According to a study published in JAMA, patients who receive fondaparinux after a certain type of heart attack had a lower risk of major bleeding events and death in the hospital and after six months as compared to patients who received low molecular weight heparin (LMWH). Both groups of patients had similar rates of subsequent heart attack or stroke.
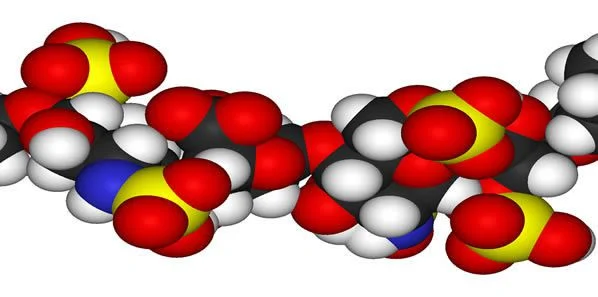
Bleeding events are associated with increased mortality and thus reduction of such bleeding events in patients receiving antithrombotic therapy is extremely important. In a large clinical trial involving patients with non-ST-segment elevation myocardial infarction (NSTEMI), fondaparinux was found to be associated with reduced bleeding events and improved survival compared with heparin. However, there is a lack of data related to the use of fondaparinux versus heparin outside of a clinical trial.
The study was led by Karolina Szummer, M.D., Ph.D., of the Karolinska Institutet, Stockholm, Sweden, and colleagues. The researchers analysed data of 40,616 patients with NSTEMI who received in-hospital treatment with fondaparinux or low-molecular weight heparin (LMWH) between September 2006 through June 2010, with follow-up through December 2010. 36.4 percent of patients received fondaparinux and 63.6 percent received LMWH.
The results showed that the absolute rate of severe in-hospital bleeding events was 1.1 percent in the fondaparinux group as compared to 1.8 percent in LMWH group. In-hospital mortality was 2.7 percent in the fondaparinux group as compared to 4.0 percent in the LMWH group. The differences in major bleeding events and mortality between the two treatments were similar at 30 and 180 days. The rate of recurrent heart attack was 9.0 percent and 14.2 in the fondaparinux group as compared to 9.5 percent and 15.8 percent in the LMWH group at 30 days and 180 days respectively. The rate of stroke was low in both groups.
Results were similar in patients with varying degrees of kidney function and in patients who had undergone early percutaneous coronary intervention.
“A randomised clinical trial is often needed to provide definite evidence and an estimate of the treatment effect in a specific, selected, well-defined target patient population. However, the effect of implementing the same treatment in clinical practice might differ and should therefore be investigated in observational cohorts and, preferably, in continuous registries with complete coverage of non-selected patients with an indication for the studied treatment. Outside of a trial setting, the treatment is given to a much more heterogeneous patient population and the treating centres and physicians are less selected. Thus, the balance between benefit and risk can differ between a randomised clinical trial and experience in a nontrial, routine clinical care setting. Therefore, experiences from clinical practice provide important complementary information,” the authors write.
Source: JAMA
Image Credit: Wikimedia Commons