The new role of hospitals and the triple aim challenge.
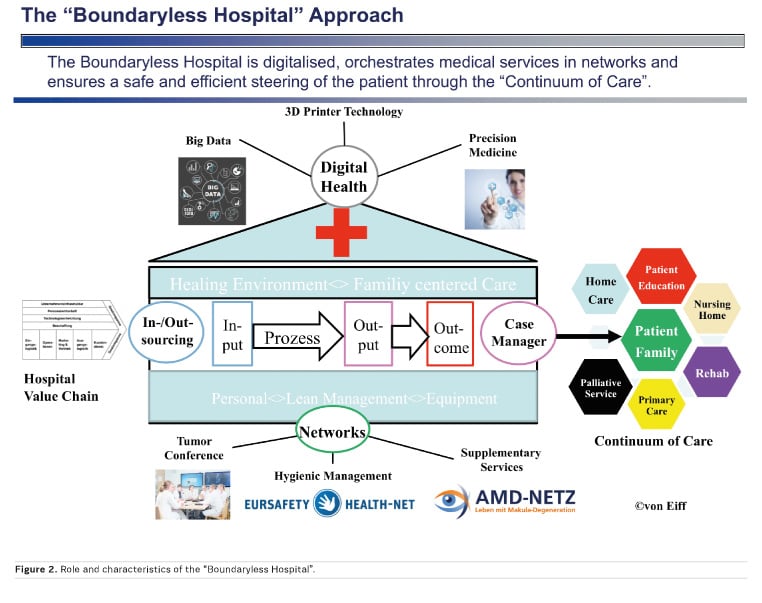
The concept of the boundaryless hospital, in combination with the value chain approach, provides the theoretical basis for an effective and efficient network design.
Initial situation
The highly developed healthcare systems of the western countries will, generally, face similar challenges over the next five to ten years. These include:
- The phenomenon of an ageing society which is causing a rising number of multi-morbid patients
- The increase of age-related diseases
- In addition, a rise in the number of chronic diseases, especially those related to an unhealthy lifestyle (work stress, poor nutrition, lack of activity)
- Medical-technological progress will enable more precise diagnoses and innovative intervention techniques, which also makes it possible to treat aged people more effectively
- A growing mentality of entitlement among patients regarding the diagnostic and treatment potential of modern medicine
On the one hand, these trends will undoubtedly contribute to a rising demand for qualified health services. But on the other hand, strict financial limitations narrow the policy option for healthcare provision. Moreover, ethical questions arise and dominate the discussion surrounding the ethics and equity of health services distribution and the limits that medical interventions have to respect. There are many questions. Should we administer any medical service to patients that we basically can?; do the economic factors override the medical aspects?; is rationing an appropriate approach for balancing an excess demand for health services and the limitations of financial resources? These questions will have a central impact on the design of medical service structures in the future. In other words, the increasing demand for state-of-the-art medical services, performed in a healing environment, has to be achieved with limited budgets.
Against this background, it is necessary for a viable structuring of the health care system in future, to find medical supply forms that:
- Conform to patients’ expectations
- Ensure the fair distribution of effective evidence-based medicine to the community and
- Integrate innovative treatment into the healthcare system in a way that ensures clear benefits and financial viability
These organisational forms of provision, which focus on therapeutic effectiveness and efficient use of resources, require the goal-driven cooperation of different medical specialists.
Therefore, the economic component, as a design parameter for medical service structures, plays a more and more important role. As a consequence, the successful organisation and management of a hospital requires:
- A patient-centred medical service portfolio, which is strictly oriented to the needs of the healthcare market
- Offering selected, highly specialised and innovative medical services (“lighthouse” performance), as well as state-of-the-art care provision for the basic medical needs of the population in a limited catchment area
- Strict orientation of the design of internal processes to patient needs
- Goal-driven and economic cooperation with highly qualified external partners who are capable of contributing to the successful treatment of patients suffering from complex diseases
- A holistic approach to the diagnosis and treatment of patients along the care continuum and
- Assurance of complementary treatments for multi-morbid patients.
The “Triple Aim”
In order to master the future challenges the developed healthcare systems are faced with (increase of elderly people, multi-morbid patients and chronic diseases, cost pressure, technical progress in medicine, entitlement mentality of patients) the provision of medical care has to be organised in networks, which interconnect primary care services with acute care treatment, rehabilitation and elderly care (especially home care based on telemedicine, health apps and digitalised monitoring devices).
Healthcare policy should extend medical provision to the community and must focus the care approach on populations.
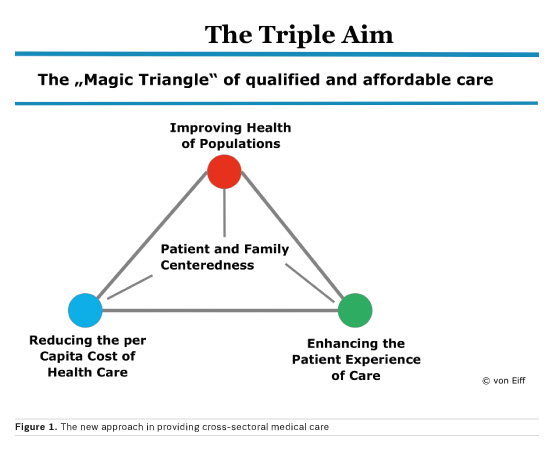
The “New Magic Target Triangle” of health policy (The “Triple Aim Approach”; see Figure 1) consists of three components:
“Patient Experience” expresses the requirement of providing high medical quality as well as excellent service performance for patients and relatives. This relates to the obligation to steer the patient smoothly through the continuum of care via case managers and addresses that quality of care inside a hospital is significantly influenced by the design of architecture, the interior fittings, the milieu, the process organisation, the corporate culture and the hygiene management
The second component of the target triangle pertains to the preventive improvement of the general health status of the entire population inside a community and relates to well-defined treatment pathways for selected populations of patients with complex and/or chronic diseases (eg diabetes, arthritis, coronary diseases)
The third component takes aim on securing a sustainable financing of medical services, contains a value-based reimbursement (pay-for-performance) and claims rules for patient compliance and copayment.
This “Magic Target Triangle” gives orientation for future healthcare provision and requires hospitals to overtake a new role in the continuum of care offering integrated services and ensuring best-in-class medicine by coordinating specialist care in networks: in short, the hospital of the future will become “boundaryless”.
The boundaryless hospital approach
The boundaryless hospital is patient-oriented, provides a safe environment, the medical knowledge is state-of-the-art and limited resources are used in a goal-oriented (effective) manner and without waste (efficient). Furthermore, the boundaryless hospital overcomes typical negative characteristics of hospitals: multi-bed rooms, lack of privacy and lack of patient autonomy. Therefore, the boundaryless hospital approach incorporates the mission of transforming a typical healthcare setting into a healing environment that improves patient outcomes and employee motivation through the creative use of evidence-based design (M.C. von Eiff 2007).
The boundaryless hospital offers a medical service portfolio alongside the continuum of care, orchestrates cross-sectoral treatment processes by using case managers and information technology (digital health, telemedicine, health apps) as a leverage for optimising clinical processes and services.
The procurement philosophy is oriented to life-cycle costs and patient benefit of a medical device and not driven by purchasing at the lowest possible price level.
Internal boundaries, caused by a silo mentality between professions and departments, with the consequence of poor communication and process inefficiency, are torn down by interdisciplinary delegation, centre organisation and an incentive system that connects both ethical and economic decision criteria.
To realise external integration, approaches like telemedicine, cluster strategy, portal clinics, networks for infection prevention, emergency supply and managed care concepts are used. The basis for a structured implementation of these concepts is the value chain approach.
The medical value chain approach refers to the sequence of supply stages for the complete treatment of a disease (eg cardiovascular diseases; diabetes) with regard to the individual and personal situation of the patient. The medical value chain is defined independently of institutions.
The hospital value chain (Porter and Teisberg 2006) includes all internal and external resources and institutions which are necessary to treat a disease comprehensively. This value chain approach focuses on the division of labour between medical service providers and aims at the appropriate design of outsourcing, cooperation and networks as supply forms.
Networks in medicine and the health business: the “boundaryless hospital” as network coordinator
Networks in medicine constitute a specific organisational type for providing a population or group of patients with healthcare services. The added value of networks, in comparison to individual (centralised) forms of supply organisation results from the following medical and economic aspects:
- Networks are virtual knowledge centres. They mobilise and distribute expert knowledge and make it broadly available
- Networks create near-to-patient services by dividing up specialised tasks and continuous medical care duties in a capability- and demand-oriented manner
- Networks enable resource sharing and ensure secure investments and utilisation efficiency
The benefit of networking between medical service providers in the healthcare system is not only motivated by a desire to improve quality or to optimise resources, but is also fostered considerably by the intention of saving costs. So, it is indicated that a medically efficient and cost-effective cooperation along the value chain (in the sense of the patient care process from initial treatment until the completion of follow-up treatment) is supported by networks.
The aim of networks is to:
- Increase patient/customer satisfaction (Nagyrapolt 2002)
- Improve patient’s well-being (patient outcome)
- Decrease costs per case
- Optimise the patient’s pathway through the entire healthcare system in a case-oriented manner, meaning shortening the process and simultaneously performing it at lower cost
- Increase the quality of medical and social care of patients (and relatives) by mobilising the best medical know-how, as well as nursing and physiotherapeutic capabilities
- Improve image so as to develop a brand status
The portal clinic as an element of a referral physicians network
Portal clinics (Münch and Scheytt 2014) are of particular importance for providing a comprehensive supply of medical services (also for highly specialised ones). Such clinics are highly-qualified primary/secondary institutions for health services, which provide precise diagnoses in order to decide whether or not a patient needs a specialised treatment. They are associated with specialised clinics (eg pulmonary/thorax surgery; neurology; etc.), qualified service providers (eg radiology centres) and maximum providers by a telemedical IT infrastructure. Patient records are documented and distributed electronically. This enables fast and precise diagnoses, second opinion consultations via conference calls and targeted acute care. Portal clinics are also of particular importance in emergency care. They give first aid in trauma networks with telemedical connections to maximum care providers.
Integrated cross-sectoral supply models
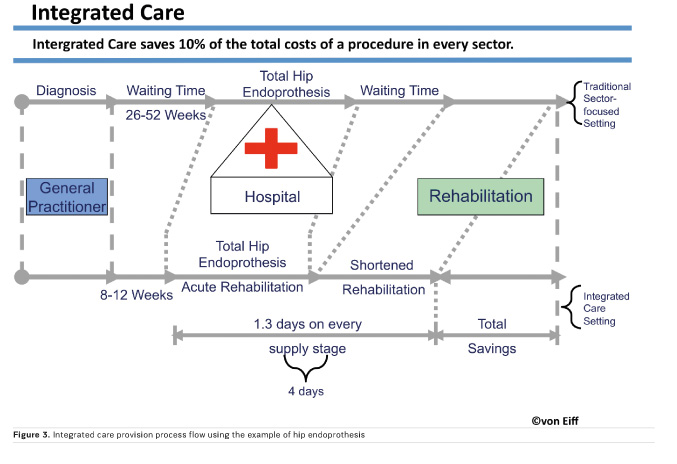
Cross-sectoral supply models (Preusker 2015) reflect a strategy of bundling the entire medical service portfolio, which is necessary to treat a disease cross-sectorally and comprehensively, subject to uniform control at a single site or in a single region. These are diseases which on the one hand have an elective character and for which the treatment process can easily be standardised (eg total endoprothesis). On the other hand, these medical provision concepts enable new forms of care for treating multi-morbid patients or those with complexity levels which require intensive medical care in the acute and rehabilitation sector (eg stroke treatment, cardio-surgical patients, transplantations).
Contracts of integrated care
Primary care by family practitioners or specialist physicians, diagnosis and treatment in acute care, rehabilitation and outpatient follow-up are cross-sectorally integrated and allocated to a central case management, which leads to shortened stays in the system, with a simultaneous decrease in treatment costs.
Such care is the basic idea behind integrated care contracts (Fig. 3). Diagnosis, therapy and rehabilitation are integrated and achieved without unnecessary waiting times. Follow-up home services enable an earlier discharge.
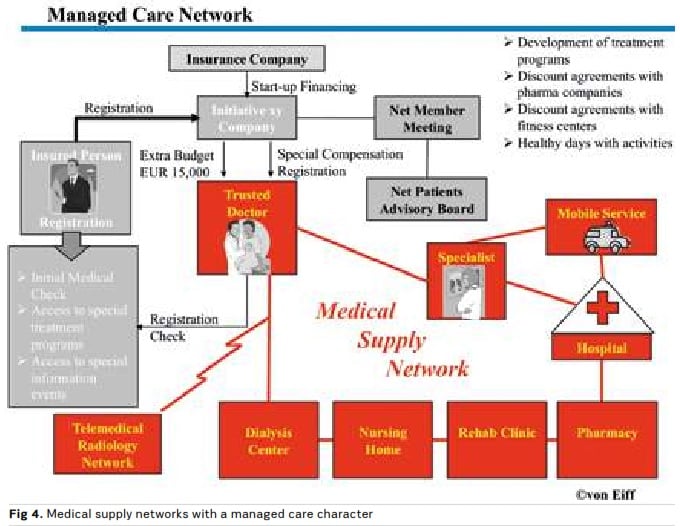
The integrated care net: supply with managed care character
The integrated supply net (Fig. 4) connects medical service providers of different specialisations with the aim of treating diseases without high complexity levels, so as to provide appropriate care and treatment at comparably low cost.
On the one hand such network structures connect medical service providers at different supply stages (family practitioner, hospital, rehabilitation clinic, nursing home, etc.). On the other hand, the medical service portfolio of such networks is the basis for insurance services, which can be obtained at particularly favourable conditions (Herzlinger 1997). Accordingly, the insurance service can be offered together with the medical service from a single source (in a single-contract package = managed care principle). Telemedical services are increasingly integrated into such managed care concepts (Kaufmann 2014).
The road ahead
Networks in medicine are a powerful form of organisation for meeting the challenges of the ageing society, medical and technological progress, as well as the increasing number of more both medically and behaviorally demanding patients. Networks are the organisation of choice, if complex illnesses are to be treated effectively.
Furthermore, networks can be built and steered by financial incentives. Such managed care networks give patients the choice between different insurance options in combination with the option to request treatment only by selected physicians under contract with a health maintenance organisation.
Networks contribute toward enhancing medical quality for the broader population and specific patient groups and toward simultaneously containing costs in the health system. The “Boundaryless Hospital” plays a pivotal role in network medicine and drives the cross-sectoral digitalisation of medicine along the continuum of care.