Mapping the landscape of ageing for more effective healthcare
How can the spatial sciences contribute to streamlined healthcare by addressing multi-morbidity in ageing populations across the globe?
The global population is ageing. This is not only a general demographic pattern but one with a variety of unique trajectories by country and region, and system-specific implications. A successful transition to the status of an aged society has implications for conventional medical approaches and health systems operations, which themselves have often emerged over decades in response to past problems and prevailing assumptions. These include the notion that people become ill from and tend to die due to one specific condition—as illustrated by health and insurance statistical systems globally (Kingston et al. 2018).
Under conditions of population ageing, the norm will increasingly be one of multi-morbidity and a consequent rise in individual and systemic complexity. This is, simply put, where older people tend to increasingly accumulate health conditions which contribute to their overall morbidity status and, ultimately, their deaths (Cheung et al. 2018). And while we may still identify a single cause of death on the death certificate, this does not adequately reflect the larger reality of health and illness in an ageing world. This rising complexity has implications for every step in the chain from birth to death and from prevention to treatment and, ultimately, end-of-life care.
On track to an aged world
Even in sub-Saharan Africa, where fertility rates remain high overall, the total numbers of older people are growing rapidly. In higher income countries, this process is already well advanced and having quite specific consequences (OECD 2017). Population ageing is already having an impact on middle-income countries where infectious and chronic diseases complicate the conventional pathway to a health transition (Gaimard 2014). In short, we can see an overarching pattern underpinned by a variety of local demographic and epidemiological trajectories. The inevitable endpoint of this larger trend will be the rise of the aged society—one in which older people outnumber the young and where ageing becomes the new demographic norm.
Multi-morbidity and mortality
Multi-morbidity refers to the presence of two or more health conditions experienced by a single individual. Interestingly, the variety of groups potentially affected by such a state is both complex and varied. Older people are commonly seen in this category of patient, and are often on equally complex medication regimes, which may in fact exacerbate their multi-morbid status while treating one (or more) of their diagnosed conditions (Gómez et al. 2015). But many other groups, such as people with a disability, with a chronic pain-related syndrome or those with a long-term workplace injury, may also exhibit features of multi-morbidity (Goodman et al. 2016). Indeed, ageing and disability commonly intersect under the rubric of multi-morbidity and the vast majority of people with a disability are older people (Quiñones et al. 2016).
Not uncommonly, such multi-morbidity may arise as a confluence of a dominant physical complaint in combination with subordinate symptoms and resulting psychological impacts. In effect, we suggest, multi-morbidity has actually been much more common (and for longer) than is generally supposed, and growing awareness is as much responsible for its rising prevalence as changes in demography and associated epidemiology. This can be seen in the tendency to dismiss the psychological impacts of diagnosable conditions as psychosomatic or, not uncommonly experienced by women, as ‘imaginary’. And given that the majority of older people, particular the very old, are female this is another dimension of current healthcare approaches that will require significant improvement.
The effort to operationalise concepts such as ‘frailty’ illustrates both the necessity and complexity of the position of multi-morbidity in contemporary healthcare environments. We need to see multi-morbidity as not simply a clinical status conferred by medicine but also a socio-political construction of the multi-morbid patient, the extent of their ‘needs’ and the framing of their entitlements to health and social care services. Such debates are already in play and, we suggest, this will only become more problematic as population ageing grows and disability categories and rates increase (and diversify).
Multi-morbidity as confounder for conventional systems of care
The World Health Organization (2016) has already identified a need for a rise (or re-emergence) in generalism in medical care for people with multi-morbidity. The contemporary dance between general and specialist care experienced by so many older people, often in a crude hub and spoke model (out and back, out and back) and others with complex conditions, is neither desirable nor sustainable into the future. Continuing increases in healthcare costs cannot simply focus on demographic change as a driver, however convenient for politicians, economists and insurers, but must also consider the current limitations to the design of healthcare systems and the shape of medical and allied healthcare practice.
The economist JK Galbraith coined the term ‘the conventional wisdom’ to refer to ideas which have become accepted, even unquestioned, in society at large. Many of our healthcare systems exhibit similar levels of comfort with the general status quo of why we provide the healthcare we do and in the way(s) we do. However, we suggest that population-level ageing represents a major disruptor to any conventional wisdom of healthcare. Ageing is already disrupting our assumptions about how we understand the health and wellbeing of older people and the current and impending effects of their growing numbers on current service design and delivery arrangements.
Complexity is on the rise and this must not only be acknowledged more directly but addressed more categorically in healthcare environments. Researchers such as Brian Castellani and colleagues (2015) have been promoting the need for a turn away from reductive strategies in healthcare in order to, finally, address the innate complexity of individuals and their circumstances. This means addressing factors such as multi-morbidity or frailty as they occur in each individual patient and not as a general or overarching diagnostic category.
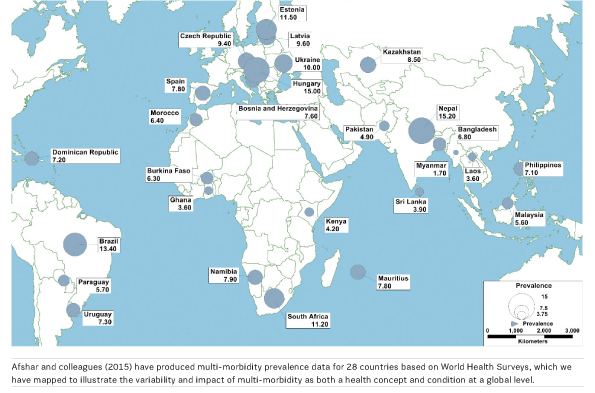
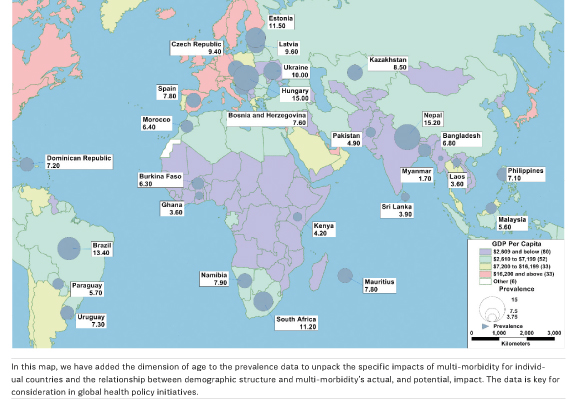
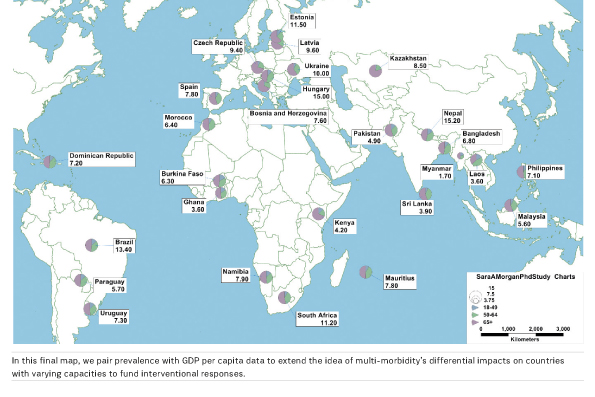
A geography of multi-morbidity
One of the viable and practical strategies for addressing multi-morbidity lies in a greater application of spatial science applications. Demography, epidemiological patterns and health services provision are, at least in many countries with good quality data, highly mappable. And all of these factors display distinctly spatial patterns. In this context, the location of individuals and clusters of people with complex shared symptomologies makes them amenable to spatial analysis. They can in effect be mapped and networked to available bricks-and-mortar healthcare resources or, if those are lacking, to substitute resources in the mobile or telehealth domains.
Building capacity for an ageing world
The growing impact of multi-morbidities and their association with population-level ageing presents a number of challenges, both philosophical and practical. One of the practical ones is connecting older people, themselves often frailer and less mobile than other community dwelling groups, to the complex web of services that currently exist. The spatial patterning of older people and the health and social care systems, themselves often poorly or inadequately connected, rarely matches up. More than this though is the prevalence in many countries of a health system designed and built around the needs of the past having to reconsider design and delivery to a less mobile, often place-bound, ageing population.
Sometimes the reaction to this is an ageist one. Older people are assumed to be in some way responsible for their inability to meet the system as it currently exists, rather than acknowledging this as an indicator of current design limitations. Indeed, any policy or service provision framework that assumes people exist simply to adapt to it will clearly find population ageing a confounder for established models, and patterns, of care. In other words, population ageing is a driver for change and one which requires a marked degree of capacity-building if older peoples’ needs are to be effectively met. Models drawn from the 19th and 20th centuries, with their emphasis on infectious diseases and acute health events, will become increasingly inadequate to meet emerging needs.
Mapping the ageing/aged world
One of the as yet underutilised strategies for coping more effectively with population ageing and the needs it is giving rise to, lies in the contemporary spatial sciences. The policy literature is replete with concepts around the term ‘ageing in place’. But this often simply refers to a person’s home or some contracted version of the older person’s perceived daily activity space (often conceived quite narrowly as home, shops and health services). Even now, the emerging digital paradigm is poorly integrated, since ageist attitudes conceive of older people as technology shy, at best. This too is going to need to change.
So here we suggest that the spatial sciences offer a potential suite of connecting technologies to support population ageing. These various combinations of hardware and software including geographic information systems (GIS), global positioning systems (GPS), remote sensing (RS); unmanned aerial vehicles (UAV) technology, radio frequency identification (RFID) and so on. While often serving quite distinct purposes, their emerging utility, as expressed in the Internet of Things concept, is one of connection through the digital to the analogue lives they can be used to support.
Typically, this means a greater interoperability between structures such as electronic health records (EHRs), alerts systems, and specific health and social care providers (including acute, sub-acute, primary care, rehabilitation and community social supports). The old policy silo structures will not be sufficient for connecting our increasingly ageing world. Using spatial technology that supports older people where they already are and in where they need or want to get to, will be an emerging development in this field.
Multi-morbidity, so intimately connected to ageing, can only encourage this increasing embeddedness of spatial technology, methods and concepts. This is especially so as the world’s population becomes increasingly urban and intimate local and contextualised knowledge of who is where diminishes. Perhaps the potential exists for this particular kind of technology to help us re-localise for high density urban environments?
Of course, this is not a call for simply more technological determinism. Instead we are proposing a response to population ageing that uses place-related, and relevant, technologies in association with geographic conceptualisations of ageing and their intimate connection to space and place. Older people, unless dislocated, are highly place dependent/interdependent. They experience local attachments and preferences, which in turn inform both memory and affect. Many aged care facilities seek to mimic the ‘home’ in their advertising in recognition of this deep and fundamentally human sense of connectedness to place. The opportunity exists to combine high technology and informative social science understandings to assist us in adapting to the emergence of the ageing and, ultimately, aged world.
Conclusion
Globally, population ageing is a driver for significant social, economic and systemic change. It is adding to the complexity of contemporary societies, in part because we have not designed our systems to accommodate complexity more effectively. The concept of multi-morbidity, and emerging concepts such as frailty, show how we are attempting to capture and respond to age-related complexities. The intersection of these ideas with problems connected to age-related neurodegeneration, such as the dementias, shows just how complex this situation is likely to become as population progresses. And how challenging it will be without a platform for supporting adaptation and capacity building the aged care ‘space’.
The conventional wisdom will serve us poorly unless it too becomes increasingly characterised by a complexity focus. Ageing is the emerging focus of many of these complexities. They will also intersect with other forms of complexity and associated adaptation, such as climate change. Our position here is that the spatial sciences, moderated through a geographic social sciences lens, have a great deal to offer in responding to those complexities. And in doing so we may yet produce a new conventional wisdom, one relevant to and informative of the aged society.
Key Points
- There are implications for healthcare in a successful transition to the status of an aged society
- The groups impacted by multi-morbidity, the presence of two or more health conditions in an individual, are complex and varied
- The spatial sciences can offer practical strategies in healthcare as multi-morbidity demographical and epidemiological patterns are highly mappable
- Population ageing is an engine for social, economic and systemic change
- Spatial sciences can offer a suite of connecting technologies to support ageing