HealthManagement, Volume 17 - Issue 2, 2017
Mobile devices are used by most students, residents and radiologists in everyday life. They allow fast and convenient access to all internet resources and to data stored on the devices. Entire bookshelves of information can be transported easily and are at the device user’s fingertips. The interactivity of mobile devices allows new techniques of knowledge presentation to be introduced. During the past years, an increasing number of learning and reference apps that draw on this capability have been introduced. Different classes of e-learning apps can be identified. Their quality in terms of content, usability, and clarity is very disparate, as is assurance of their continued availability. There is a need for radiology e-learning apps to undergo quality control and review. In addition to mobile devices, social media will also play an increasing role in radiology e-learning.
Although mobile devices (personal digital assistants like the PalmPilot® and Windows PocketPC®) were introduced in the late 1990s and early 2000s, it was the introduction of the iPhone ten years ago that started the success story of mobile devices. Today, mobile devices are ubiquitous, and in the pocket of almost every student, resident or radiologist. Most smart functionality of mobile devices is provided by mobile applications that can be purchased on the device from so called App stores.
Advantages of Mobile Devices
Mobile devices have a number of advantages. They provide portability, flexibility, access to multimedia, and the ability to look up information quickly (Wallace et al. 2012). Mobile devices have enough memory to store huge amounts of data, enabling the user to store the equivalent of an entire library of radiology books and journal articles. In addition to the weight advantage when compared to printed media, mobile devices now have excellent screens and powerful processors, allowing dynamic and enhanced display of radiologic images or other documents. While paper is able to display only static images, mobile devices allow entire stacks of radiology examinations to be rendered, including 3D rendering of data enhanced with overlays of comments and highlights that can be turned on and off for learning purposes. Compared to conventional desktop computers or laptops, the advantage of mobile devices is their portability. This is of special interest in the learning context, since it is much more convenient to read an ebook or use a teaching app on your mobile phone than a laptop when travelling on a train or plane.
Categories and Examples of Apps
Depending on the way content is generated and used on mobile devices, different categories of mobile apps may be distinguished. Some editors propose using a combination of different categories.
Classic Media Content Transferred to Mobile Devices
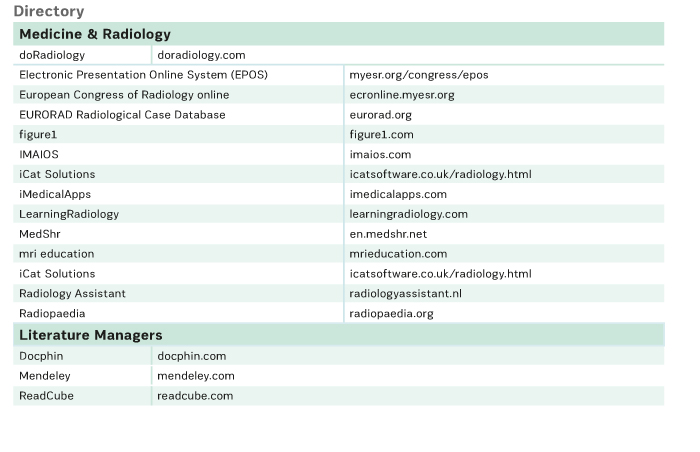
Most print media are available in digital format, usually Adobe PDF®. Different reader applications allow these texts to be read on mobile devices. The digital format allows searching and the ability to use hyperlinks within the same or between different texts. Some applications also allow the reader to make personal annotations in digital documents. However, many readers still feel more comfortable reading books, because they believe it is faster to browse through these than through an ebook. Lectures can be easily recorded on electronic media and distributed through the internet. Channels of distribution include YouTube and Podcasts among other platforms. A great collection of radiology-only lectures has been collected by the European Society of Radiology (ESR ) and can be found on European Congress of Radiology (ECR) Online (ecronline.myesr.org). ESR also offers a large collection of teaching cases with EURORAD (eurorad.org) and radiological posters with EPOS (myesr.org/congress/epos). All of these are readily available on mobile devices that have access to the internet (myesr.org/education/online-services).
Literature Managers
There are several powerful tools that can be accessed on mobile devices, which enable the user to organize collections of articles and book chapters. These apps allow the user to access and download articles from electronic scientific journals, and index articles or other documents from other channels. They also integrate powerful tools, which enable the user to organise a personal library. Keywords can be attributed to articles, citations can be extracted, and notes to articles can be documented. Examples of literature managers are ReadCube (readcube.com), Mendeley (mendeley.com) and Docphin (docphin.com).
Wikis
“A wiki is a website that provides collaborative modification of its content and structure directly from the web browser” (en.wikipedia.org/wiki/Wiki). Wikis are powerful and flexible knowledge management systems. The best-known public radiology wiki is Radiopaedia (radiopaedia.org), which provides more than 10,000 articles and 25,000 cases at the time of writing. In contrast to Wikipedia, where quality is supposed to be controlled by “crowd intelligence”, the accuracy of articles in Radiopaedia is assured by a board of editors. While access to the web version is free (financed by advertising), the content for the mobile app has to be paid for.
See Also: Creating Healthcare Apps that Meet Needs and Usability Expectations
Dedicated Radiology Learning Apps
Specialised radiology learning apps constitute a new category of media. In the best cases, they have excellent content written by an expert author, are overseen by a n e ditor, a nd m ake good use of the m ultimedia capabilities of mobile devices, thus offering an enhanced learning experience. Dynamic display of images, multidimensional display, interactivity and audio are examples of new possibilities that facilitate understanding and retention of sometimes complex content. Excellent examples are the series of apps published by doRadiology® (doradiology.com). Technically less innovative, but with proven content, mri education has released a series of apps combining lectures to watch combined with notes on the basic physical principles of MRI (mrieducation.com). Radiology Assistant (radiologyassistant.nl) is a source of radiological knowledge both as a website and an app, with continuously extended peer-reviewed content for several subspecialties. Another app with a broad range of radiological content (in German), including books, journals, and other educational and reference material in one app, is the eRef App (eref.thieme.de) from Thieme Editors.
Anatomy Apps
This is a special class of apps, which together with their desktop counterpart, have rapidly replaced classic anatomy books. The major advantage for the radiologist is the ability to interactively scroll through the body in different planes, and the possibility to display schematic and MR or CT anatomy side by side. For the student or resident, the biggest advantage is the possibility to turn anatomy marks on and off. Whilst a wide variety of anatomy apps exist, it is certainly worth having a look at the innovative e-anatomy app from Imaios (imaios.com).
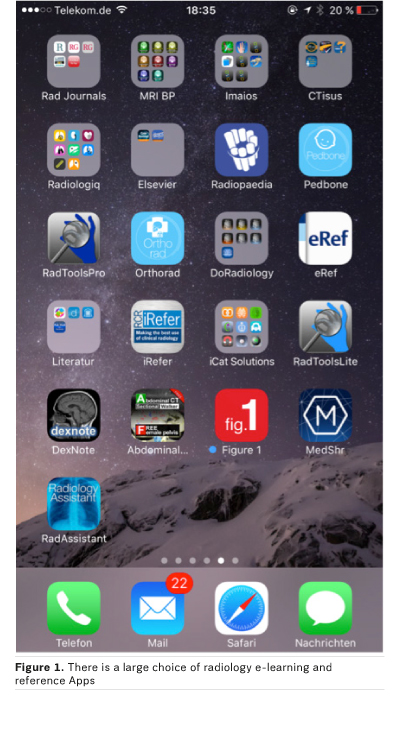
Simulation Apps
Simulation apps engage the user either to actively set up parameters in the app interface, to control a virtual device or to respond to a virtual diagnostic situation (patient simulation). Good examples are apps that simulate the control of different MRI sequences and present the corresponding images as a result of the interaction, such as MRI Sim from iCat Solutions (icatsoftware.co.uk/radiology.html).
Limitations of Apps and Mobile Devices
Quality and Persistence Issues with Apps
While apps on mobile devices offer many new possibilities, the radiology app market is far from mature. When searching the app stores, the sheer number of radiology apps (Rodrigues et al. 2013) makes choosing one difficult (Aungst et al. 2014). Many radiology apps have been written by one person. In these cases, an update of the app or of its content is often not guaranteed. Some older apps no longer even run on newer mobile operating systems, and this is not always evident when downloading the app. For most apps, it is also unknown whether content undergoes peer review and editorial control. For these reasons, a self-certification system for medical apps has been proposed by Lewis (2013). There are a few websites trying to help with reviews of medical apps, such as iMedicalApps.com. Only a few reviews of radiology apps are available in the literature. Shelmerdine and Lynch reviewed smartphone applications in paediatric radiology (Shelmerdine and Lynch 2015) and the Journal of Digital Imaging started in 2015 to conduct reviews of radiological apps (Shih 2015). Usability of radiology apps needs to be improved in many cases (Kim et al. 2016).
Mobile Devices are Not Integrated into Radiologists’ Workflow
Radiologists in their daily routine are less mobile than other medical doctors. Since they are sitting most of the time in front of a diagnostic workstation, the use of a mobile device could be less attractive than for other specialists, especially when considering clinical decision systems, which we expect in the future to be seamlessly integrated into radiologists’ workflow.
Where Are My Personal Notes?
A major inconvenience of apps, as with web content, is their very limited capability to hold personal notes made by the user. This is a real drawback when compared with classic books or journals. For many people, enriching text or other content with personal comments or highlights is an important support for memorisation, and helps them to quickly recall facts when coming back to the same text. While one can still keep a personally annotated older copy of a book, this is impossible with apps or websites. The notes are simply lost when you get an upgrade of the app or when the website is rewritten.
Future Trends
Microlearning, Integration of Clinical Decision Systems and
E-Learning
The rapid increase and turnover of medical and radiological knowledge makes it difficult to learn all radiology knowledge through books and other printed media as in the past. It is almost impossible to keep up to date with new classifications or clinical pathways. The role of clinical decision systems will increase in the future, not only for ordering radiology examinations, but also for coming to conclusions or making recommendations based on radiology examinations. If well conceived, these clinical decision systems could lead to something Charles Kahn called “just-in-time learning” (Kahn 2006), ie microlearning during the radiology reading process. New or updated information would be presented on demand by the system during the reading of radiology examinations. It is reasonable to expect mobile devices in the future to be linked to desktop applications, thus bridging the gap between mobile e-learning and clinical decision systems.
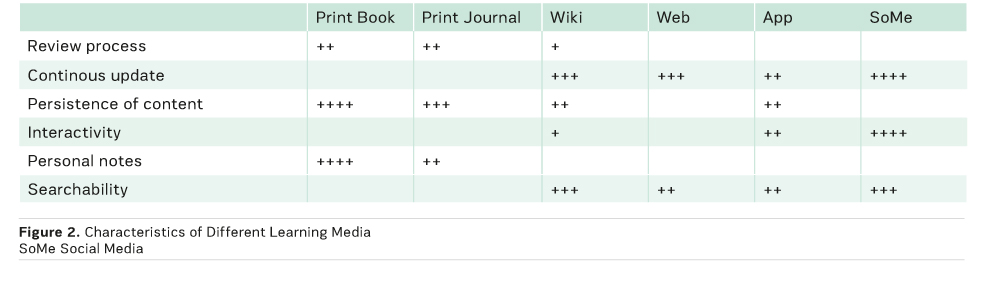
Social Media and E-Learning
“Social media use web-based technologies, desktop computers and mobile technologies (eg, smartphones and tablet computers) to create highly interactive platforms through which individuals, communities and organisations can share, co-create, discuss, and modify user-generated content or pre-made content posted online” (en.wikipedia.org/wiki/Social_media). Social media are ubiquitous in the daily life of the general population and radiologists (Ranschaert et al. 2016). While general social media, such as Twitter, Facebook or Instagram, can be used to enhance e-learning (ie, to tweet about new content from sites such as LearningRadiology (learningradiology.com)), social media specialised in medical e-learning are appearing on the market. New relevant content is actively being pushed to the user. Information is presented in small pieces— something that appears to be an important feature for digital natives, who can have shorter attention spans than previous generations. Small pieces of information are also very convenient for presentation on mobile devices and on the go. The pioneer in this field is figure1 (figure1.com). Another example is Medshr (en.medshr.net), which is intended for discussion of medical cases in a professional social network. Social media are expected to play an increasing role in e-learning. For example, FOAMrad is a community of radiologists that shares and discusses free open access radiology education material (twitter.com/foamrad).
Conclusion
While print media today still have some advantages, it is
foreseeable that for future generations of students, residents and
radiologists—the digital natives—print media will be replaced with digital
content (Duszak 2011), and digital content will, for a large part, reside on
personal mobile devices. Some of today’s inconveniences of digital content
(including lack of editorial control, quality issues and usability) will be
resolved by organisational changes, such as the expansion of small companies,
or large commercial editors stepping into the mobile market. Interactivity and
social media will play an increasing role in learning radiology, since these
are tools that upcoming generations have grown up with and use in their
everyday life.
References:
Aungst TD, Clauson KA, Misra S et al. (2014) How to identify, assess and utilise mobile medical applications in clinical practice. Int J Clin Prct, 68(2): 155-162.
Duszak RD, Haines GR, Van Duyn Wear V et al. (2011) White paper from the ACR Task Force on Print Media in Radiology. J Am Coll Radiol, 8(10): 692-702.
Kahn CE, Ehlers KC, Wood BP. (2006) Radiologists' preferences for just-in-time learning. J Digit Imaging, 19(3): 202-6.
Kim MS, Aro MR, Lage KJ et al. (2016) Exploring the usability of mobile apps supporting radiologists' training in diagnostic decision making. J Am Coll Radiol, 13(3): 335-43.
Lewis TL (2013). A systematic self-certification model for medical applications. J Med Internet Res,15(4): e89.
Ranschaert E, Van Ooijen PM, McGinty GB et al. (2016) Radiologists' usage of social media: results of the RANSOM survey. J Digit Imaging, 29(4): 443-9.
Rodrigues MA, Visvanathan A, Murchison JT et al. (2013) Radiology smartphone applications; current provisions and cautions. Insights Imaging, Band 4(5): 555-62.
Shelmerdine SC, Lynch JO (2015) Smartphone applications in paediatric radiology: availability and authority. Pediatr Radiol, 45(9): 1293-302.
Shih G (2015) App review series introduction. J Digit Imaging, 28(1): 7-9.
Wallace S, Clark M, White J (2012) 'It's on my iPhone': attitudes to the use of mobile devices in medical education, a mixed methods study. BMJ Open, Band 2(4). doi: 10.1136/bmjopen-2012-001099.



