The human oral cavity hosts a diverse array of microorganisms, most of which are symbiotic with the host. However, some microbes, known as colonising opportunistic pathogens (COPs), can pose significant health risks under specific conditions. These pathogens are generally of low abundance and harmless in their natural niche but can become virulent when they translocate to other body sites. This phenomenon has been linked to various chronic and acute diseases, ranging from systemic illnesses like diabetes and Alzheimer's disease to acute infections such as pneumonia and sepsis. This article delves into the nature of oral COPs, with a particular focus on the Klebsiella species, exploring their potential to cause severe infections and the broader implications for public health.
Oral COPs and Their Role in Disease
The oral microbiome includes several COPs, such as Streptococcus pyogenes, Streptococcus pneumoniae, and Haemophilus influenzae. These bacteria are typically part of the normal oral flora, coexisting peacefully within the microbial community. However, they can become pathogenic under certain conditions, leading to diseases such as streptococcal pharyngitis, pneumonia, sepsis, and meningitis. The process by which these bacteria transition from benign colonisers to harmful pathogens involves several factors, including changes in the host's immune status, the presence of other microbial species, and the bacteria's ability to translocate to other body sites.
Oral bacteria have been implicated in a range of chronic systemic illnesses. For instance, the translocation of oral bacteria to the bloodstream can lead to bacteraemia, a condition that has been associated with cardiovascular diseases, including atherosclerosis. Similarly, the migration of these bacteria to the lungs or gastrointestinal tract can exacerbate conditions like chronic obstructive pulmonary disease (COPD) and inflammatory bowel disease (IBD). Understanding the mechanisms that drive these bacteria from a harmless state to pathogenicity is crucial for developing preventive and therapeutic strategies.
Klebsiella Species: A Case Study in Oral COPs
Among the oral COPs, Klebsiella species, particularly Klebsiella pneumoniae, stand out due to their pathogenic potential and antibiotic resistance. Klebsiella species are typically low in prevalence within the oral microbiome but are consistently present as part of the community. They have a pronounced ability to colonise and persist, particularly in nosocomial environments, where they can be a significant cause of hospital-acquired infections. These infections are often severe and include pneumonia, urinary tract infections, and septicaemia, primarily affecting immunocompromised individuals and critically ill patients.
Klebsiella pneumoniae is notable for being one of the ESKAPE pathogens—a group of bacteria known for their ability to escape the effects of antibiotics. This resistance makes Klebsiella infections particularly challenging to treat. The bacteria possess several virulence factors, including capsule formation, siderophores, and endotoxins, which enhance their ability to cause disease. Moreover, Klebsiella species can harbour various resistance genes, including those for beta-lactamases, making them resistant to a broad spectrum of antibiotics. This resistance is often mediated by plasmids, which can be transferred between bacteria, spreading resistance genes across microbial communities.
Survival Mechanisms of Klebsiella Species
Klebsiella species exhibit remarkable resilience and adaptability, allowing them to survive in various challenging environments. One crucial survival mechanism is their ability to withstand desiccation and other environmental stresses. Studies have shown that Klebsiella species can persist on abiotic surfaces, such as hospital sinks and drains, for extended periods. This persistence is facilitated by their ability to form biofilms, a protective layer that shields the bacteria from environmental stresses and antimicrobial agents.
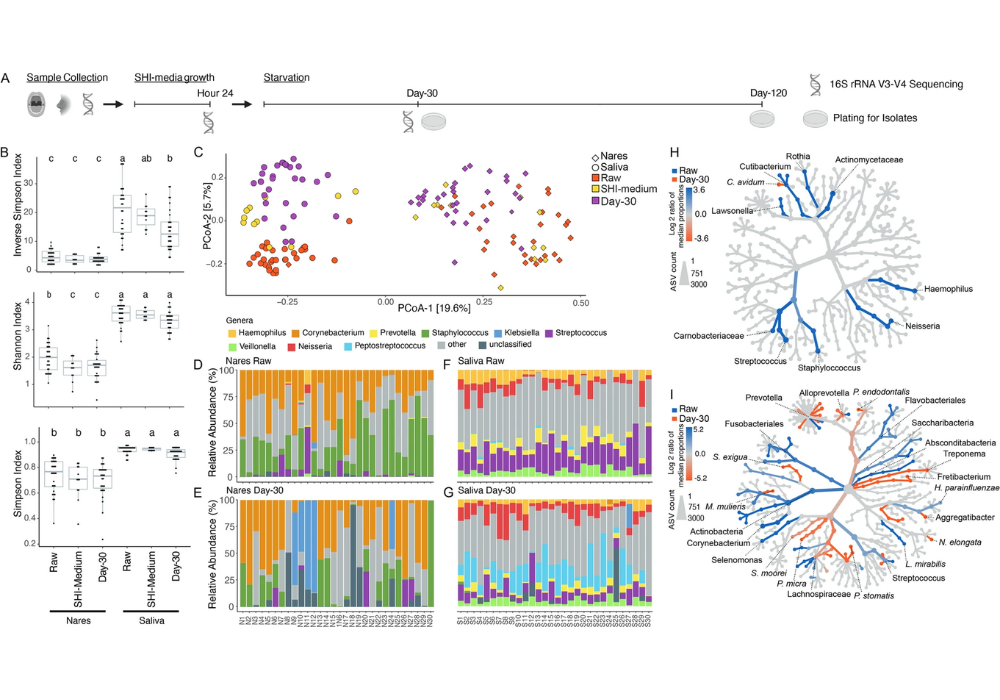
In a study examining the survival of oral microbiome members under starvation conditions, Klebsiella species emerged as the dominant taxa, outlasting other bacterial members. This finding underscores their capacity to survive in nutrient-depleted environments, which is a common condition on hospital surfaces where nutrients are scarce. Klebsiella's ability to outgrow other microbes in such conditions suggests a competitive advantage, possibly due to their metabolic versatility and efficient nutrient utilisation mechanisms.
Furthermore, Klebsiella species have been shown to utilise nutrients released from dead bacteria, allowing them to sustain growth even in the absence of external nutrient sources. This ability to scavenge nutrients from their environment not only supports their survival but also enables them to colonise new niches and potentially disseminate within the hospital environment. The resilience and adaptability of Klebsiella species highlight the need for stringent infection control measures, particularly in healthcare settings, to prevent the spread of these potentially dangerous pathogens.
Managing the Risks of Oral Colonising Opportunistic Pathogens
The study of colonising opportunistic pathogens in the oral microbiome reveals a complex interplay between harmless colonisation and pathogenic infection. Klebsiella species, with their multidrug resistance and resilience, exemplify the potential risks associated with oral COPs. As the healthcare community becomes more aware of the role of the oral cavity in harbouring these pathogens, there is a growing need for comprehensive strategies to monitor and control their spread. This includes not only infection control measures in hospital settings but also a better understanding of the microbial dynamics within the oral cavity and other body sites.
Future research should focus on elucidating the specific conditions and mechanisms that enable COPs like Klebsiella to transition from harmless colonisers to pathogenic invaders. This could involve studying the genetic and environmental factors that trigger virulence, as well as exploring potential interventions to disrupt these processes. Additionally, public health strategies should emphasise the importance of oral hygiene and regular dental check-ups as preventive measures to reduce the risk of infections originating from the oral microbiome.
In conclusion, while the oral cavity is often overlooked as a reservoir for pathogenic bacteria, it plays a crucial role in the overall microbial ecology of the human body. The insights gained from studying oral COPs like Klebsiella can inform broader strategies for preventing and managing infections, ultimately contributing to better health outcomes.