Prostate MRI is pivotal in managing prostate cancer, employing tools like PI-RADS for detection and localization. Various MRI-based scoring systems serve multiple purposes, such as evaluating image quality, monitoring changes during active surveillance, and assessing recurrence risk after treatments. Yet, confusion persists regarding their proper application and timing within clinical workflows. Standardizing scoring systems is crucial for consistent radiological reports and effective communication with physicians. This ESR Essentials paper offers a comprehensive overview of prostate MRI tools, addressing current evidence and limitations. It also provides clear flowcharts to aid radiologists in choosing the appropriate scoring system for different clinical scenarios.
Optimizing Prostate Cancer Diagnosis: The Role of MRI and PI-RADS Scoring System
Prostate MRI conducted prior to biopsy serves as a crucial tool in optimizing the biopsy process. It effectively reduces unnecessary biopsies, ensures the detection of clinically significant prostate cancer (csPCa), and mitigates the risk of overdiagnosing indolent tumors. Recommendations advocate for MRI as a triage test for individuals with suspected prostate cancer, with PI-RADS (Prostate Imaging Reporting and Data System) guidelines being the cornerstone for MRI interpretation.
PI-RADS, initially introduced by the European Society of Urogenital Radiology (ESUR) in 2012 and updated in version 2.1, provides a standardized framework for acquiring, interpreting, and reporting multiparametric MRI (mpMRI) of the prostate. It aids in the detection and localization of clinically significant lesions in treatment-naïve men undergoing prostate MRI for suspected cancer.
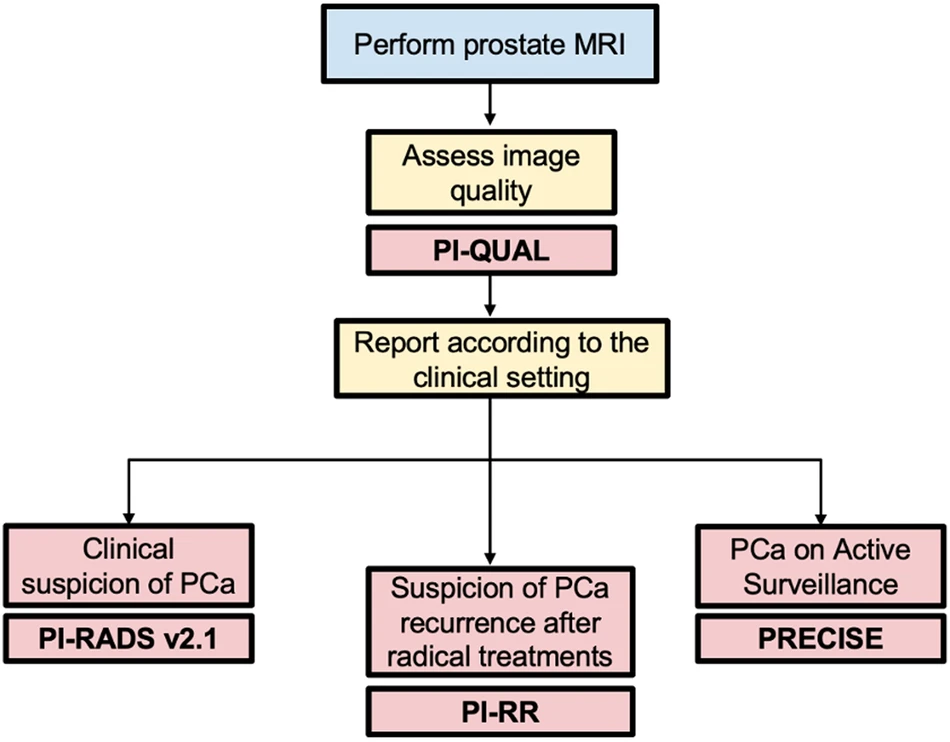
Image Credit: SPRINGER
The categorical scoring system of PI-RADS involves a 5-point scale, reflecting the likelihood of harboring csPCa for each identified lesion. This score is derived from a combination of specific findings on T2-Weighted (T2W), Diffusion-Weighted Imaging (DWI), and Dynamic Contrast-Enhanced (DCE) sequences. Notably, DCE's role is somewhat debated, and there's a growing interest in non-contrast protocols, like biparametric MRI (bpMRI), as potential alternatives to the comprehensive mpMRI.
When interpreting PI-RADS scores, it's essential to consider zone-specific assessments, distinguishing between lesions in the peripheral (PZ) and transition zone (TZ) of the prostate. DWI is emphasized for assessing PZ lesions, while T2W imaging is primary for the TZ. DCE plays a supplementary role, typically used to upgrade indeterminate PZ lesions from PI-RADS 3 to PI-RADS 4.
In clinical practice, biopsy decisions often align with PI-RADS scores. Biopsy may be considered for patients with PI-RADS 4–5 lesions, while it's generally avoided for PI-RADS 1–2. For PI-RADS 3 lesions, additional clinical factors should inform biopsy decisions. However, PI-RADS v2.1 doesn't prescribe specific biopsy options, as these decisions heavily rely on thorough risk assessment and local expertise.
The diagnostic performance of PI-RADS v2.1 is notable, with pooled sensitivity and specificity reported at 87% and 74%, respectively, for detecting Gleason score ≥ 3 + 4 cancers. The system demonstrates a step-up function for detecting csPCa with higher PI-RADS scores. Its reproducibility is also commendable, impacting clinical guidelines and patient care practices.
Overall, prostate MRI and the PI-RADS scoring system significantly contribute to the management and diagnosis of prostate cancer, ensuring more accurate and tailored patient care.
Prostate Imaging Quality (PI-QUAL) scoring system
The Prostate Imaging Quality (PI-QUAL) scoring system is designed to standardize the assessment of image quality in prostate MRI studies. It employs a 5-point scale to communicate the reliability of findings based on image quality, regardless of the purpose of the MRI. Scores range from 1 to 5, with higher scores indicating better image quality. Scores of 1 or 2 suggest that the images fall below the minimum standard, making it difficult to reliably rule in or rule out clinically significant lesions. A score of 3 indicates sufficient quality to rule in but not rule out lesions, while scores of 4 or 5 indicate adequate quality to both rule in and rule out lesions.
Research suggests that image quality, as assessed by PI-QUAL, impacts various aspects of prostate cancer detection and staging. Higher quality scans are associated with increased biopsy yields in targeted biopsy cohorts, while lower quality scans may impair MRI performance in evaluating extraprostatic extension (EPE) compared to clinical staging tools.
The PI-QUAL scoring system is continually evolving in response to clinical experience and scientific evidence. An international working group is actively collaborating on an updated version to address current limitations. This updated version aims to streamline technical parameter assessment, be applicable for evaluating non-contrast protocols like biparametric MRI (bpMRI), and separate assessments of image quality and clinical implications to broaden its applicability to various MRI applications, including active surveillance and population prostate cancer screening.
Prostate Cancer Radiological Estimation of Change in Sequential Evaluation (PRECISE) scoring system
The Prostate Cancer Radiological Estimation of Change in Sequential Evaluation (PRECISE) scoring system addresses the need for standardized reporting of radiological changes in patients undergoing active surveillance (AS) for prostate cancer. AS involves closely monitoring indolent prostate cancer rather than immediate treatment. Eligibility criteria vary across guidelines but typically include a biopsy Gleason score ≤ 3 + 4, clinical stage ≤ T2b, and serum PSA level < 10 ng/mL. The European Association of Urology (EAU), American Urological Association (AUA), and UK National Institute for Health and Care Excellence (NICE) recommend using MRI for patient selection and AS assessments.
PRECISE, introduced in 2016, evaluates radiological changes on serial imaging using a scoring system ranging from 1 to 5. Scores indicate radiological regression (1-2), stability (3), or progression (4-5) based on lesion features like conspicuity and size. Radiologists assess lesions compared to baseline scans, emphasizing the "index" lesion. Measurements should align with PI-RADS guidelines, and scans must be of high quality. PI-RADS and PRECISE are complementary, with PRECISE providing additional information on radiological changes.
However, uncertainties exist in PRECISE recommendations, especially in defining imaging changes subjectively. Variability in measurements, magnet field strengths, and background alterations can affect interpretations. An updated version (PRECISE v. 2) aims to address these uncertainties and highlight areas for further research.
While PRECISE demonstrates a robust negative predictive value (NPV), its positive predictive value (PPV) for predicting disease progression is lower. Thus, clinical factors and biomarkers should guide follow-up and re-staging biopsies, rather than relying solely on imaging changes.
Overall, PRECISE aids in standardizing radiological reporting in AS but should be used alongside clinical factors for informed decision-making regarding treatment initiation or re-biopsy.
Prostate Imaging for Local Recurrence Reporting (PI-RR) scoring system
The Prostate Imaging for Local Recurrence Reporting (PI-RR) scoring system is designed to standardize the acquisition, interpretation, and reporting of pelvic MRI in patients who have undergone whole-gland therapies for prostate cancer with curative intent, such as radiation therapy (RT) or radical prostatectomy (RP). It employs a 5-point assessment scale ranging from "very low" to "very high" likelihood of local recurrence.
MR images are acquired following PI-RADS v2.1 technical recommendations, with specific considerations for post-RP patients requiring sagittal planes. The scoring criteria are based on anatomical and functional imaging findings, with T2W images aiding lesion localization but not participating in the final assessment. DWI and DCE sequences play key roles, with DWI dominant in RT patients and DCE dominant post-RP. PI-RR scores range from 1 to 5, with 1-2 indicating no abnormalities or benign findings and 4-5 indicating suspicious lesions, primarily based on their location relative to the primary tumor site.
Retrospective validation has shown the PI-RR system to be effective in detecting local recurrence with moderate to high inter-reader agreement. However, prospective multicenter studies are still needed. Its limitation lies in assessing relapse risk only within the prostate gland or prostatic bed after whole-gland therapies. Clinical adoption may also be impacted by the preference for PSMA-PET imaging in patients experiencing biochemical recurrence post-RP.
Furthermore, two scoring systems have been proposed for evaluating residual/recurrent disease after focal therapy (PI-FAB and TARGET), although they lack clinical validation. Additionally, various other tools for prostate cancer assessment exist, such as grading systems for predicting extraprostatic extension (EPE), albeit less commonly employed.
Key recommendations
- Image quality assessment is crucial before all MRI interpretations. Uniform reporting of image quality is essential, and the PI-QUAL score is the standardized tool for this purpose (Level of evidence: moderate).
- The use of prostate MRI before biopsy is recommended as a triage test in selected patients with clinical suspicion of prostate cancer and should be acquired and interpreted using PI-RADS v2.1 recommendations (Level of evidence: high).
- PRECISE assessments are designed to be used to predict the likelihood of clinically significant radiological changes during active surveillance of prostate cancer, whereas the PI-RR scoring system estimates the likelihood of local recurrence following primary whole-gland curative treatments (Level of evidence: moderate).
Source Credit: SPRINGER
Title Image Credit: iStock






