An overview of the application of personalised medicine in cardiology and the potential benefits it offers for improved cardiovascular care.
The term “personalised medicine” was first introduced in the late 1990s. The Council of Advisors on Science and Technology of USA defined personalised medicine as “the tailoring of medical treatment to the individual characteristics of each patient. It does not literally mean the creation of drugs or medical devices that are unique to a patient, but rather the ability to classify individuals into subpopulations that differ in their susceptibility to a particular disease or their response to a specific treatment. Preventive or therapeutic interventions can then be concentrated on those who will benefit, sparing expense and side effects for those who will not” (PCAST 2008).
Personalised medicine has made great strides in the treatment of cancer. But the same cannot be said for cardiovascular disease. When we talk about cardiovascular disease and precision medicine, we mean an approach to CVD prevention and treatment that is based on the patient's genetics, lifestyle, and exposures.
Over the years, significant focus has been placed on increasing awareness about measures that can prevent the onset of cardiovascular disease. These measures include lifestyle modifications, and the use of evidence-based therapies. However, despite this focus, cardiovascular diseases continue to be the leading cause of disease burden and deaths worldwide. There are approximately 92.1 million adults in the US alone who have been diagnosed with cardiovascular disease. It is projected that by 2030, 44% of the adult population will have this diagnosis (Leopold and Loscalzo 2018).
Cardiovascular disease is quite complex. The traditional approach of treatment of cardiovascular disease currently focuses on treating large patient groups with similar therapies. The focus at present is to treat established cardiovascular disease without addressing individual characteristics. But now, with the advancement in panomics and a greater focus on data analysis, clinicians can personalise treatment based on clinical, biological, and molecular phenotyping. Precision medicine could thus be a more effective strategy to prevent and treat cardiovascular disease. This strategy would be based on genetics, exposures, lifestyles and health factors. Based on these elements, clinicians will be able to determine the optimal treatment strategy for the patients.
The effective application of personalised medicine in cardiology could help ease the burden of cardiovascular disease and would also provide a more comprehensive solution for its prevention and treatment. This would include a) the traditional risk factor assessment, overview of family history, and diagnostic testing); b) genetic testing; c) proteomics to identify novel biomarkers; and d) identifying personalised treatment solutions (Moo-Sik et al. 2012).
The practical application of personalised medicine would require an analysis of a patient's genetic makeup, family history, and genetic information as well as the effect of the disease on the patient. Extrinsic factors such as smoking and air pollution would also have to be considered. Other external factors such as poverty, difficulty in access to care, inadequate care, etc. should also be taken into account since they have an impact on morbidity (Ruben 2011). Cardiovascular disease increases the health burden globally as well as the total cost of care. The use and application of personalised medicine for the treatment of cardiovascular disease makes perfect sense because genetics is an important contributor. However, its application in cardiology still faces some challenges. While the use of genomics research is already happening, there is still a need to understand that as far as cardiovascular disease is concerned, there are other factors that must be considered. As already stated, cardiovascular disease is complex; there are multiple interactions between genes, environmental factors, and socioeconomic factors that must be considered. There is also a need to better understand epidemiological issues. We are still focused on the treatment of cardiovascular disease whereas what we need is an increased emphasis on prevention.
Personalised medicine still has a long way to go. The healthcare regulatory system related to the use and application of personalised medicine is still in its infancy. There is still a lot that needs to be done with respect to the development of appropriate healthcare technologies that could potentially make the theoretical benefits of personalised medicine a reality. Finally, we still need to align research efforts in this area with investment and education.
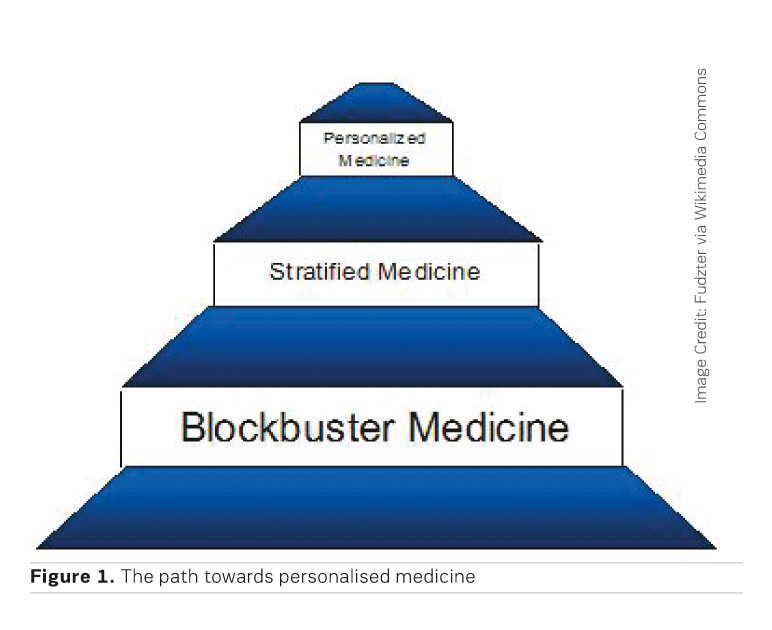
The path to personalised medicine is a stepwise process. We've already crossed the first step - that of developing blockbuster medicines, and we are currently moving towards stratified medicine, which involves the identification of subgroups of patients with clearly identifiable manifestation of disease, or have demonstrated a certain response to treatment. The next step in this journey is personalised medicine (Figure 1). We are not there yet, at least not in cardiology.
This discussion is not meant to dismiss personalised medicine. On the contrary, it has the potential to completely change the way we perceive cardiovascular disease. But in order to be able to do so, we still have to utilise the right people, identify the relevant areas of research, focus on connecting and linking genetics with other factors and come up with solutions that are not only geared towards treating cardiovascular disease, but preventing it.
Conflicts of Interest
None.
Key Points
- Personalised medicine refers to the tailoring of medical treatment to the individual characteristics of each patient
- There are approximately 92.1 million adults in the US alone who have been diagnosed with cardiovascular disease. By 2030, 44% of the adult population will have this diagnosis
- Application of personalised medicine in cardiology would include a) the traditional risk factor assessment, overview of family history, and diagnostic testing); b) genetic testing; c) proteomics to identify novel biomarkers; and d) identifying personalised treatment solutions.
- The path to personalised medicine is a stepwise process. The first step is blockbuster medicine, followed by stratified medicine, and then personalised medicine.