According to a study published in JAMA, patients who experienced a heart attack and underwent a percutaneous coronary intervention (PCI) show a decrease in adverse clinical events when they were given anticoagulant bivalirudin following the procedure.
Compared to heparin alone or heparin plus tirofiban, bivalirudin resulted in a reduction in adverse clinical events, in particular a reduction in bleeding events.
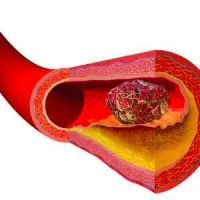
The use of antithrombotic therapy after primary PCI is critical to prevent adverse ischaemic events such as stent thrombosis as well as the occurrence of a subsequent heart attack. However, the use of such therapy should be weighed against the risk of haemorrhagic complications. In most cases, anticoagulation during primary PCI is achieved with heparin or bivalirudin. Since there have been mixed results in trials involving these drugs, the clinical safety and efficacy of bivalirudin is still uncertain.
This study was conducted by Yaling Han, M.D., Ph.D., of the General Hospital of Shenyang Military Region, Shenyang Liaoning Province, China, and colleagues. They randomly assigned 2,194 patients with AMI undergoing primary PCI at 82 centres in China to receive bivalirudin with a post-PCI infusion (n = 735), heparin alone (n = 729), or heparin plus tirofiban with a post-PCI infusion (n = 730).
Adverse events at 30 days occurred in 8.8 percent of patients treated with bivalirudin compared with 13.2 percent in the heparin group and 17 percent in the heparin plus tirofiban group. Adverse clinical events were a composite of cardiac or cerebral events (all cause death, subsequent heart attack, ischaemic-driven target vessel revascularisation or stroke), or bleeding.
Bleeding at 30 days was reduced by bivalirudin (4.1 percent) compared with heparin at 7.5 percent and heparin plus tirofiban at 12.3 percent. Bleeding requiring medical intervention was also reduced by bivalirudin.
No major differences in rates of major adverse cardiac events or cerebral events were observed between treatments at 30 days. The results remained similar at the 1-year follow-up.
“In this multicenter randomized trial [the BRIGHT trial], by reducing bleeding with comparable rates of major adverse cardiac or cerebral events and stent thrombosis, bivalirudin significantly reduced 30-day and 1-year rates of net adverse clinical events compared with both heparin alone and heparin plus tirofiban in patients with AMI undergoing primary PCI. The reduction in net adverse clinical events was consistent across multiple subgroups,” the authors write.
In an accompanying editorial, Matthew A. Cavender, M.D., M.P.H., and David P. Faxon, M.D., of Brigham and Women's Hospital, Harvard Medical School, Boston write that a tailored approach should be used when determining antithrombotic regimen in patients undergoing PCI. Those patients who are at a higher risk of bleeding such as women, patients with renal dysfunction or those who require femoral access may benefit from antithrombotic regimen that decreases the risk of bleeding. However, those at risk of thrombotic complications may benefit from regimens that reduce the risk of thrombosis. Ultimately, the goal should be to optimise patient outcomes.
Source: JAMA
Image Credit: Wikimedia Commons