The EMR does not have to fail
The much-maligned Electronic Medical Record (EMR) is not necessarily a tool which leads to physician burnout. The KLAS Arch Collaborative shows that proper training, personalisation and teamwork can optimise the use of this digital tool without stress and frustration. (For the purposes of this report, the terms EMR and EPR are synonymous.)
EMRs are being attacked by sensationalist articles in the media regarding their impact for driving increased physician burnout related to poor design that frustrates their efforts to deliver efficient patient care. While these articles may drive higher numbers of readership, they are rarely if ever substantiated by statistically significant data for EMR usability and satisfaction. The KLAS Arch Collaborative has surveyed over 110 organisations globally that have generated over 50,000 clinician responses on the usability and satisfaction with their EMRs in supporting healthcare delivery. Key human factor approaches that drive higher levels of EMR usability and satisfaction are associated with EMR training and follow-up education, an emphasis on helping clinicians use EMR personalisation tools to improve care delivery workflow efficiency and establishing a culture of teamwork between the IT staff and the clinicians for effectively supporting and enhancing EMR capabilities. Employing these human factors approaches for implementing and supporting the EMR can have significant positive satisfaction impacts for all clinicians with their EMR solutions.
Arch Collaborative data overview
The KLAS Arch Collaborative data is collected from organisations using a standard 25 question survey to measure EMR usability and satisfaction from doctors, advanced practice providers, nurses, and allied health personnel. A net promoter scoring system is used to generate a Net EMR Experience Score (NEES) to rate EMR functions, personalisation tool adoption, training approaches, and stakeholder performance (eg leadership/IT, the clinicians, and the EMR vendor(s)). A total NEES is created for the organisation as a whole and compared to three cohorts, the global collaborative, organisations with the same EMR, and with similar organisation types (eg academic medical centres, children’s hospitals, large organisations, community health systems, etc). Additionally, Arch Collaborative data is used to conduct statistical analysis to establish key findings.
Initial EMR Training – a key factor
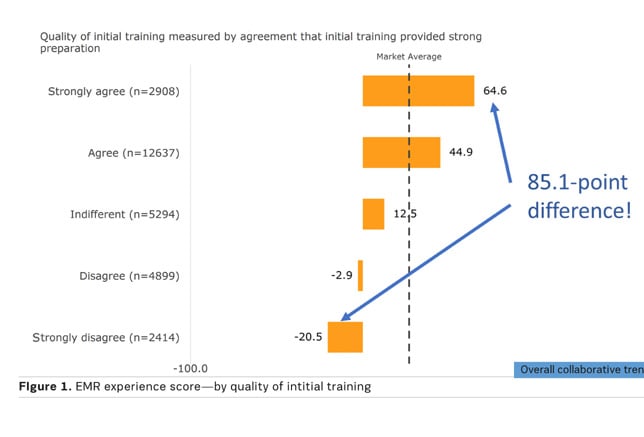
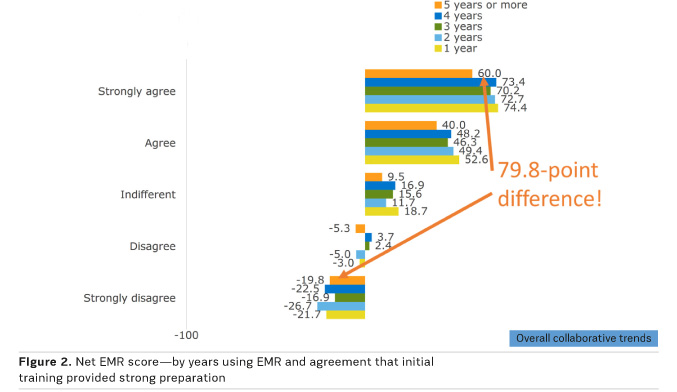
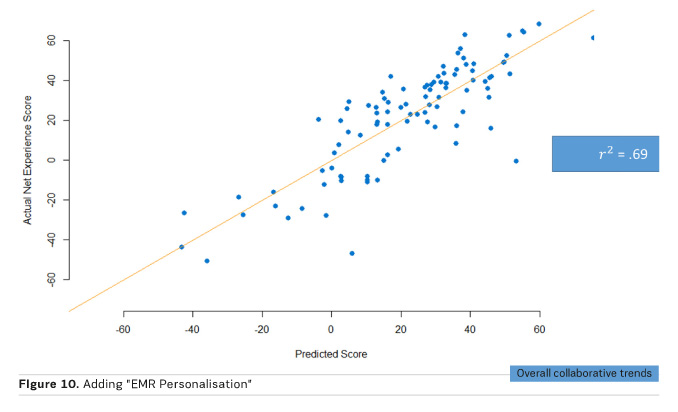
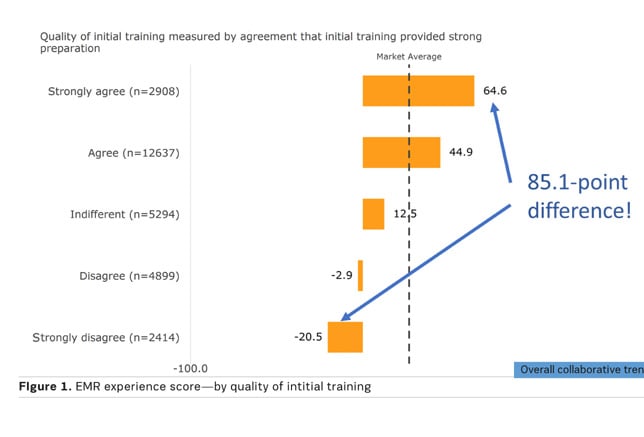
Initial EMR training and education is an overlooked factor for improving EMR satisfaction and usability. To many organisations, it is a necessary evil required to drive the clinicians to use the EMR as soon as possible. A notable discovery of the Arch Collaborative is that initial training and education not only provides a key indicator for EMR satisfaction, it can establish EMR satisfaction for several years afterward. As shown in Figures 1 and 2, clinicians who strongly agree they received high quality initial EMR training versus those who strongly disagree with this finding, have a NEES that only drops 5.3 points over five years. This is a clear indication that high quality initial EMR training is a key factor in establishing and maintaining higher levels of EMR satisfaction with clinicians.
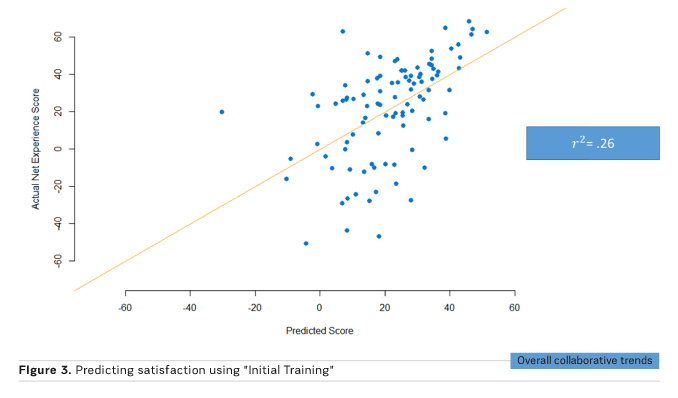
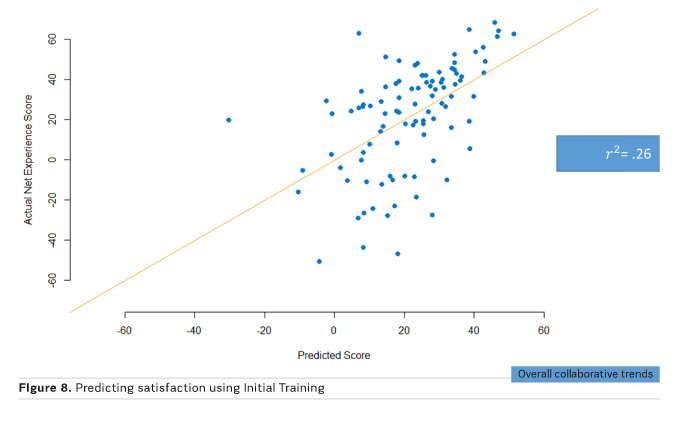
Using the NEES for initial training as a predictor of EMR satisfaction generates a correlation coefficient of 0.26. See Figure 3. This statistic further supports the impact of initial training for establishing a solid foundation for EMR satisfaction.
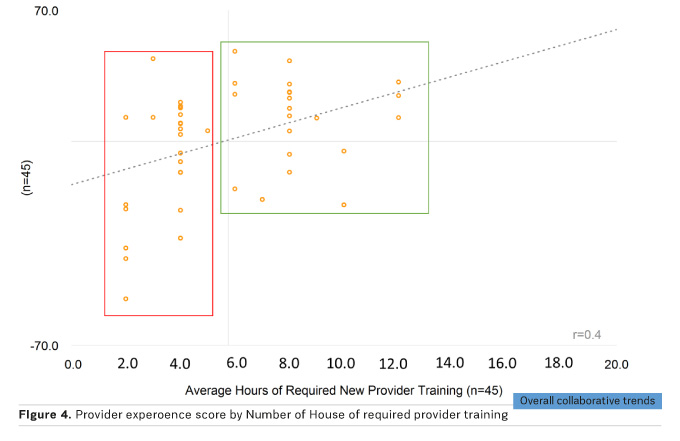
Another key correlation for EMR satisfaction related to initial training is the number of hours provided. Figure 4 demonstrates that provider organisations that deliver six or more hours of initial EMR training and education generate higher NEES with a correlation factor of 0.4. The six hours of initial training do not have to be delivered at the same time. Many organisations provide two hours of initial training followed up with additional sessions of at-the-elbow-training 30, 60, or 90 days post the initial two-hour training session.
The combined findings of the Arch Collaborative on the importance of delivering high quality initial EMR training are undeniable relative to EMR satisfaction impacts. Organisations who fail to heed these findings will suffer with additional costs related to higher levels of ongoing EMR support services, as well as lower satisfaction ratings from their clinician base.
Personalisation tool adoption
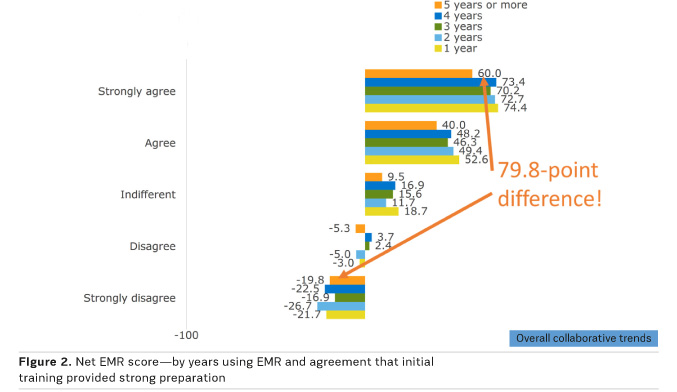
A second key factor in predicting EMR satisfaction is the adoption of personalisation tools by clinicians to increase workflow efficiency for care delivery. As seen in Figure 5 clinicians who have high levels of adoption of personalisation tools have a 14.3 point advantage in NEES over clinicians who have moderate personalisation. This NEES difference is even more pronounced between high and low personalisation clinicians at 30.2 points. The best analogy to EMR personalisation is the personalisation that people adopt for their smart phones. How many smart phone applications are added to a person’s smart phone to make them more efficient and connected? How useful would these smart phones be to these individuals if they were removed? Doesn’t the same logic apply to the EMR?

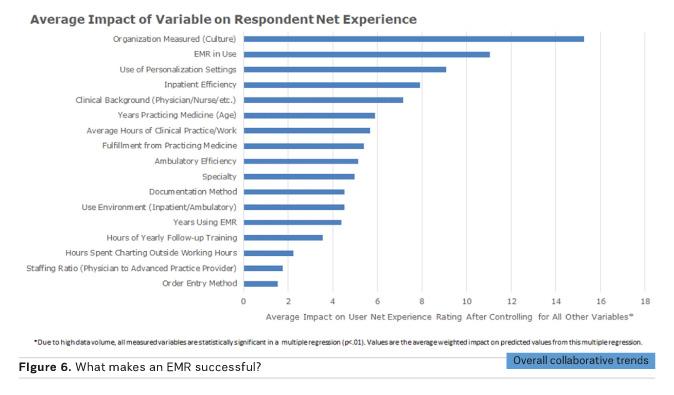
Another finding regarding the personalisation factor for EMRs is that tools that support clinicians with efficiently extracting data from the EMR or assisting in improved EMR functional navigation will have the most impact on provider satisfaction. In Figures 6 and 7, a comparison of NEES scores between various personalisation tools between Epic and Cerner EMR users that have adopted compared to those who have not adopted the tools, demonstrates this finding. For both EMR solutions, personalisation tools that support data extraction/retrieval and navigation have a higher NEES difference between adopters and non-adopters, than for tools that are used for EMR data input. But, what do we focus our EMR training to achieve? Using tools for EMR data input. Follow-up education for the EMR should focus on creating support to help clinicians use tools for EMR data extraction/retrieval and navigation. This education should be focused on tool adoption related to the workflows of the clinician specialists. Cardiologists will have a much different need for personalisation tools to support their workflows than oncologists, and the same applies to nursing and therapy specialties. With the amount of money we have invested in acquiring EMRs, how can anyone justify short changing the ability to optimise their use?
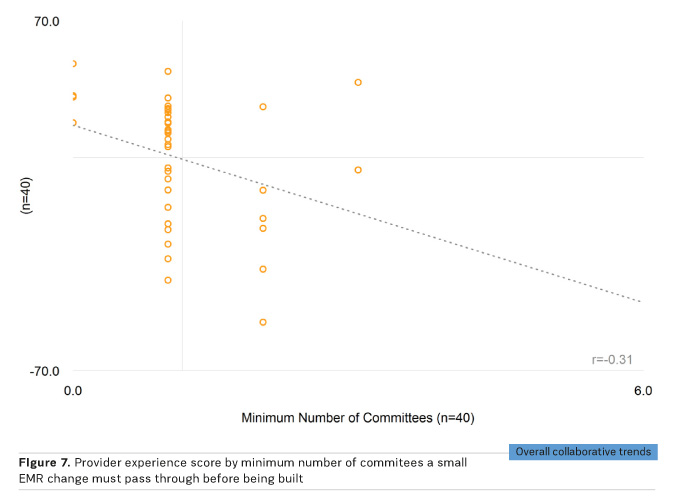
Establishing a culture of EMR teamwork
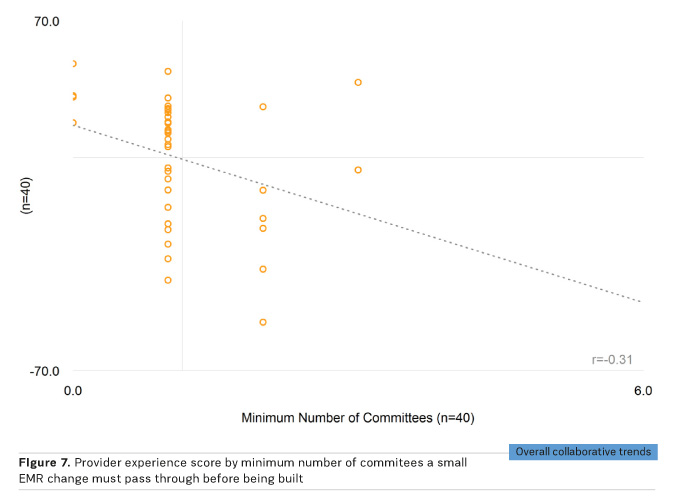
One of the most important factors for improving EMR usability and satisfaction is the ability of organisational leadership/IT to establish a trusted role for supporting and improving the EMR with the clinicians. Figure 8 demonstrates the impact of organisational culture on NEES. The highest performing global organisations to date have established a close relationship with their clinicians for supporting EMR changes that improve the usability of the EMR. To demonstrate this further, Figure 9 depicts higher NEES for fewer committees a small EMR change must pass through with a correlation coefficient of negative 0.31. No clinician likes to make a request for a simple EMR change and not see it implemented, or implemented several months later. A key consideration for establishing a trusted relationship with clinicians regarding EMR governance is to ensure clinicians are engaged in the strategy and enhancements for the EMR. Delivering quickly on relevant clinician EMR requests initiates the trust relationship between IT and clinicians and will also assist in reducing clinician frustrations with the EMR. The result is effective clinical informatics governance.
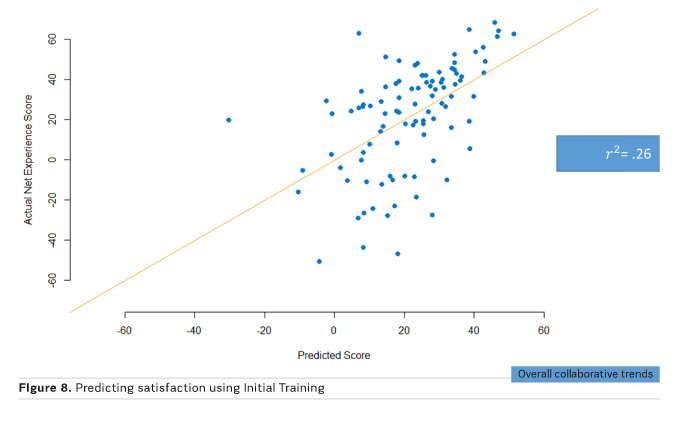
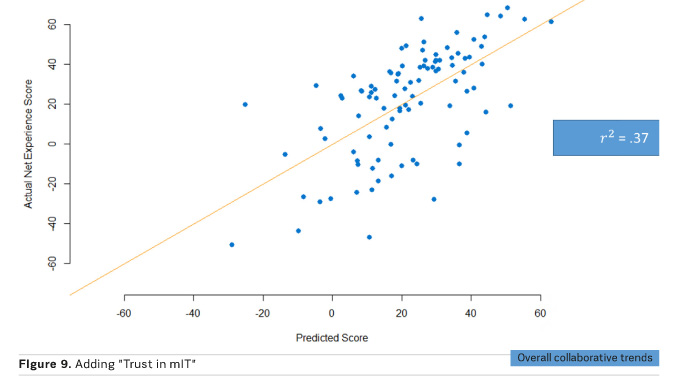
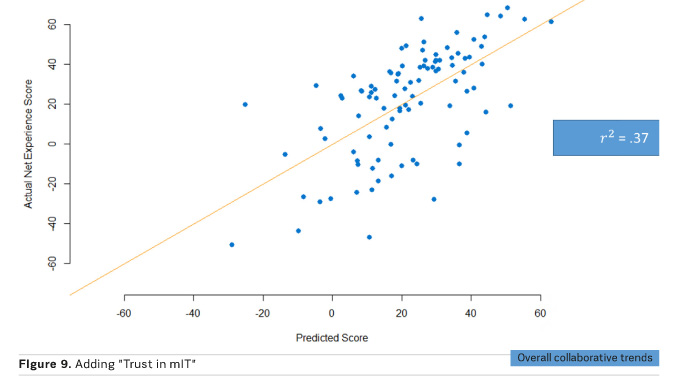
A combination of human factors accurately predicting EMR satisfaction
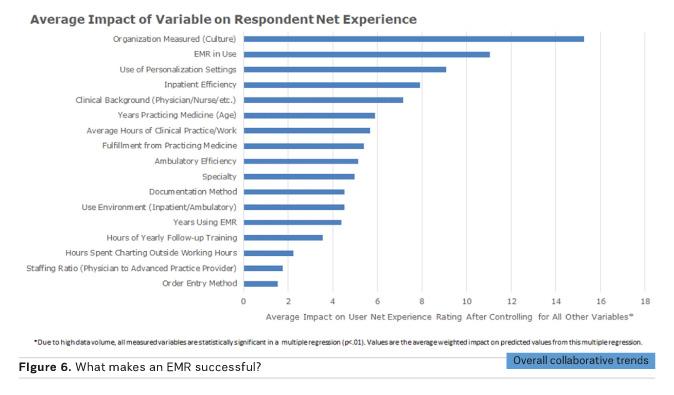
The Arch Collaborative has derived three key human factors that incrementally build on the ability to accurately predict EMR satisfaction. Figure 10 demonstrates that by evaluating the predictive scores of initial EMR training, “Trust in IT”, and the adoption of EMR personalisation, almost 70 percent of EMR environments can be accurately assessed to improve EMR usability and satisfaction. Arch Collaborative survey results help organisations effectively target which of these three (in some cases all three) can be targeted with resources to improve their EMR environments. Ongoing Arch Collaborative research will measure improvements for organisations who have made operational adjustments for EMR training, personalisation adoption, and EMR governance to determine the impact of human factors for delivering an optimised ROI for the EMR. At this time, we also believe improvements in EMR satisfaction will also improve physician wellness/fulfillment measurements, and we will continue to evaluate that aspect of EMR satisfaction.
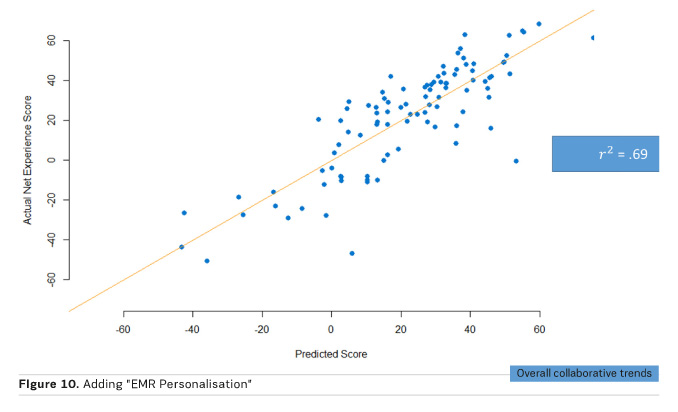
The human touch is the way forward
The three key findings from Arch Collaborative global research that drive higher levels of EMR usability and satisfaction are related to human factors, not new and shiny technologies. Human factors that provide high quality and effective initial EMR training, the adoption of EMR personalisation tools that support clinician workflows for retrieving EMR data and navigating the EMR more efficiently, and the ability to create a trusted teamwork environment between leadership/IT and clinicians will result in an EMR environment that will help support lower healthcare delivery costs and higher quality healthcare.