HealthManagement, Volume 20 - Issue 9, 2020
Vall d’Hebron University Hospital is one the largest hospitals in Spain and one of the most prominent examples of a value-based healthcare institution in Europe. An expert behind the hospital’s VBHC transformation shares the ongoing experience of assessing and redesigning the care cycle based on the VBHC model and outlines the main challenges and achievements on the way.
There is no consensus on what value-based healthcare is. How is it understood at Vall d’Hebron Hospital?
There have been so many concepts linked to the philosophy of value-based healthcare (VBHC). The definition of Value according to Prof. Michael Porter is the Outcomes that matter most to patients divided by the Costs of the care process. Nevertheless, when it comes to implementing it at the operational level, patient needs (thus, value) vary within the same clinical condition. One cannot help wondering how exactly we measure the outcomes that matter most to each patient (once the basic outcomes, such as survival, are assured), how we calculate the cost of the optimised process in a personalised manner.
Vall d’Hebron Hospital (VdH) has developed a methodology that aims to put as the main goal what each patient defines as value. For that, we need to find the root cause of all the clinical activities that don’t add value to the patient, and to erase them from the pathways so that we can reallocate the resources to the activities that do add value to the patient, and, as a consequence, increase Value.
The VdH’s methodology to implement VBHC focusses on four root causes: the optimisation of the process, the consolidation of the safety culture, the enhancement of innovation from the frontline professionals, and the assurance of the clinical practice appropriateness. The continuous improvement of these four concepts will be one of the drivers that work towards the increase and decrease of respectively the numerator and the denominator of Prof. Porter’s formula.
The other driver to systematically increase the value provided to the patient is their engagement/empowerment. When process is being redesigned, we ask patients about their feelings and met/unmet needs through their care process, so that we can together design the tools to enhance engagement and shared decision-making.
Measuring outcomes is crucial as it will be the ‘snitch’ that can tell if patients are getting value in a tangible, routine manner as well as be the driver to culturally root the PDCA (plan-do-check-act) concept at the everyday, operational level.
Costs are the reflection of each patient process and, despite the difficulties we have with measuring these in our organisation, we think the denominator should vary according to the measures embedded in the care process continuous improvement, as this will let us leave aside the costs linked to safety issues, process inefficiencies or inappropriateness of the clinical practice, and only include costs linked to value practices.
What specific challenges has VdH had to overcome during its transition to VBHC?
Where do I begin!.. The real challenge behind these two drivers is the cultural change for all the stakeholders of the care pathway that implies VBHC implementation, which is understood and faced differently by both patients and team members dealing with a clinical condition. Reminding that patient value is common ground through the change process is important.
Some specific challenges we’ve found rooted in the culture at the operational level are breaking the ‘silos’ way of working (meaning that each stakeholder knew their own duties but not the ones of another team member treating the same patient); understanding the real potential of the patient outcomes as a tool to personalise the value given to each patient instead of ‘one more task that I have to do’; ownership of process redesign by the frontline team members (who were used to a hierarchy culture, in which all decisions had to be led by ‘the top of the pyramid’); believing that VBHC had to go hand in hand with assigning more resources instead of methodologically detecting where the non-value in their care pathways was, so that those resources could be reallocated; or extracting and analysing data, since data were stored in ‘silos’. Overcoming these challenges is an everlasting work in progress.
If we zoom out a bit from the frontline team members, another challenge could be the extrapolation of the VBHC implementation to ‘non-care’ departments of the hospital. Still at the conceptual level, for example, Human Resources could play a role in this cultural change, as the methodology for job requirement definition can be reoriented towards going beyond the clinical skills, to also include the ‘value skills’ identified for each clinical condition. Similarly, Teaching Departments in university hospitals/institutions can also play an important role by incorporating the VBHC model and its practical applications in the practitioners-to-be learning programmes. Those are yet to come through at our hospital.
All in all, let’s say that ‘it’s always been done this way’ plays an important role for all the stakeholders when talking about challenges.
What were the first steps you took?
The first step to be mentioned was the full convincement from the Board of Directors to implement VBHC at the hospital. This leadership was essential to communicate to all the teams that VBHC was the key point of the hospital’s growth strategy.
For the VBHC implementation, a management team with a variety of profiles (doctors, nurses, engineers, etc.) was formed. It began with redesigning the care process, identifying practices that didn’t add value, and enhancing those that did. We started with those treatment units’ processes that were ‘common ground’, such as OR, ER, inpatient wards, etc. A blueprint was developed gathering identified best practices to enhance cultural change among professionals so that they could own these changes. It was the key element of the transformation.
A year passed, and we started working on the outcomes. We introduced the patient-reported outcome measures (PROMs) as a tool to make patient needs the driver for change in the professionals. In addition, primary care was incorporated in most of the working teams. Due to that, the blueprint was redesigned so that outcome measurement and cost calculations among others were added. It should be noted that some of the activities included in the blueprint have not been developed yet at the operational level, as we need to go step by step and learn along the way.
The blueprint has been evolving ever since as we keep on identifying the best practices for cultural change to implement VBHC.
In the beginning, VdH conducted a comprehensive analysis of the existing cycle of care. What tools did you use?
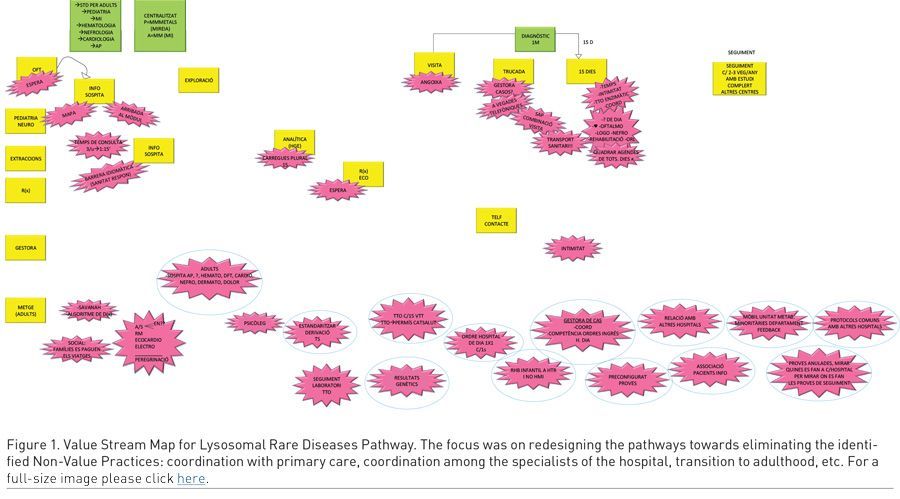
Our primary blueprint was supported by five to six sessions per clinical working group led by the management team, with the aim to empower them to lead the transformation within their units. The content of these sessions was adjusted to the group needs but mainly included training sessions on process redesign, Value Stream Mapping, cross-observation among professionals, a patient session, a development of the new working standard session and implementation of the improvement projects (Figure 1).
What were the top organisational inefficiencies/low-value activities you discovered and how did you address those?
The top non-value tasks are under the umbrella of coordination with primary care and between specialists at the hospital. These lead to information contradiction, duplicate testing, unnecessary patient and staff trips, increased waiting times, etc.
Building a new standard of clinical pathway implied creating a consensual evidence-based way of working, where all the stakeholders are represented. Normally they all need to lead the change in their units to adjust to the agreed standard, so the Deming cycle (PDCA) is set up (Figure 2).
Optimally, the process (and its changes, both current and future, resulting from continuous improvement) should be represented in the enterprise resource planning (ERP) of the institution so that the wedge in the PDCA cycle can be reaffirmed.
What kind of training did the staff require?
There are several training sessions held along our blueprint. The very first session that we carry out with clinicians is on process redesign, safety culture and clinical practice appropriateness. Here the tangible outcomes are the technical concepts and the intangible outcome is ‘breaking the ice’ among professionals of all profiles, who work in different buildings but treat the same patients. The teaching methodology for this is case-study based, and trainees participate in role playing in a very practical and dynamic way.
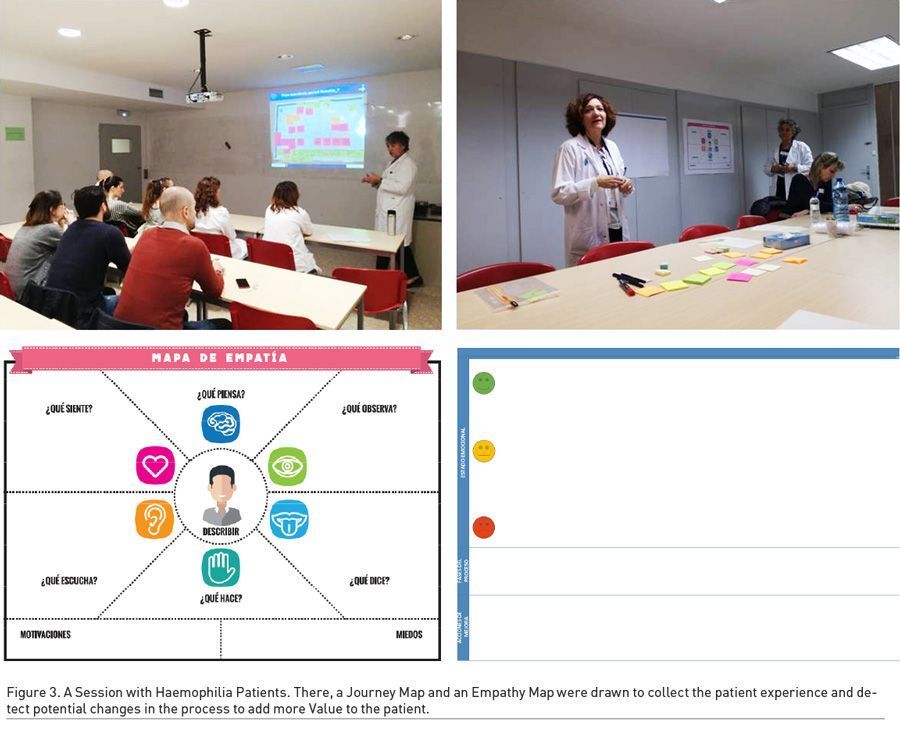
Next, a training session on the outcomes definition and potential uses is performed with the clinical team, right before the session with the patients, so that the methodology is given to transform empathy into a standardised way of measuring and working.
Right after this session comes the one with patients, led by the Citizen Care Department. With the help of an Empathy Map and a Journey Map (Figure 3), we learn about the patients’ experience through their care processes as well as the unmet needs they indicate. In the future, these sessions aim to also be a tool to identify a patient representative for each clinical condition and to incorporate them in the continuous improvement teams.
Patient education and training is named as one of the important elements of the VBHC strategy. How do you address this aspect?
During the sessions with patients, we distinguish different profiles that require different approaches. Improvement projects towards patient education and training to enhance engagement are being developed. For example, in the stroke and neurotrauma clinical pathways, patients have a visual management tool so that they can anticipate their daily agenda and discuss their therapeutic goals. Another example is a visual management board for paediatric solid organ transplantation, engaging kids to adhere to their treatment and healthy lifestyle.
We think this is just the first step on a long way. During the sessions with patients, we already feel like identifying those who in the future might be integrated in the clinical teams, so that they can actively participate in the clinical pathway redesign.
What role does technology play in VdH’s transition to VBHC? Have there been any major technological changes you had to implement along the way?
Technology plays a very important role since all the information coming from different actors (patient, caregivers, doctors, etc.) must be collected using digital tools. Furthermore, all this information has to be analysed and displayed in real time and in a simple way to allow actions to be taken. Naturally, it must be integrated with the hospital information system (HIS).
With regard to the VBHC implementation, we internally created a platform to develop:
• a tool to generate and send questionnaires and collect information from patients and/or caregivers
• an algorithm that processes the information and presents it as a diagram considering health areas around the clinical condition
• a balanced scorecard to show all relevant information using KPIs.
Please tell us more about how you receive self-reported results from patients and use these in clinical practice.
Once the data are received and processed on our server and a spider diagram is built on health areas around the disease, clinicians can anticipate the patient’s needs and a personalised care process can be built depending on each patient’s requirements.
One example for this is the objectification of a high depression rate in a group of patients. Before an outpatient clinic visit with the neurologist, these patients are referred to the psychologist/psychiatrist where the patient fill in a motivational questionnaire and the decision on the treatment is taken if necessary.
Can you give any examples of any prominent misalignments between patients’ expectations and the existing care provision that you discovered? How have you addressed those?
One such example comes from the stroke patients sessions. For these sessions, we built a Decision Tree to help us choose the patient profiles, so that we could have a variety of experiences within the same clinical condition in the room. For the stroke patient session, there were patients of all sequelae levels.
Specifically, a patient who did not have sequelae after stroke, but whose brother died of stroke, let us know how grateful she was but also how difficult it had been for her after discharge. She was told to quit smoking and was referred to primary care to join a respective programme. The woman was given a treatment, which eventually made her go to the ER as she suspected infarction. At the ER she was sent back to primary care to change her treatment. However, with the second treatment she ended up in the ER again – and so she was going back and forth, but didn’t quit smoking in the end.
What was she actually saying? Because of the silos between hospital and primary care and of how the pathways between the two are organised, it is difficult to quit smoking, i.e. to adhere to a treatment.
Out of this session a group of professionals from both primary care (led by neurologist Dr Manuel Milian) and the hospital (led by neurologist Dr Carlos Molina) was formed to work on the discharge process. Currently, this group is working on two main processes. One is a shared discharge follow-up via the Farmalarm platform. The other is an app for those primary care patients who have been identified as being at risk of stroke; the app should facilitate the change in their lifestyle.
Last year, the Paediatric Infectious Diseases and Immunodeficiencies Unit of VdH won the VBHC Dragons Endorsement prize. What are the key take-aways from this achievement?
The participation in the Paediatric Immunodeficiency Diseases (PID) Early Detection (PED) project has undoubtedly been a key factor for the VBHC implementation. Four hospitals (Ospedali Riuniti di Ancona and Ospedale Mauriziano di Torino in Italy; Hospital Universitari Vall d’Hebron in Spain; and UZ Gent University Hospital in Belgium) have worked together (Figure 4) to create a solid network involving integrated practice units (IPU), to provide patients and relatives with an early diagnosis of PID with standardised diagnostic, therapeutic and follow-up protocols and improve the quality of life for PID patients. The aim of this project is to reduce the PID diagnostic delay, which is about 8.8 years with 50% of people undiagnosed.

The results can currently be appreciated in two aspects.
The first is early diagnosis. Newborn screening for SCID and a pilot phase of the PIDCAP project with around 300,000 individuals are being implemented in Catalonia. The PIDCAP project has made possible the screening of more than 100,000 individuals. Referral rate and quality have significantly improved. Also, a PDTA has already been organised in the Marche region (Italy) with the approval granted by the Health Administration in June 2019, and is ongoing in the Piedmont region. These key figures are part of the pathway design that allows to eliminate a number of unnecessary exams and anticipates the diagnosis of PIDs.
The second one is dissemination. Colleagues from the Ghent University Hospital have set up an interactive website to raise awareness and share information about PID with primary care practitioners and non-PID specialists.
In summary, this combination of efforts constitutes a very powerful initiative that is pivotal for early diagnosis of PID. There’s still a long way to go. The PED project has a great potential to deliver superior patient value to patients with rare diseases, from newborns to elderly, decreasing mortality rates, improving patients’ quality of life and reducing costs in the whole healthcare cycle.
So far, what have been the most important ‘lessons learnt’ for VdH on its way to VBHC?
• Promotion of professional leadership and team work by building trust among the staff (conflict resolution, commitment to each another, assuming responsibilities, defining and obtaining results, identifying value from the patient’s perspective).
• Elimination of non-value activities and practices, always from the patient’s perspective.
• Change management is not easy, let’s be perseverant!
• Let’s look for the easiest way to do it. Let’s build the Minimum Viable Product and try it. Waiting for it to be complete and perfect raises frustration associated with waiting times.
• Make the problem visible, so that we can solve it.
• At the beginning, we have to go for the quick wins and make them visible to inspire the continuous improvement in our daily work.
• It is necessary to take a chance and step out of our comfort zone to grow.
• Let the team grow at their own pace and let them make mistakes when necessary, so that they are learning by doing.
Implementation of VBHC is an exciting, ambitious long-term project, and we’re just at the departure line. Let’s keep it going!
Conflict of Interest
None. 



