The utilisation of medical imaging has witnessed a remarkable surge in the past decade, accompanied by a concerning rise in inappropriate referrals for imaging procedures. In a bid to address this pressing issue, a recent study published in Insights into Imaging explores the efficacy of implementing a Point-of-Care Clinical Decision Support Tool (POC CDST) to mitigate inappropriate referrals and enhance the efficiency of medical imaging processes.
Rapid increase in imaging services demand may pose a challenge for patient well-being and healthcare resources.
According to data from the Health Service Executive (HSE) in Ireland, approximately 2.5 million diagnostic imaging tests are conducted annually, with a staggering 226,166 patients waiting for imaging services in 2021. This surge in imaging demand has not only exacerbated patient wait times but has also led to a notable increase in unnecessary radiation exposure associated with imaging procedures. Detrimental consequences of inappropriate imaging referrals include delayed diagnoses, increased healthcare costs, and unnecessary exposure to ionizing radiation. Moreover, studies have linked excessive imaging, particularly CT scans, to potential health risks such as thyroid cancer. It is evident that addressing inappropriate imaging referrals is imperative to safeguard patient well-being and optimize healthcare resources.
Point-of-Care Clinical Decision Support Tool leads to both clinical and environmental benefits
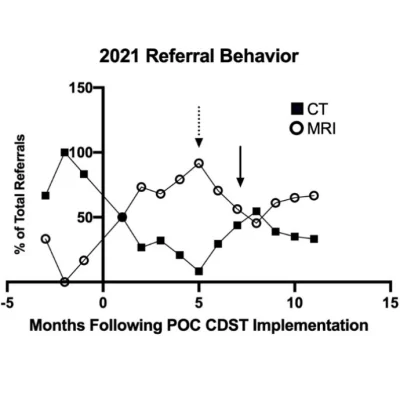
To tackle this challenge, the study evaluates the impact of implementing a POC CDST within a subset of physicians at a tertiary referral hospital in Ireland. The POC CDST integrates evidence-based imaging referral guidelines into the referring physician’s workflow, aiding in the selection of the most appropriate imaging modality for patients. By providing decision support at the point of care, the POC CDST aims to improve referral appropriateness, reduce unnecessary radiation exposure, and enhance the overall quality of patient care. The findings of the study reveal promising outcomes following the implementation of the POC CDST. There was a notable shift in referral behavior, with a preference for MRI over CT scans, resulting in a significant reduction in effective radiation dose per patient. Moreover, the study observed a substantial decrease in the volume of unnecessary duplicate imaging, leading to both clinical and environmental benefits.
Significantly, the implementation of the POC CDST not only improved the completeness of referral information but also facilitated a more efficient referral process, thereby reducing the burden on radiology departments.
Referral guidelines may drive adoption and optimize healthcare delivery
The study underscores the importance of integrating referral guidelines into the physician workflow to enhance adherence and optimize resource utilization. Despite the promising results, the study acknowledges certain limitations, including confounding variables such as the impact of external events like the HSE cyber-attack and the COVID-19 pandemic. Furthermore, future research is warranted to explore the long-term effects of POC CDST implementation on patient outcomes and healthcare efficiency. In conclusion, the implementation of a POC CDST represents a significant advancement in addressing inappropriate medical imaging referrals in Ireland. By incorporating evidence-based guidelines into the referral process, healthcare providers can make more informed decisions, thereby improving patient care and optimizing resource utilization. Moving forward, widespread adoption of POC CDSTs holds the potential to alleviate patient wait times and enhance the quality of healthcare delivery nationwide.
Source: Insights into Imaging
Image Credit: Insights into Imaging