A recent study investigates the clinical factors influencing clinician decisions regarding fluid administration, vasopressor initiation, and vasopressor route in early sepsis. Previous concerns about fluid overload in sepsis have prompted interest in early vasopressor initiation, especially through peripheral IVs, as an alternative to central lines. While clinical trials comparing fluid-restrictive and fluid-liberal strategies have yielded neutral results, personalised approaches to resuscitation remain unexplored. Understanding how clinicians navigate resuscitation decisions in practice is crucial for informing future trials to optimise sepsis management.
The objective of the study was to gain insight into how clinicians personalise their decisions regarding resuscitation in clinical practice.
The survey study involved clinicians in the U.S. The survey was conducted between November 2022 and January 2023. Each survey contained ten vignettes depicting patients with sepsis, with randomised clinical factors such as fluid received and volume status. Respondents were asked to select the next steps in management based on the presented scenarios. Data analysis was performed between February and September 2023.
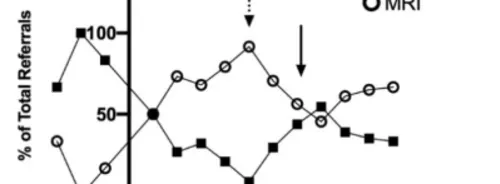
Among 11,203 invited clinicians, 550 participated in the study. Most were physicians (61.3%) and critical care trained (67.1%). Clinical decisions regarding fluid administration and vasopressor initiation were significantly influenced by factors such as the volume of fluid already received by the patient and their volume status. For instance, after 1 litre of fluid, 82.5% of respondents prescribed additional fluid, while 55.0% initiated vasopressors. However, after 5 litres of fluid, only 17.5% prescribed more fluid, while 92.7% initiated vasopressors. The patient's examination findings, such as dry or wet volume status, also influenced fluid prescription. Medical history, respiratory status, lactate trend, and acute kidney injury had minor associations with fluid and vasopressor decisions.
In cases where patients lacked central access, respondents were willing to start vasopressors through peripheral IV catheters in the majority of scenarios. However, if patients were already receiving peripheral norepinephrine, respondents were more inclined to place a central line at higher norepinephrine doses and after 24 hours compared to lower doses and earlier time points.
Findings from this study indicate that the amount of fluid already received by the patient significantly influences decisions regarding ongoing fluid and vasopressor administration, often more so than other clinical factors. Peripheral vasopressor use is prevalent in practice. Moving forward, efforts to personalise resuscitation strategies should consider fluid volumes as a key factor and may benefit from the development of tools to aid clinicians in tailoring resuscitation approaches to individual patient needs.
Source: JAMA
Image Credit: iStock