HealthManagement, Volume 16 - Issue 3, 2016
HOW TO DEFINE, MEASURE, AND INCREASE POSITIVE AND REIMBURSABLE PATIENT CARE OUTCOMES
Due to increasing cost pressure, established remuneration models for healthcare services are changing all around the world. As part of the move toward value-based care, patient outcomes are entering the spotlight. Thus, hospital managers face the challenge of improving overall patient outcomes in a cost-effective manner.

Diagnosis: Making Well-Informed Decisions
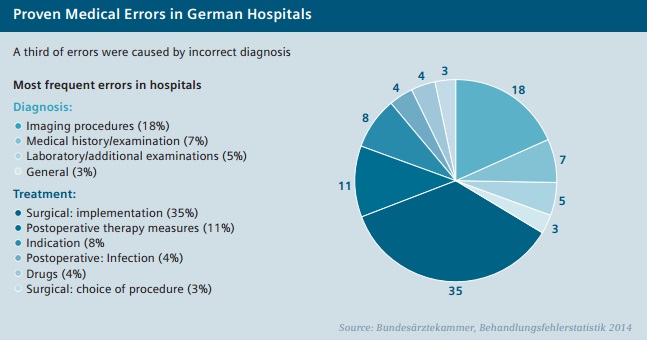
Every successful treatment and pathway to positive patient care outcomes begins with a correct and timely diagnosis. When a patient goes to see a doctor, the first few minutes usually determine the subsequent treatment steps – which directly influence the success of the treatment and the associated costs. However, diagnosis itself can be a particularly complex challenge. Research suggests that, in the U.S. for example, diagnostic errors affect one in 20 patients annually, an estimated 12 million Americans each year.1 Moreover, diagnostic error is the leading cause of medical malpractice claims in the U.S. (almost 30 percent), and is estimated to cause 40,000 to 80,000 deaths annually.1
As demanding as it can be to identify and avoid diagnostic errors, it is well worth the effort, as doing so significantly improves patient outcomes. Misdiagnosis can lead to unnecessary treatment for non-existing conditions, or to proper treatments being initiated too late or not at all. This not only impacts the patient but providers as well. Providers are increasingly facing the operational and economic consequences of incorrect medical care – for instance, when hospital stays are unnecessarily long, medications are used incorrectly, or avoidable exams and operations are performed. The results are often a worsening of the patient’s condition, readmissions, reduced efficiency, and, worst of all, expensive legal battles.
Efficient and Effective Treatment
Usually, the diagnostic procedure is followed by a treatment decision. In the interests of beneficial patient outcomes, diagnosis and treatment should be seen as two separate decision-making processes that need to be optimized, because the initial diagnosis could be incorrect or incomplete. In addition, even if the diagnosis is correct, there are often several possible therapeutic approaches. For good treatment decisions, it is important to know all the options. These arise from one’s knowledge of the individual medical condition, the patients themselves, and scientific findings. Electronic health records (EHR) and a seamless flow of information between physicians and specialists, and science and technology, can play a crucial role here.
The variety o f treatment options and t he uncertainty involved in planning them are the areas in which patient outcomes and sensible resource allocation are at risk. Treatment should be efficient as well as effective, and should lead to the desired outcomes. Clinical monitoring will become more important for optimizing patient outcomes and maximizing cost efficiencies. Up-to-date diagnostic imaging and laboratory equipment can support the ongoing, near-time monitoring of treatment success. However, many hospitals delay modernization of expensive devices due to increasing cost pressure. This can create significant differences in the kind of hospital equipment available in richer countries compared to poorer countries. For example, data on European equipment stocks show that patients in Eastern Europe in particular have very limited access to MRI s and CTs.2
Improving Outcomes through Quantification
The quality of diagnosis, treatment decisions, and monitoring/management of the treatment significantly affect patient outcomes. According to U.S. economist Michael Porter, provider organizations - facing lower payment rates and potential loss of market share - have no choice but to improve value and be able to prove it. Although hospital managers have now recognized the need for doing this, in practice they often still lack suitable measurement methods. Most quality metrics do not gauge quality; rather, they are process measures that record compliance with practice guidelines. According to Porter, the only true measures of quality are the outcomes that matter to patients.3
To obtain meaningful benchmarks, care providers should actively engage patients in the collection of outcomes data. Patient-Reported Outcome Measures (PRO MS) are already being successfully used by various hospitals in the U.K. to improve patient outcomes. For example, PRO MS are used to calculate health gains in the aftermath of several kinds of surgical treatment, using preoperative and postoperative patient surveys. Some British studies show how hospitals have successfully used PRO MS data as a benchmark for their own quality measures. These best-case studies show that standardization can greatly help improve patient outcomes. At the same time, the case studies suggest that improved patient outcomes do not necessarily have to be accompanied by higher costs, and can actually improve profitability.4
Creating a Continuum of Care
Especially in western industrialized nations, the present-day healthcare system is a highly sophisticated but fragmented collection of service providers. Previously, the process of tracking the journey of individual patients often ended at the point of transfer to another provider/specialist, or at discharge. Follow-up on the success of treatment rarely took place. In light of rising costs, however, providers in many countries are increasingly seeking to make optimum use of available healthcare resources. To ensure more cost-effective healthcare, providers are examining the entire care continuum to identify areas for improvement. By looking at the overall patient journey, providers can potentially improve patient outcomes while reducing costs. Also, provider cooperations and alliances that encompass hospitals, physician groups, outpatient clinics, and other provider facilities are on the rise.
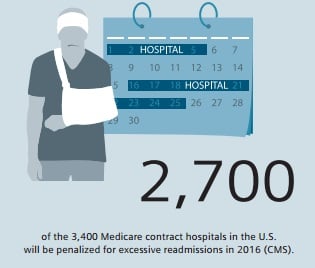
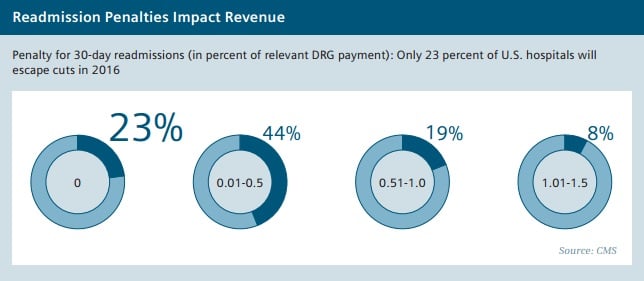
The Affordable Care Act, which was passed in the U.S. in 2010 under President Barack Obama, provides clear examples of how service providers are encouraged through financial incentives to continue making a positive contribution to patient outcomes beyond the day of discharge. For instance, Medicare reduces provider compensation if patients are readmitted within 30 days of discharge. This affects every fifth Medicare patient - a staggering number of those treated. According to the Center for Medicare and Medicaid Services (CMS), approximately 2,700 of the 3,400 Medicare contract hospitals will have cuts totaling $420 million in fiscal year 2016 due to such readmissions.5
Because of increasing cost pressure, hospital managers face the challenge of improving patient outcomes in a cost effective manner.
Engaged Patients Improve Outcomes
For healthcare providers, it is worthwhile to examine how care is provided along the treatment chain and to optimize it as needed. In particular, the general practitioners who care for patients following their discharge, and also the patients themselves, have a considerable influence on patient outcomes. Survey and research results from the U.S. show that hand-off communication and the discharge process are sorely in need of improvement at many companies. In the latest annual U.S. national patient survey, 14 percent of respondents said they had neither received any written information about what symptoms or health warning signs they should look for in the future, nor had had conversations about the need for a follow-up appointment and, with whom, after their discharge.6
However, the patient’s proven influence on his or her own outcomes may be challenging in cases where service providers find it difficult to increase patient engagement. Socioeconomic factors such as low income, unemployment, and poor education can lead people to neglect their health and fail to follow their doctors’ recommendations or keep appointments. Several studies from the U.S. actually show a link between high readmission rates and a hospital’s catchment area. It indicates that hospitals in poor regions are disproportionately affected by readmission penalties.7 This once again shows how important it is to develop reliable and reasonable outcomes measurements.
Smarter Data for Better Care
Well-managed IT infrastructure and mobile technology can help optimize the patient pathway and investments in mobile technology encourage patient engagement, for example by helping patients and doctors stay connected via mobile resources like tablets and smartphone apps. Thus, visitbased care is giving way to connected care. In developed economies, some of the greatest benefits of connected care would be improvements in the treatment of chronic diseases.
Furthermore, the greatest benefits of Internet-of-Things applications could lie in expanding delivery of healthcare services to the under-served, according to a recent McKinsey study.8
The Electronic Health Records that have been introduced in many countries also provide a platform for shared decision making between patients and doctors. According to a recent survey by the consulting firm Accenture, more than half of all patients want to be able to access their data online.9 This would definitely be to the benefit of many doctors. A vast majority of U.S. doctors report that patient updating of personal electronic medical records improves patient engagement and satisfaction. 10 Healthcare providers who manage to create stronger ties to their patients and let them independently contribute to their patient journey can achieve better long-term patient outcomes.
References:
1. Society to Improve Diagnosis in Medicine, www.improvediagnosis.org
2. COCIR, Medical Imaging Equipment, Age Profile & Density 2014
3. Harvard Business Review, The strategy that will fix health care, Michael Porter and Thomas H. Lee, 2013
4. Health and Social Care Information Centre HSCIC, PROMs Benefits case study, 2015
5. Modern Healthcare: Medicare readmission penalties create quality metrics stress, http://www.modernhealthcare.com/article/20150808/MAGAZINE/308089963
6. HCAHPS online: http://www.hcahpsonline.org
7. JAMA Internal Medicine, Patient Characteristics and Differences in Hospital Readmission Rates, 2015
8. McKinsey Global Institute, The Internet of Things: Mapping the value beyond the Hype, 2015
9. Accenture Healthcare IT Vision 2015, top 5 eHealth Trends
10. Accenture doctors survey 2015

