HealthManagement, Volume 21 - Issue 4, 2021
Healthcare needs to change to meet demographic shifts, increasing demand and rising costs. To change healthcare, success lies in its transformation of the healthcare worker for tomorrow. In the face of these disruptions and increasing adoption of automation and digitalisation, healthcare workers must be equipped to redesign their jobs and upskill themselves to drive innovation and productivity.
The Centre for Healthcare Innovation’s (CHI) systems approach to innovation called the “innovation cycle” is an iterative cycle that starts with redesigning care and processes, then leveraging technologies, and sustaining the change by redesigning jobs to deliver better care and job value. This article chronicles Tan Tock Seng Hospital’s learning journey using the innovation cycle to redesign jobs for the Healthcare Worker 1.0 to 4.0.
Key Points
- Healthcare Worker 1.0 (Individual Job Redesign) – With job redesign tools, staff can redesign their jobs and upskill themselves to perform higher value-added roles.
- Healthcare Worker 2.0 (Team Job Redesign) - Applying job redesign beyond an individual level to the team level, allowing every staff to practise at the top of their license.
- Healthcare Worker 3.0 (Transdisciplinary Job Redesign)- Increasingly, as care moves from a care facility into the community, different mental models in workforce transformation need to be explored, where one caregiver is able to provide care for a multitude of related conditions as opposed to many caregivers to one patient in a hospital.
- Healthcare Worker 4.0 (Digitally Enabled Job Redesign) - Delivering care anytime and anywhere aided by digitalisation and employing technology that would move care beyond the walls of the hospital.
Healthcare Innovation & Workforce Transformation
Healthcare systems are ramping up to meet the needs of an ageing population, growing healthcare demands and rising costs. More of the same may not be better. To redesign healthcare with new models of care, healthcare jobs need to be redesigned. In the face of disruptive change and digital transformation, there are added pressures for healthcare systems to be agile in driving innovation and renewing their workforce to sustain large-scale change. Healthcare workers want better jobs and new capabilities to redesign their jobs for the future.
The Centre for Healthcare Innovation (CHI) drives thought leadership in healthcare innovation, digitalisation and workforce transformation. A big part of transforming the workforce was to change the way we redesign, train and enable our workforce for the future. Hosted by Tan Tock Seng Hospital (TTSH), CHI serves as an open co-learning platform that encourages ideas and translates these ideas through Communities of Practice. CHI adopts a systems approach to healthcare innovation called the “innovation cycle”, an iterative cycle that starts with redesigning care and processes, then leveraging technologies, and sustaining the change by redesigning jobs to deliver better care and value.
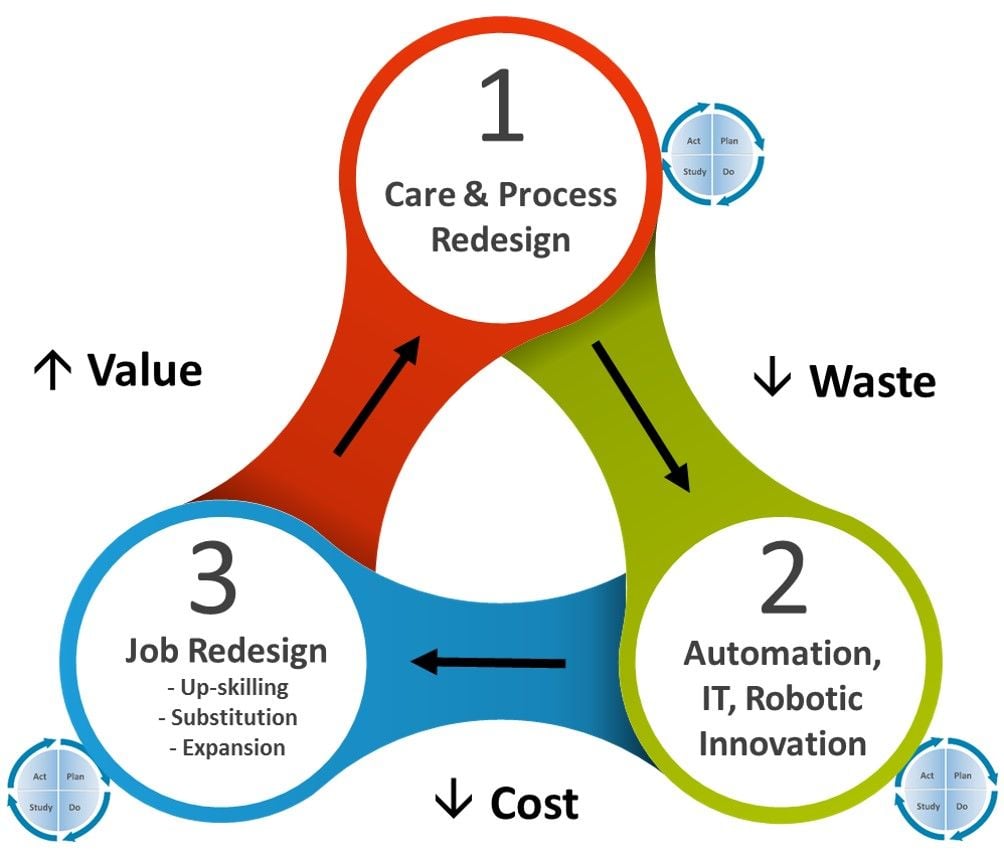
Figure 1: The Innovation Cycle
This article chronicles TTSH’s journey in using the innovation cycle to redesign jobs for the Healthcare Worker 1.0 to 4.0.
- Healthcare Worker 1.0 (Individual Job Redesign) – With job redesign tools, staff can redesign their jobs and upskill themselves to perform higher value-added roles.
- Healthcare Worker 2.0 (Team Job Redesign) – Applying job redesign beyond an individual level to the team level, allowing every staff to practise at the top of their license.
- Healthcare Worker 3.0 (Transdisciplinary Job Redesign) – Increasingly, as care moves from a care facility into the community, different mental models in workforce transformation need to be explored, where one caregiver is able to provide care for a multitude of related conditions as opposed to many caregivers to one patient in a hospital.
- Healthcare Worker 4.0 (Digitally-Enabled Job Redesign) – Delivering care anytime and anywhere aided by digitalisation and employing technology that would move care beyond the walls of the hospital.
The four levels for job redesign allow for the stacking of capabilities from Healthcare Worker 1.0 right through 4.0 in a systematic, scalable fashion. This is illustrated by the four case studies below that demonstrate how job redesign can help to anchor innovations and sustain change in transforming the healthcare workforce for the future.
Healthcare Worker 1.0: The Evolution of the Patient Service Associate
At the very heart of delivering value and quality care for patients and community, is the individual healthcare worker. At Healthcare Worker 1.0, transformation focused on the individual level by redesigning better value jobs in healthcare.
TTSH redesigned the jobs for our frontline Patient Service Associates (PSA). PSAs are administrative staff who are tasked to attend to and manage patient administration from handling enquiries, performing registration, making appointments, coordinating care and collecting payments. At the clinics, they perform front desk services and assist our doctors in the consultation process. In the wards, they provide administrative support for inpatient care. It was challenging to retain PSAs given the work scope and also the lack of upskilling opportunities and career progression.
Their job redesign was championed by PSAs themselves through a hospital-level committee. PSAs knew their job best and therefore, were in the best position to redesign their jobs given the right tools and support. The committee was constituted to transform the job scope of PSAs, enhance their career development, create a strong PSA identity and engage PSAs in doing so. The committee comprised PSAs from across the hospital and was chaired by a PSA leader with the Chief Operating Officer. Hospital Operations and Human Resources were key to ensure the work done by the committee was supported and scaled. The Hospital union was engaged early and played an important role in supporting the efforts of the PSAs.
The job redesign for the PSAs was part of a larger innovation cycle to transform our clinics and wards, where the processes were first redesigned and technologies adopted to reduce the manual tasks associated with patient administration like self-registration kiosks to digital applications. This enabled PSAs to redesign and upgrade their jobs to perform new value-added services. PSAs were trained and certified to perform up to 21 Value-Added-Services (VAS) such as phlebotomy, electrocardiograms and basic eye tests, tasks that were previously performed only by nurses.
With the redesigned jobs for PSA, the committee recognised that PSAs are professionals with new capabilities and career development aspirations. The hospital developed three distinct career development pathways for its PSAs:
(i) Management and Administration
(ii) Training and Development, and
(iii) Clinical
The suite of VAS were differentiated into the three career development pathways. Initially offered to only high-performing PSAs, these VAS are now integrated into the PSA’s staff competency framework, aligned with opportunities to develop focus in one of the three career pathways. The competency framework also recognises that PSAs need to be equipped with interpersonal skills in addition to technical skills, to do their job well.
Opportunities are also provided for PSAs to participate in other hospital-level committees, to develop and hone their leadership skills. They undertake roles and responsibilities that involve the various professional groups within the hospital and span across the hospital’s various settings. Job rotations for PSAs within the organisation have also been introduced.
Since implementation, the attrition rate of PSAs has dropped by 50 percent with increased job satisfaction. Ultimately, PSA job-redesign and upskilling led to increased productivity and decreased headcount growth for both PSAs and Nurses.
Healthcare Worker 2.0: Team-Based Job Redesign
An example of team-based job redesign towards Healthcare Worker 2.0 would be the workforce transformation undertaken by the Singapore Integrated Diabetic Retinopathy Programme (SiDRP).
Before the programme was launched, the reading of retinal images was done by Polyclinic doctors during lunchtime or after working hours, and the results would be communicated to the patients within two to four weeks. However, there were no harmonised grading criteria and guidelines at the national level.
To improve the efficiency of DRP reporting and standardise grading standards, the National Healthcare Group Eye Institute (NHGEI) at Tan Tock Seng Hospital collaborated with the Singapore National Eye Centre (SNEC) and Integrated Health Information Services (IHIS) to set up SiDRP in December 2013. The objectives were to improve the level of screening standards and turnaround time; provide uniform assessment and referral guidelines for DRP reporting at the national level, and standardise training and audit governance for DRP reporting.
To empower the clinical programme and leverage the introduction of teleophthalmology in the reading of retinal images, the NHGEI undertook a team-based job redesign of its workforce. This workforce transformation was key to optimise resources, improve turnaround time, and enable staff to perform at the top of their license.
The SiDRP reporting process required three levels of graders:
- The primary grader to assess and provide the report
- A secondary grader to re-assess and provide the report when the primary grader is in doubt
- An arbitrating grader to arbitrate both reports and make the final call, if reports by both the primary and secondary graders differed.
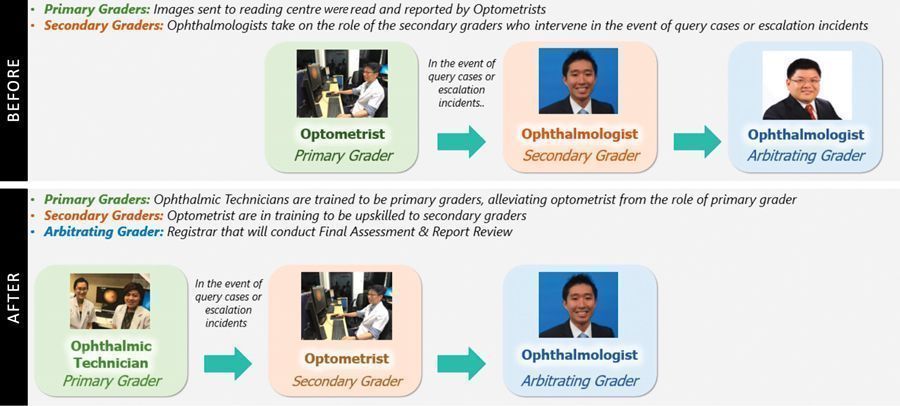
At the start of the SiDRP programme, the role of the primary grader was taken on by Optometrists, who would send their graded images to the Ophthalmologist (secondary grader) when there was doubt or a clinical indication for escalation. The secondary grader would make an assessment, and if the two reports differed, a more senior ophthalmologist would be brought in to act as the arbitrating grader.
Through team-based job redesign, PSAs were trained to take over the running of certain eye diagnostic tests usually performed by ophthalmic technicians, once again using the VAS platform. In turn, ophthalmic technicians were trained to be primary graders, while optometrists were upskilled to become secondary graders. Ophthalmologists then focused primarily as arbitrating graders and treating complex cases. This disruptive innovation across the team was enabled by job substitution, bottom-up. This is how team-based job redesign for Healthcare Worker 2.0 can stack up on the individual job redesign for Healthcare Worker 1.0.
Healthcare Worker 3.0: Therapy Assistants Job Redesign in the Community Space
In Singapore, Therapy Assistants (TA) generally work within the confines of the professional group they are employed in. TAs work in physiotherapy, occupational therapy and other allied health professional groups. The advantage of this is that they can develop deeper skills to deliver highly specific care and this serves well in settings of team-based interprofessional and multi-disciplinary hospital settings. In the community space where patients’ medical conditions are more stable and care needs more multi-dimensional, TAs with trans-disciplinary competencies would be able to maximise each contact and opportunity with the patient. Patient’s needs could be provided in a more holistic way and in a timely manner, avoiding excessive hand-offs or multiple visits. From a system’s perspective, manpower deployment becomes more efficient and resilient, and costs of care more sustainable.
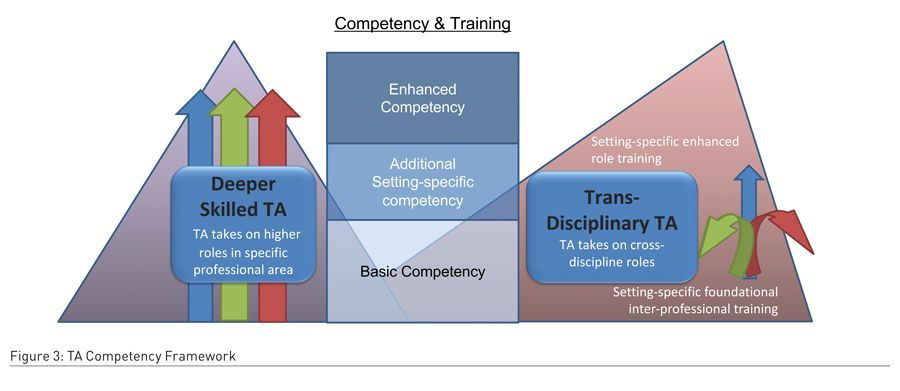
The TTSH Allied Health and Pharmacy Division developed a stacked job redesign approach that comprises deeper-skilling for the individual as Healthcare Worker 1.0 and multi-skilling for transdisciplinary care as Healthcare Worker 3.0. This dual approach enabled Allied Health TAs to practice independently in the clinical areas of higher acuity and holistically in the community. This is illustrated in Figure 3 above.
With multi-skilling, TAs are trained to practise as broad-based transdisciplinary therapy assistants to support patient care in the community. Having such trained staff providing care in the community is important because they provide greater ease and flexibility of deployment, enhanced training, ability to perform higher functions and the potential to conduct independent casework. This is a transformative shift from Many to One in the hospital setting to One to Many in the community.
To enable transdisciplinary job redesign, the division first looked into common physical care needs of the patients across allied health professionals. The team aligned the TA competencies across three different therapy departments – physiotherapy (PT), occupational therapy (OT), speech therapy (ST) – and three different settings (hospital, rehabilitation and community). Based on this, a concerted training programme that focused on the teaching of ten identified common competencies that span across the three professional groups was developed. Following the development of training materials, the departments started to train all new TA recruits with the aligned training syllabus.
Two interesting pilots are ongoing to further build upon the job redesign for TAs. First, in the sub-acute and rehabilitation setting, where a small team of transdisciplinary TAs conduct group circuit classes for inpatients. Second, in the acute hospital setting, where an integrated transdisciplinary approach has been adopted by physiotherapists and occupational therapists to assess and perform common basic therapy for patients whose medical conditions have largely stabilised and present with generic care needs. Further discussions are ongoing with Nursing to enable more transdisciplinary job redesign opportunities.
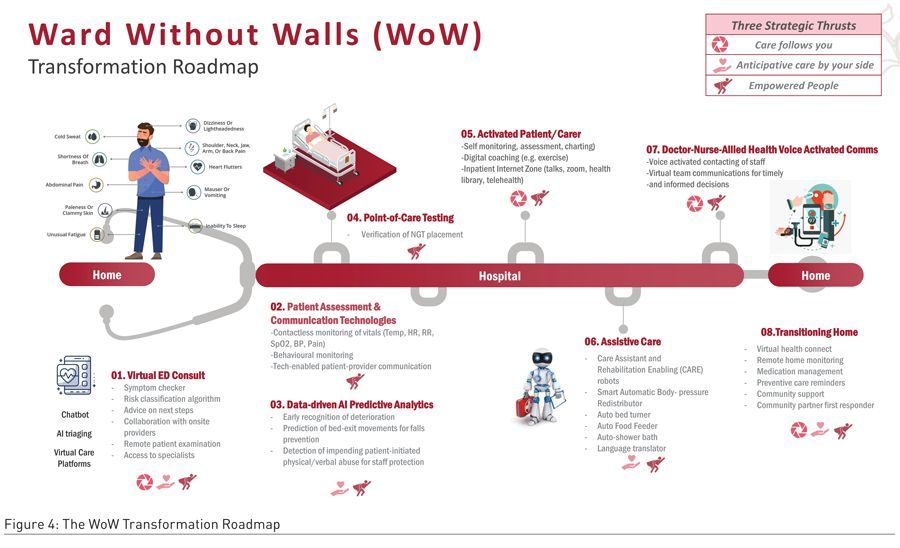
Healthcare Worker 4.0: Digitally Enabled Job Redesign that empowers Wards Without Walls
Patients transit from home to the hospital when hospital care is needed and returning home thereafter. This is the model of building a relationship-based model of care for the population to enable an H3 journey of Home-Hospital-Home. TTSH’s inpatient transformation journey began in 2010 with the redesign of nursing care in the Wards of the Future (WoF). This decentralised the central nursing counter and embedded nurses in patient cubicles to be more proximal to their care needs. It also sought to reduce non-value-added tasks in order to increase the time spent with patients. This is further augmented by the adoption of technologies such as RFID-tagging of patients, wireless vital signs monitoring, electronic discharge tracking system, inpatient pharmacy automation system to improve safety and reduce manual tasks. Further innovations with nurse-led ward rounds and ward resource nurses were critical to best coordinate and anchor inpatient and post-discharge care.
Ward without Walls (WoW) is the next phase and an extension of WoF to enable a full H3 journey for patients. WoW adopts 3 principles: Patients are Carers; Care Transformation; and Care is a Transition. The focus is on ensuring seamless care delivery beyond the hospital and providing patients and their caregivers the necessary tools to take charge of their care journey. Digitalisation is a key enabler for the H3 journey, supported by a spectrum of technologies from Artificial Intelligence (AI) and analytics, digital applications, virtual care platforms, robotics etc., coming together as a coordinated system. It would reduce our reliance on manpower, yet level up the quality of care and value that we would be able to deliver to our patients, enabled by a digitally enabled workforce i.e. Healthcare Worker 4.0.
Inpatient falls were common yet complex challenges that influenced hospital care, particularly in elderly patients. More than one-third of inpatient falls cause injuries such as fractures and head trauma, which could be a heavy burden in terms of medical, financial and social outcomes. Falls that do not result in injury may consequently cause distress and anxiety to patients, next-of-kin and healthcare teams. It may lead to restriction of future activity, further losses of strength and lastly, independence. Traditional solutions such as bed-exit sensor mats or motion detectors could be inaccurate and were cumbersome to deploy with no automation or smart features. Nurses usually suffer from alarm fatigue and end up shelving such technologies.
Through an innovation project, TTSH co-developed the PreSAGE Falls Prevention System - a smart bed-exit prediction and prevention system based on thermal sensing. Trained on 12,000 hours of real patient thermal data, PreSAGE provided accurate early warning based on machine learning models that predict bed exit. An alarm was triggered whenever a positive bed-exit was predicted and provided more response time (as compared to current sensor mat system) for nurses.
The alarm would be automatically disarmed whenever a nurse was detected near the patient’s bedside, and armed automatically when patient was alone. This feature removed the burden of remembering to arm/disarm the system alarm, which was required in a number of traditional surveillance systems, making it a user-friendly smart system.
PreSAGE could operate continuously regardless of lighting and environmental conditions, was non-contact and most importantly, non-intrusive. Thermal data provided crisp and clear silhouettes of objects detected, but do not show sensitive information such as facial or body features. The system has been deployed in TTSH’s general wards, with studies that show 97 percent sensitivity and 100 percent specificity. The system requires minimal maintenance, easy setup and projects to save up to 30 percent Nursing FTE for falls prevention surveillance.
“Transforming Care Beyond Boundaries” is the next phase of TTSH’s inpatient care transformation journey. The WoW Transformation Roadmap provides a structured way to move through the many initiatives and manage the WoW transformation efforts needed to realise success in creating a digitally-enabled workforce. Patient’s journey will be connected as one, where there will be a smooth and timely flow of information between home, hospital, and the community. This ensures that the care follows the patient regardless of care setting.
Redesigning Healthcare Jobs for the Future
The Innovation Cycle enables a systems approach to Healthcare Innovation – Care Redesign, Enabling Technologies and Job Redesign. Through job redesign, we can sustain and scale the change by empowering our Healthcare Worker with better jobs. The four levels of job redesign for Healthcare Worker 1.0 to 4.0 illustrate the ability to stack up job redesigns from individuals to teams to transdisciplinary to digitally enabled healthcare workers. This is the future of healthcare, where every healthcare worker owns his job and can change his job to deliver better care and better value.
Conflicts of Interest
None.


![Tuberculosis Diagnostics: The Promise of [18F]FDT PET Imaging Tuberculosis Diagnostics: The Promise of [18F]FDT PET Imaging](https://res.cloudinary.com/healthmanagement-org/image/upload/c_thumb,f_auto,fl_lossy,h_184,q_90,w_500/v1721132076/cw/00127782_cw_image_wi_88cc5f34b1423cec414436d2748b40ce.webp)









