England (Royal College of Physicians 2017). New technology allows for more sophisticated approaches, and the European Union’s Horizon 2020 research and innovation programme is currently sponsoring five major hospitals across the continent to stimulate development of the ‘ultimate patient monitoring system’. This Nightingale H2020 project recently had over sixty companies submit tenders to build such systems, with nine consortia selected to go forward to the next phase. These are a mix of multinational companies and small/medium-sized enterprises aiming to use ‘real-time’ analyses of wireless monitoring of vital signs combined with patient self-reports, laboratory data, demographic details and other information from the electronic health record (see nightingale-h2020.eu). The initial focus is on high-risk patients including emergency admissions, major surgical cases and ICU follow-ups; but the ambition is to be able to monitor a whole range of hospital patients and selected patients at home in due course.
RRS outcomes
Systematic reviews of RRS effectiveness most consistently find a reduction in cardiac arrests and often a mortality reduction too (Jones et al. 2016). Suboptimal management of patients at risk of deterioration has led to the development of national guidelines and tools for tracking and responding to these situations (Royal College of Physicians 2017; Subbe et al. 2017), but ultimately the clinical skills, decision-making and team-working of healthcare practitioners determine optimal care. It has been demonstrated that the RRS can play a leading part in developing a safety-focused culture and patient-safety systems across hospitals, although it takes time for systems to mature, for barriers to be overcome, and for escalation of at-risk patients and learning from adverse events to become routine practice. An interrupted time series study of nearly 10 million patients in 232 hospitals described a progressive reduction in failures to rescue deteriorating patients, cardiac arrests and mortality from early on, and then also improved outcomes for low mortality diagnostic-related patients in the latter years (Chen et al. 2016; Pain et al. 2017). However, the response cannot occur in isolation and the system cannot survive without integration in an overall patient safety framework.
International Society for Rapid Response Systems
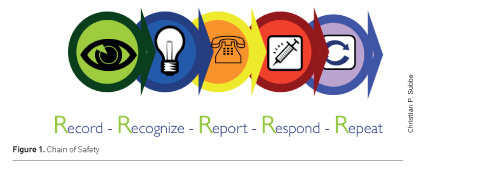
The International Society for Rapid Response Systems (iSRRS) is a global membership organisation committed to being the ultimate knowledge source for those involved in the identification and treatment of deteriorating patients and improvement of patient safety. The society is relatively new, but its founders have a body of work behind them including thirteen international conferences, two textbooks, two consensus conferences and a series of internationally conducted courses on how to establish a RRS. The first consensus conference described the essential components of the RRS including data collection and administrative arms to oversee all RRS activities and integrate these into the complex whole hospital environment (DeVita et al. 2006). The core components are methods to reliably record key patient data (vital signs, but also laboratory data and demographic information), having clear indicators enabling staff to recognise at-risk and deteriorating patients, ensuring timely report – or escalation – of deterioration; and a timely, effective response (Subbe and Welch 2013): see Figure 1.
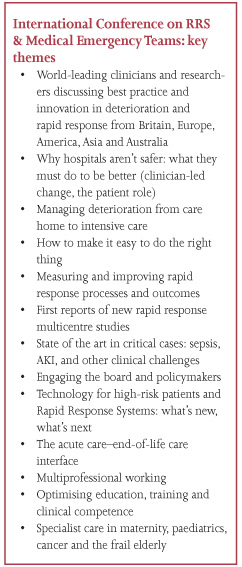
International Conference on Rapid Response Systems & Medical Emergency Teams
In 2018 the iSRRS is working together with the Health Service Journal and Patient Safety Congress to bring the issues of the at-risk and deteriorating patient and patient safety more generally closer together. The Patient Safety Congress is now in its 11th year and last year brought together over 1000 attendees. It has built a reputation as the UK’s best-regarded safety and quality improvement event by developing a high-quality programme in partnership with national and international experts, patients and frontline practitioners. The iSRRS and UK National Outreach Forum’s 14th International Conference on Rapid Response Systems & Medical Emergency Teams will be co-located with the Patient Safety Congress and Patient Safety Awards on 9th and 10th July at Manchester Central to deliver a two-day landmark event to help dramatically improve patient outcomes and safety in healthcare.
The 2018 International Conference is the key opportunity for all clinical and managerial staff interested in at-risk and deteriorating patients—together with policy-makers—to discuss international best practice in the field. There will be integrated multidisciplinary expert panels, insights into optimal clinical care of challenging patients, sharing of innovation and improvements from different settings, and a new consensus conference on the metrics needed to evaluate the whole RRS. A shared stream of content and a single expanded exhibition area open to delegates from both events will promote the sharing of ideas between clinicians, patient safety and quality improvement experts from around the world.
Note: for International Conference on RRS & Medical Emergency Teams delegate information contact [email protected] / +44 (0)20 7608 9072.
Websites for more information:
References:
Chen J, Ou L, Flabouris A, et al. (2016) Impact of a standardized rapid response system on outcomes in a large healthcare jurisdiction. Resuscitation, 107: 47-56.
Devita MA, Bellomo R, Hillman K et al. (2006) Findings of the first consensus conference on medical emergency teams. Crit Care Med, 34(9): 2463-78.
Donaldson LJ, Panesar SS, Darzi A (2014) Patient-safety-related hospital deaths in England: thematic analysis of incidents reported to a national database, 2010-2012. PLoS Med, 11(6): e1001667.
Goldhill DR, Sumner A (1998) Outcome of intensive care patients in a group of British intensive care units. Crit Care Med, 26(8): 1337-45.
Jones D, Moran J, Winters B et al. (2013) The rapid response system and end-of-life care. Curr Opin Crit Care, 19(6): 616-23.
Jones D, Rubulotta F, Welch J (2016) Rapid response teams improve outcomes: yes. Intensive Care Med, 42(4): 593-5.
McQuillan P, Pilkington S, Allan A et al. (1998) Confidential inquiry into quality of care before admission to intensive care. BMJ, 316(7148): 1853-8.
Pain C, Green M, Duff C et al. (2017) Between the flags: implementing a safety-net system at scale to recognise and manage deteriorating patients in the New South Wales Public Health System. Int J Qual Health Care, 29(1): 130-6.
Royal College of Physicians (2017) National Early Warning Score (NEWS) 2: Standardising the assessment of acute-illness severity in the NHS. Updated report of a working party. London: RCP.
Subbe CP, Kellett J, Barach P et al. (2017) Crisis checklists for in-hospital emergencies: expert consensus, simulation testing and recommendations for a template determined by a multi-institutional and multi-disciplinary learning collaborative. BMC Health Serv Res, 17(1): 334.
Subbe CP, Welch JR (2013) Failure to rescue: using rapid response systems to improve care of the deteriorating patient in hospital. Clin Risk, 19(1): 6-11.









