Shear wave elastography (SWE) has become widely accepted in clinical practice at breast centres around the world. Studies have demonstrated that SWE has reduced the number of unnecessary biopsies, helped prevent false negative diagnoses, and improved overall diagnostic confidence and patient management (Berg et al. 2012; Evans et al. 2012).
With data from over 60 peer-reviewed publications, shear wave technology has proven benefits. In clinical practice, the benefits continue to be seen every day, impacting clinician and patient alike.
Technology
Shear wave elastography is a technological advancement that provides additional, important quantitative information about tissue elasticity to ultrasound imaging. Unlike conventional elastography methods, which rely on manual compression and measure tissue displacement, SWE requires no manual compression. Shear wave propagation speed is calculated and a colour-coded, real-time SWE map is produced showing quantitative (in kilopascals or m/s), local tissue stiffness.
Clinical Benefits Tissue stiffness or hardness of a mass provides important information to the clinician. When the stiffness of the lesion and its surrounding tissue are quantified, a physician can use that information for more accurate diagnosis and planning. The information plays a critical role. as it offers meaningful information about the Breast Imaging-Reporting and Data System (BI-RADS®) classification, location and morphology of a specific lesion.
In our breast centre, SWE is used routinely on every suspected lesion. The technology is of particular benefit for classification of difficult category 3 and 4 lesions on the BI-RADS scale. The technology allows us to confidently downgrade a suspicious lesion from one of highly suspicious and requiring biopsy to one of low suspicion and thus not requiring biopsy, ultimately reducing the number of unnecessary biopsies. The same can be said of the decision to upgrade and biopsy. SWE increases overall diagnostic confidence.
This experience is not unique; a prospective multicentre study of 958 women confirmed that adding SWE improved specificity of ultrasound mass assessment without loss of sensitivity (Berg et al. 2012).
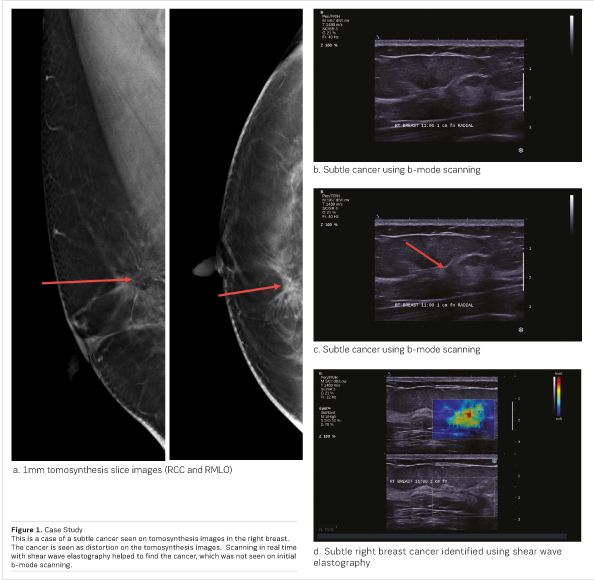
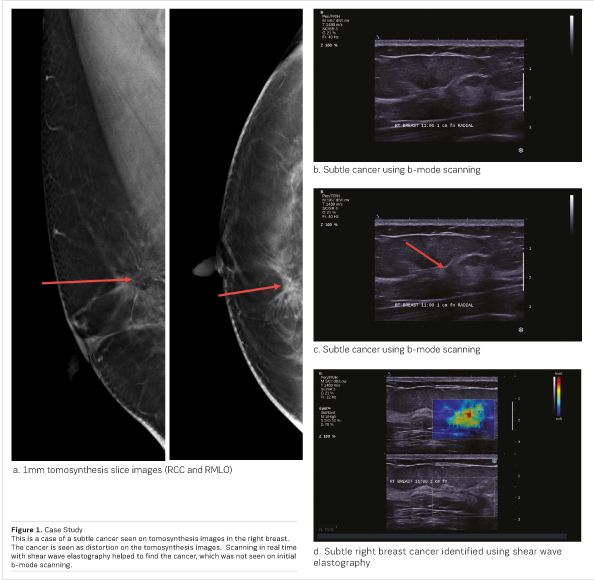
Another important benefit of SWE is its role in biopsy guidance in real time. In a recent case at our centre (see Figure 1), a patient had an area of subtle distortion that was detected using digital breast tomosynthesis. It was confirmed, located and documented on shear wave elastography. When the patient came back for biopsy, b-mode alone failed to visualise and detect the lesion. With the addition of SWE, we were able to clearly identify the lesion, correlating it with tomosynthesis. During this procedure, real-time SWE identified the stiffest portion of the lesion for targeting and guidance. The result was the discovery of a small invasive cancer, which might have been missed using conventional b-mode ultrasound.
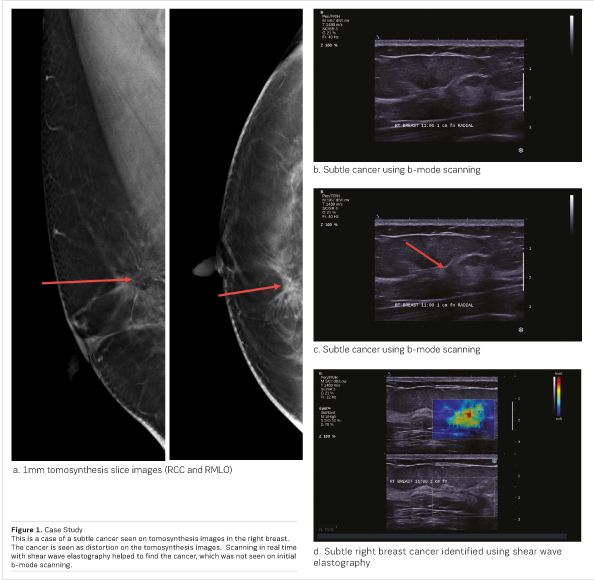
Without SWE, a tomo-guided needle biopsy, a stereotactic biopsy or even surgical biopsy may have been required.
This case further validates research I conducted in which real-time SWE added to second-look ultrasound after MR imaging increased the detection rate of cancers and helped target cancers for ultrasound-guided biopsy (Plecha et al. 2014).
The image quality that SWE produces is a major clinical benefit. Both MRI and tomosynthesis are noted for their image quality, but the addition of SWE provides unparalleled clarity and definition of borders. This allows for the improvement in locating lesions, classifying lesions and targeting lesions during biopsy.
Improved Patient Management and Workflow
The clinical benefits previously discussed have an impact on the overall breast centre function, from both a patient and workflow perspective.
The ability to classify lesions more confidently, avoid false positive as well as false negative diagnoses, and improve locating and targeting during biopsy have a profound impact on the patient and breast centre.
With SWE, we are able to quickly identify those patients requiring or not requiring biopsy. For the patient not requiring a biopsy, anxiety is immediately reduced. In addition, these patients are able to avoid lost time and cost burdens. For the patient who does require a biopsy, the ability to quickly classify the need for biopsy, as well as efficiently and accurately conduct the biopsy, helps alleviate the stress associated with the procedure. As a result, the overall patient experience is improved.
The breast centre as a whole benefits as well. Clinician and technologist time is allocated appropriately, and this helps the centre run more efficiently.
Conclusion
The information that shear wave elastography provides helps to improve diagnostic confidence. Improved diagnostic confidence has a profound impact across the continuum of care, limiting unnecessary care, directing resources to the patients who need it, avoiding unnecessary burdening of the patient, time lost to follow-ups, and needless costs.
SWE continues to be more broadly adopted into the daily workflow, and as confidence grows, the use of SWE will certainly expand.