HealthManagement, Volume 22 - Issue 1, 2022
Early during the COVID-19 pandemic, a newly developed Surge Operations Call Center (SOCC) averted overload in individual Central Ohio hospitals by directing patients to hospitals with available beds and staff.
Key Points
- The SOCC, designed to load balance patients during emergencies to network hospitals according to bed and staff capacity, helped prevent hospital overload during the COVID-19 pandemic.
- Streamlined processes, ‘backstage’ execution, and consistent messaging for all referring providers are designed into the SOCC to prevent confusion and frustration in referring providers/facilities and unnecessary rework.
- The SOCC increased relationship building and staff collaboration between separate hospital systems.
- During emergencies, the SOCC brought about better coordination of patient traffic between hospitals to help address patient volume surges.
On 26 March 2020, the three adult healthcare systems in Central Ohio received a call to action requesting that they develop a process to manage the surge of patient volumes related to the COVID-19 pandemic. A conference call with the Central Ohio Trauma System (COTS) Team and hospital leadership occurred that afternoon. The teams collaborated and coordinated with all key stakeholders to develop the Surge Operations Call Center (SOCC), which was activated on 8 April 2020. The initial goal was to monitor the COVID-19 patient population in the Central Ohio area and the overall census capacity in each hospital. A large surge of COVID-19 patients was anticipated. SOCC’s goal was to direct patients to hospitals with available beds and staff to avoid overloading individual hospitals. If one hospital reached capacity, the SOCC would evaluate census across the region and direct patients to the closest most appropriate hospital with capacity. We arranged for 24/7 physician coverage to assist the SOCC registered nurses (RNs) with decision-making support as needed. Physicians from each health system collaborated and developed a rotating call schedule for the SOCC. Fortunately, we never reached a point where our health systems could not accommodate a patient’s hospital of choice.
In addition to the activation of the SOCC, we also had a daily multidisciplinary video conference call with participants from across the region to discuss capacity and COVID-related issues. These participants included transfer centre leadership, health system executives, and COTS leadership. As we progressed further into the pandemic, participation expanded to include Columbus and Franklin County Public Health, leadership from the Ohio Department of Rehabilitation and Corrections (ODRC), and leadership from 46 hospitals across our entire zone.
Who We Are
Central Ohio Trauma System
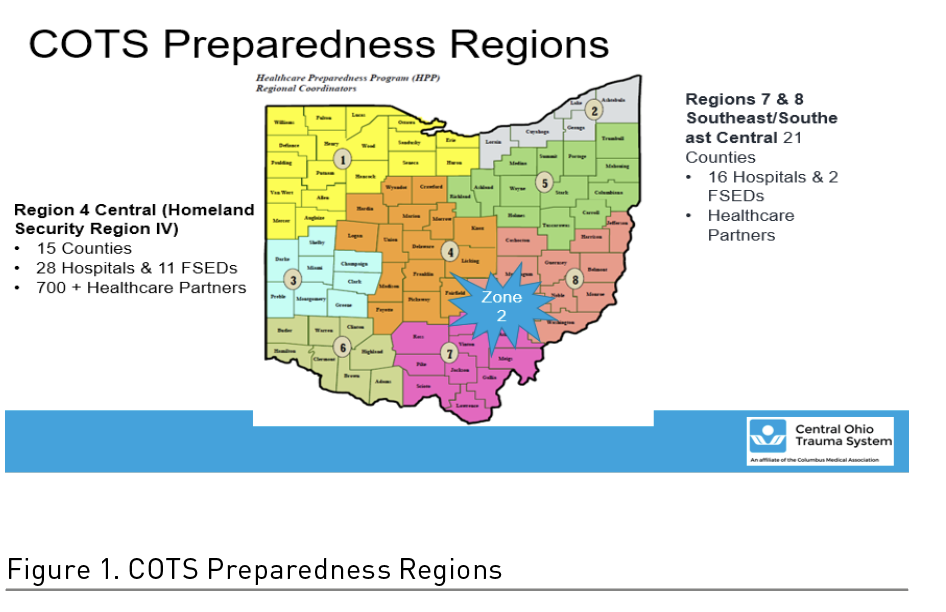
The Central Ohio Trauma System, located in Columbus, Ohio, is a 501(c)(3) private non-profit organisation that coordinates trauma care, emergency care, and disaster preparedness systems throughout 36 counties in central, southeast, and southeast central Ohio. COTS began its collaborative work in 1997 to improve outcomes for injured patients through the coordination of a citywide trauma data registry and trauma education. Today, COTS serves as the hospital preparedness coordination agency for the Ohio Homeland Security Regions 4, 7, and 8. The Central Ohio Trauma System established the Healthcare Incident Liaison (HIL) role to support Central and Southeast, Southeast Central Ohio hospitals and partnering agencies in the event of a disaster, regardless of its scale. The HIL serves as a conduit for situational awareness and information sharing, assists with regional resource allocation, and facilitates response activity coordination for 43 trauma and acute care hospitals.
The facilitation and coordination role of the COTS HIL designates COTS as the coordinating agency for the three regions, which have now become known as Zone 2. The HIL was essential in coordinating the planning of the Alternate Care Site located at the Greater Columbus Convention Center (GCCC). This site was designed to admit COVID-positive (+) patients in anticipation of a surge that would exceed hospital capacity. Each of the three Central Ohio hospital systems were prepared to set up operations at the GCCC. Fortunately, we did not have to operationalise this during the height of the pandemic.
Mount Carmel Health System
The Mount Carmel Health System is a part of Trinity Health, one of the nation’s largest multi-institutional Catholic health care delivery systems, serving diverse communities that include more than 30 million people across 22 states. The Mount Carmel Health System was founded in 1886 by the Sisters of the Holy Cross. Today, the health system is comprised of four hospitals and three free-standing emergency centres serving more than one million patients in Central Ohio each year.
Ohio State Wexner Medical Center
The Ohio State University Wexner Medical Center is a multidisciplinary academic medical centre located in Columbus, Ohio, on the main campus of The Ohio State University. The origin of The Ohio State University Medical Center dates back to 1834 with the founding of the Willoughby Medical University of Lake Erie in Willoughby, Ohio. The Willoughby school moved to Columbus in 1846 to expand and improve its clinical facilities by becoming Starling Medical College, the first teaching hospital in the United States. Over the next six decades, the Starling Medical College merged several times. In 1914, all of its assets were donated to The Ohio State University. It has been named in honour of Ohio State alumnus and The Limited founder Les Wexner since 2012.
As one of America’s top-ranked academic health centres, our team of more than 23,000 is driven by our mission to improve patients’ lives in Ohio and worldwide through innovation in research, education, and patient care. The Ohio State University Wexner Medical Center is comprised of seven hospitals with 1604 patient beds, nine multispecialty centres, 100+ facilities, and a National Cancer Institute (NCI) designated comprehensive cancer centre.
OhioHealth
OhioHealth is a nationally recognised, not-for-profit, faith-based, charitable healthcare outreach of the United Methodist Church. Based in Columbus, Ohio, OhioHealth has been serving its communities since 1891. OhioHealth is a family of 35,000 compassionate associates, physicians, residents, fellows, and volunteers that support a system comprised of 12 hospitals and more than 200 ambulatory sites, hospice, home health, medical equipment, and other health services spanning a 47-county area.
Annually, OhioHealth provides care and services to our patients, their families, and the communities we serve through multiple access points, including over 2.6 million outpatient visits, 541,349 emergency department (ED) visits, 162,754 inpatient and observation hospital admissions, 106,942 surgeries, 14,050 births, and 500 research studies.
Surge Operations Call Center Drill
During the COVID pandemic, it quickly became apparent that the Surge Operations Call Center (SOCC) could be utilised to support additional emergency and patient capacity situations post-COVID. The following debrief describes the first real-world utilisation of the SOCC post-COVID. The Franklin County National Disaster Management System (NDMS) hospitals partnered with the Central Ohio Trauma System and Wright Patterson Air Force Base (WPAFB) to test their role in an NDMS response during the Operation Ultimate Caduceus Exercise from 26 April through 30 April 2021.
The drill’s purpose was for NDMS to partner with healthcare facilities to ensure a network exists to provide care for American citizens and/or military casualties within an area impacted by a natural, man-made disaster, military health emergency, or other public health emergency when additional or complex care is unavailable. The Department of Health and Human Services (HHS), through NDMS, is the lead federal agency for definitive care through a coordinated partnership with the Departments of Homeland Security (DHS), Veterans Affairs (VA), and Defense. In the event of a public health emergency, NDMS, through 65 VA and Department of Defense (DOD) Federal Coordinating Centers (FCCs), manages the medical evacuation from areas impacted by a disaster to designated reception facilities within the NDMS health care facility network.
A nationwide network of over 1,900 civilian hospital partners provides definitive care for NDMS federal patients. The NDMS Definitive Care Reimbursement Program reimburses institutions and practitioners who participate and provide care to NDMS federal patients. Ohio healthcare coalitions support the NDMS mission with 109 certified NDMS hospitals. The COTS regions contain seven certified NDMS hospitals, all located in Franklin County: Mount Carmel East, Mount Carmel St. Ann’s, Nationwide Children’s Hospital, OhioHealth Doctors Hospital, OhioHealth Grant Medical Center, OhioHealth Riverside Methodist Hospital, and The Ohio State University (OSU) Wexner Medical Center.
Ohio NDMS hospitals participate in bimonthly bed availability reporting drills and real-world events using the state-wide SurgeNet system. For the first time, they had the opportunity through SOCC to upgrade to a multi-state military patient movement exercise. The scenario depicted a military conflict. Once patients arrived at WPAFB, they were then transported (simulated) to the Ohio NDMS hospitals. WPAFB, COTS, and the hospitals’ Surge Operations Call Center worked together to load balance incoming victims from the NDMS response. This process allowed patients to be placed efficiently in the most appropriate hospital.
A Hot Wash and After-Action Report was written following the NDMS exercise that detailed successes and a few opportunities for improvement. The SOCC was mobilised and response-ready within just a few minutes after activation. Utilising a WebEx format, hospital transfer centres could communicate and load balance patients between the health systems. The WPAFB patient report spreadsheet provided essential information that allowed the SOCC to place the patient in the appropriate facility and bed type. In all, 76 patients were placed in Columbus hospitals experiencing a high patient census. Sharing patient information between the air force base and the hospitals was initially loosely conducted; however, the process was streamlined and became more proficient by the end of the exercise. Additional exercises will be created and facilitated by the NDMS program at WPAFB.
The Operation Ultimate Caduceus Exercise was a success and truly tested the SOCC operations in a large MCI event involving NDMS. It evaluated the intricacies that will allow for precise improvement to the newly developed SOCC plans and procedures. It also enhanced networking between agencies to prepare for the next exercise and/or response. In addition, WPAFB and the hospitals were also able to test the OHTrac patient tracking system, a state-wide system used for family reunification. Refer to NDMS and Ohio Healthcare Coalitions for more information (U.S. Department of Health and Human Services 2019; Ohio Department of Health 2019).
This exercise’s timing was a perfect endeavour following the recent COVID-19 response, which provided a unique opportunity to test the new SOCC. Creation of the SOCC in early April for Zone 2 included COTS regions 4, 7, and 8 of the Office of the Assistant Secretary for Preparedness and Response (ASPR) grant recipients (Figure 1).
System Planning
The adult hospital systems (Mount Carmel, OSU, and OhioHealth) in Columbus worked together to develop a 1,100-bed field hospital or Alternate Care Site (ACS) located at the Greater Columbus Convention Center for hospital transfer of low acuity stable adult COVID-19 patients. This ACS has since been demobilised and can be re-activated if needed. A huge part of that collaboration led to the establishment of a Command-and-Control Center or a Joint Transfer Center to coordinate the movement of patients across Zone 2, later named the SOCC.
While the ACS did not meet the predetermined triggers for activation during the peak of the COVID-19 response, the SOCC was mobilised to manage transfer calls and can be re-activated within minutes, as necessary, for real-world events and/or drills. Additional planning has since been facilitated by COTS, with the Franklin County adult hospitals and Nationwide Children’s Hospital, to further develop the SOCC as a best practice to incorporate into pre-planned events such as the Arnold Sports Festival, Red White & Boom (RWB), and no-notice mass casualty incidents (MCI). The importance of the SOCC’s participation in no-notice events is to load balance patients being transported from the scene to a hospital or transferred in from a rural county hospital.
To quickly develop a seamless SOCC deployment process across the three main Central Ohio adult healthcare systems while simultaneously communicating to all key stakeholders and educating associates and providers, the team utilised lean methodology tools and concepts (i.e., process flow maps, stand work, rapid-cycle tests of change, and scripting) for managing the design and workflows.
In partnership with COTS, the SOCC project team consisted of transfer centre, information technology (IT), information systems (IS), information security, systems analyst, enterprise project management office (EPMO), marketing/communications, telecommunications, user experience (UX), and physician team members from Mount Carmel Health Systems, The Ohio State Wexner Medical Center, and OhioHealth. The team worked together to develop a unique, collaborative multi-health system COVID-19 triage transfer line within two weeks, which did not disrupt normal referral/transfer processes on the front end for referring providers. All the new processes and workflows for the SOCC were intentionally designed for ‘backstage’ execution to avoid confusion and frustration in referring providers/facilities and unnecessary rework of the individual healthcare system’s normal transfer workflows.
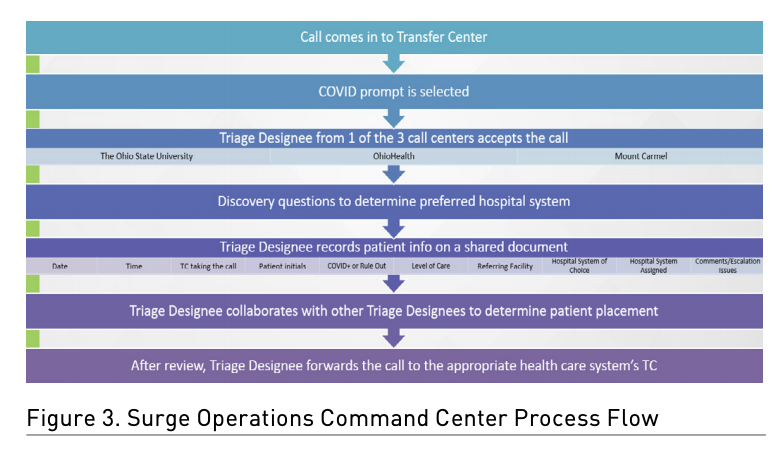
In collaboration with the transfer centres, the IT and telecommunications teams changed the automated messaging for all inbound calls into each of the three transfer centres in Central Ohio to state ‘if you are calling to transfer a suspected or confirmed COVID-19 patient, please press 1.’ The call was then routed behind the scenes, via a call tree process, to a team of RNs comprised of one RN from each of the three main adult healthcare systems in Central Ohio covering the SOCC 24/7. The three RNs interacted with audio and video connectivity via a live WebEx. This provided the opportunity for real-time collaboration to review capacity and ensure COVID-19 patient transfers were balanced across Central Ohio. Figures 2 and 3 represent two examples of process flow maps for the SOCC workflows.
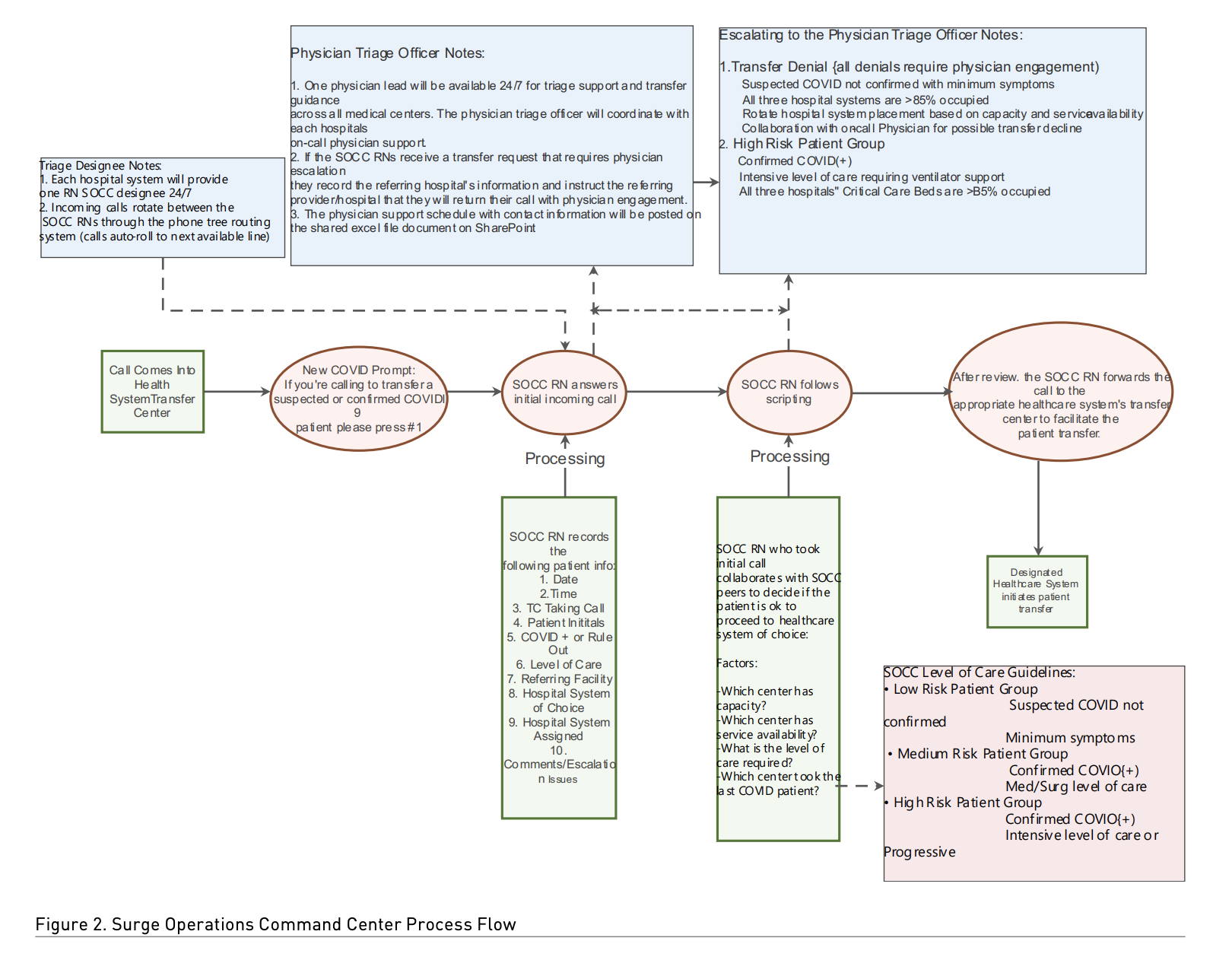
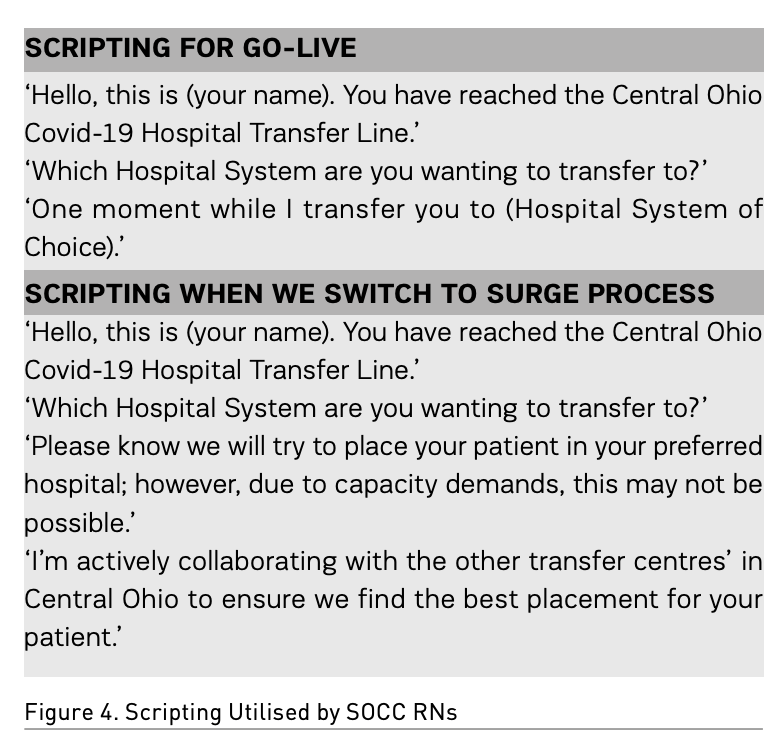
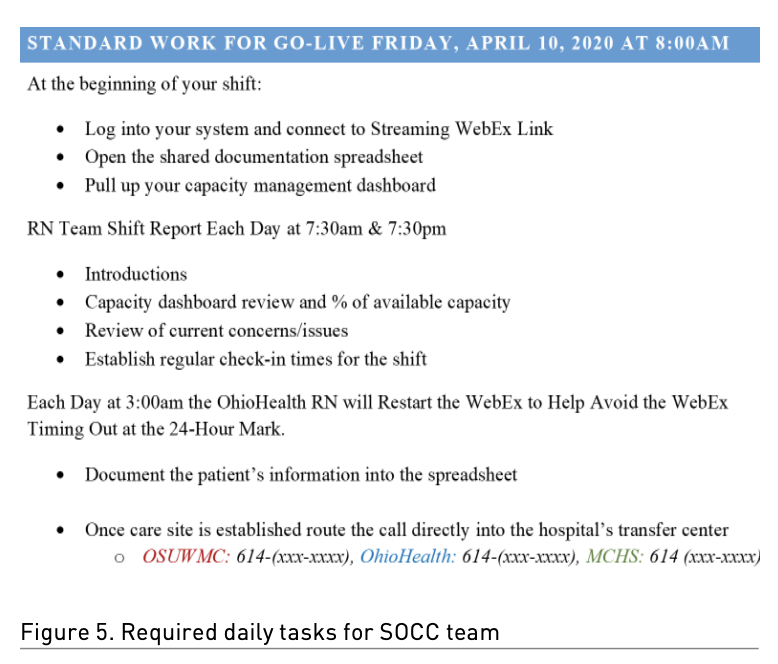
To further streamline processes and keep messaging consistent for all referring providers and care sites, scripting was developed for the SOCC RNs. Two different scripts were created based on capacity levels. Figure 4 is an example of the scripting utilised by the SOCC RNs. Along with scripting, standard work was created to help identify required daily tasks for the SOCC team (Figure 5) and expectations for shift reports between the RNs from the three healthcare systems.
Go-Live
The teams were ready for Go-Live on 20 April 2020, and the inbound messaging was turned on in all three systems at 7 a.m. that day. A shared spreadsheet was developed that allowed each triage nurse to document the call, referral hospital, level of care, and the system to which the patient was assigned. This shared document supported the triage nurses in decision-making regarding patient assignment when patients needed to transfer to a care site outside of their healthcare system of choice.
Placement decisions were based on capacity and equitable distribution of COVID+ patients. It was deemed appropriate to transfer patients to any of the three health systems regardless of the original request, with two exceptions: transplant patients were sent to The Ohio State Wexner Medical Center only, and active cancer patients and pregnant patients were sent to the facility of the patient’s choice. There was an on-call Triage Physician available for any issues, concerns, or questions at all times. Each system took turns assigning the on-call Triage Physician. Our experience was such that this physician’s expertise was needed very infrequently to assist with assignments.
The collaboration between these three hospital systems was impressive; the triage nurses quickly came to know each other and their working environments. It was soon decided that the three triage nurses could communicate through written statements in the chatbox, and it was unnecessary to keep the audible communication open 24/7. At the beginning of each shift, reports were managed by verbal communication, including reviewing each system’s capacity.
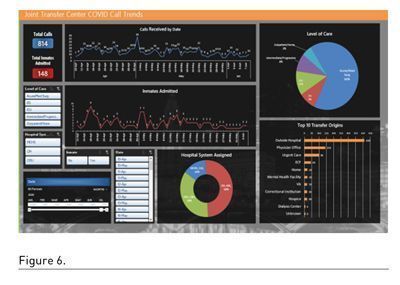
Given that data are drivers of all innovation, we committed to keeping the Central Ohio COVID-19 Hospital Transfer Line data as pure as possible through our shared documents. Figure 6 shows the dashboard developed and shared weekly with the system administrators.
Unanticipated Benefits
On 1 May 2020, The Ohio State Wexner Medical Center experienced a phone and integrated healthcare information system (IHIS) outage, preventing the transfer centre from receiving external calls. The internal phone system remained intact during this outage. Since all calls were being routed and answered by any of the three system hospitals, Mount Carmel and OhioHealth could receive calls meant for Ohio State. The calls were then ‘transferred’ back into Ohio State without difficulty. This day was the highest call volume for the SOCC since the original go-live day. Thus, the SOCC provided a great unintended benefit for Ohio State and allowed the continued flow of all patients into the healthcare system.
At the beginning of this endeavour, all state inmates were being admitted to The Ohio State Wexner Medical Center related to contractual agreements. The system quickly became saturated with the inmate population, while the total capacity of COVID+ patients increased alarmingly. The ODRC began collaborating and planning visits to the OhioHealth and Mount Carmel Health systems to identify designated units for state inmates. In mid-May 2020, there was a large surge of inmates admitted to Ohio State, which rapidly expanded the areas within their hospital to accommodate this patient population. Given concerns that the number of inmates would exceed this extended capacity, ODRC visited Mount Carmel Health and an OhioHealth hospital to identify inpatient units that could accommodate inmates. A plan was developed for correctional officers to be deployed to these sites; the hospitals were prepared to admit inmates. Fortunately, the inmate surge subsided before Ohio State exceeded capacity; however, the other health systems were prepared to help at any time if needed.
Our Public Health Systems began to collaborate with the Extended Care Facilities (ECFs) in the surrounding areas to ensure adequate testing, isolation practices, and safe processes for transfer into one of our three systems for care of the COVID+ patients. Public Health also began working closely with our three systems during this time to ensure the appropriate transfer of recovered COVID+ patients back to the ECFs upon discharge from the hospital. Columbus Public Health and Franklin County Public Health joined our daily surge calls and became a part of our collaborative team. Each healthcare system was assigned a group of ECFs to partner with, and the health departments partnered to provide guidance. We arranged for a personal protective equipment cache that could be supplied to ECFs as needed, and there were discussions around strategies to cohort discharged COVID patients within the ECFs to ensure the safety of all residents and staff. This support allowed the ECFs to bring their residents back to their facilities which positively impacted capacity within the hospitals.
Current State
The SOCC was deactivated on 10 June 2020, as the increasing numbers of COVID+ patients stabilised, and the systems believed they could resume COVID+ normal practices. It was tested at this time to see if the Transfer Line could be re-activated within a two-hour time frame in case an emergency-type situation required it. The test was successful.
Future State
Out of this collaboration, the SOCC was developed as an integral part of the emergency system for the surrounding Columbus area. SOCC’s vision is to activate the call centre within 60 minutes of an emergency involving the community and/or surrounding areas. As we looked to enhance SOCC’ effectiveness, Nationwide Children’s Hospital has become a functioning member of the call centre.
As previously discussed, the SOCC was successfully utilised in the Operation Ultimate Caduceus Exercise. We continue strengthening our relationships through monthly meetings, planning future drills, and our continued conversations as a collaborative group.
Lessons Learned
This experience’s most valuable lesson was that three major competing healthcare systems could collaborate to protect their community in a designated region. Before creating the SOCC Mount Carmel, OhioHealth, and The Ohio State Wexner Medical Center had never collaborated on a joint venture of this magnitude.
Thankfully, we never reached a surge level which necessitated diverting patients from their hospital of choice. On 20 June 2020, the decision was made to discontinue the 24/7 SOCC process. Before placing this process on hold, we consulted with our IT and telecommunications team to develop a plan to quickly re-activate the SOCC if needed. We determined that, if necessary, the entire process could be re-activated within one hour. In mid-October 2020, we entered another COVID patient surge which vastly exceeded patient numbers in the spring. The SOCC was re-activated until the volume of COVID admissions began to decrease. Although the SOCC is now deactivated, we continue to have a monthly call to check-in, share information, or discuss issues within the zone.
One of this process’s many benefits, which cannot go unmentioned, was the relationship building and collaboration between the three health systems and COTS. The healthcare systems, who always viewed one another as competitors, now consider ourselves partners who work together to serve our communities and patients. Senior leadership, physicians, IT, telecommunications, and the transfer centre leadership teams continue to collaborate and reach out to discuss the long-term pandemic-related issues (i.e., visitor restrictions, vaccination strategies, capacity). We also collaborate on topics unrelated to COVID-19 and are always ready and willing to discuss issues as they arise.
The value provided by the SOCC and collaboration among our health systems has many potential advantages for use beyond the pandemic. We have partnered with COTS to develop a plan to use the SOCC during planned emergency drills and true no-notice emergency situations. We will use the planned drills to re-activate the process and keep our team members competent. This process was an undertaking that required a vast number of people and resources to make the concept a successful process in a short timeframe. It is exciting that this effort, which started as a short-term process related to one issue, will continue to serve our patients, communities, and healthcare systems for years to come.
Conflict of Interest
None.

References:
Ohio Department of Health (2019) Hospital Preparedness Program. Available from odh.ohio.gov/wps/portal/gov/odh/home/
U.S. Department of Health and Human Services (2019) NDMS Patient Movement Program. Available from www.phe.gov/Preparedness/responders/ndms/Pages/patient-mvmt.aspx







