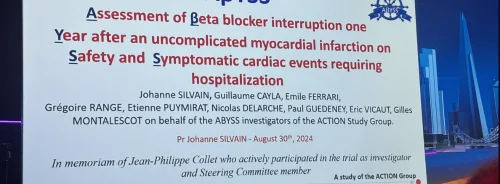
New research presented at ESC Congress 2024 showed that discontinuing beta-blockers in patients with a history of myocardial infarction (MI) did not demonstrate cardiovascular safety compared to continuation and provided no improvement in patients' quality of life.
Advancements in MI management and findings from observational studies have led to questions about the necessity of continuing beta-blockers beyond one year after MI, as unnecessary treatment could lead to side effects. The ABYSS trial aimed to provide definitive randomised data on the effects of beta-blocker interruption versus continuation on cardiovascular events and quality of life. Findings show that interrupting beta-blockers did not preserve safety in terms of clinical outcomes and offered no benefit in quality of life.
The ABYSS trial enrolled patients with a prior MI who were on long-term beta-blockers, had a left ventricular ejection fraction of at least 40%, and had not experienced cardiovascular events in the previous six months. Participants were randomly assigned in a 1:1 ratio to either interrupt or continue their beta-blocker therapy.
The primary endpoint was a composite of death, non-fatal MI, non-fatal stroke, or hospitalisation for cardiovascular reasons at the longest follow-up (minimum one year), assessed using a non-inferiority analysis (defined as a between-group absolute difference of less than 3 percentage points for the upper boundary of the two-sided 95% confidence interval [CI]). The main secondary endpoint was the change in quality of life as measured by the European Quality of Life–5 Dimensions (EQ-5D) questionnaire. A total of 3,698 patients from 49 sites in France were randomised.
During a median follow-up of three years, beta-blocker interruption was not shown to be non-inferior to continuation. The primary outcome occurred in 23.8% of patients in the interruption group compared to 21.1% in the continuation group.
Deaths occurred in 4.1% of the interruption group and 4.0% of the continuation group, while MI occurred in 2.5% and 2.4%, respectively. Hospitalisation for cardiovascular causes was higher in the interruption group (18.9%) compared to the continuation group (16.6%). The interruption of beta-blockers was also associated with increased systolic and diastolic blood pressure and heart rate at six months and throughout the study follow-up. There was no improvement in quality of life with beta-blocker interruption.
The differences observed between the groups in terms of hospitalisations for cardiovascular reasons, the negative impact on blood pressure, and the lack of improvement in quality of life do not support interrupting chronic beta-blocker therapy in post-MI patients.
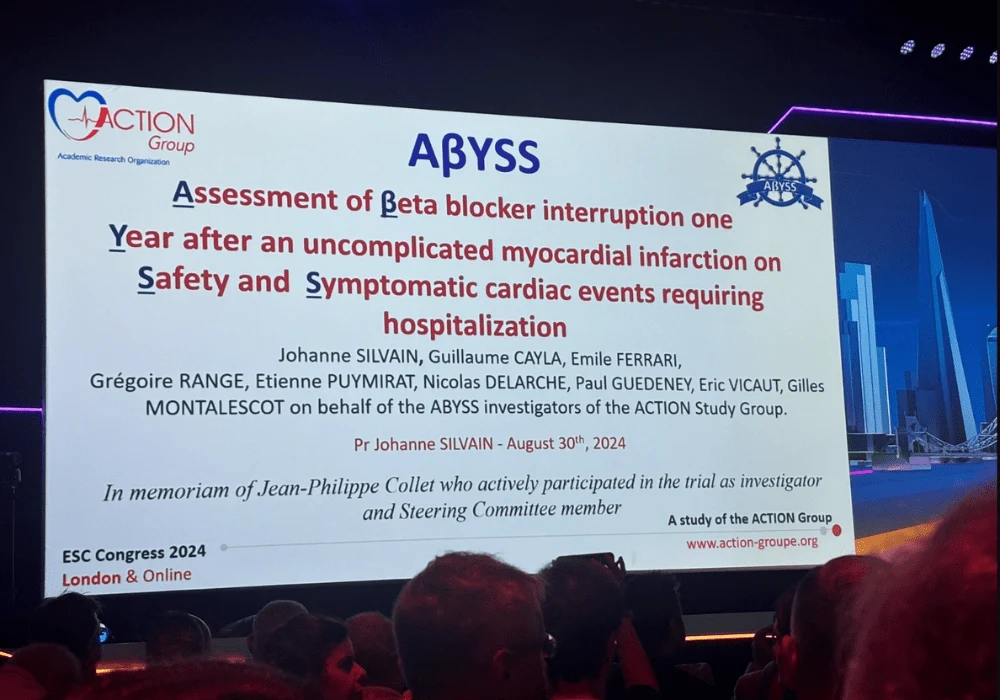
Source & Image Credit: ESC Congress 2024