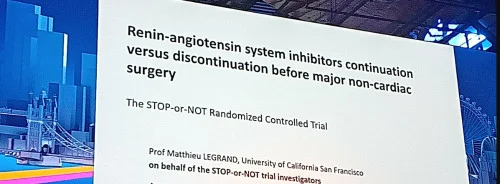
Late-breaking research presented at a Hot Line session at ESC Congress 2024 found no significant difference in major post-operative complications between patients who continued versus those who stopped renin-angiotensin system inhibitors (RASIs) before non-cardiac surgery.
Many patients undergoing major surgery have a history of hypertension, diabetes, or heart failure and are on chronic treatment with RASIs, such as angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin receptor blockers (ARBs). Due to the lack of conclusive data from randomised trials, there has been uncertainty about whether to stop RASIs before non-cardiac surgery. Continuing RASIs could lead to intra-operative hypotension, potentially causing post-operative cardiovascular events and acute kidney injury (AKI). Conversely, stopping RASIs might increase the risk of post-operative hypertension, heart failure, or arrhythmias.
The STOP-or-NOT trial was designed to resolve these uncertainties. Study results showed no difference in major post-operative outcomes between continuing or stopping RASIs. The trial was conducted across 40 centres in France. It involved patients scheduled for elective major non-cardiac surgery who had been on ACEIs or ARBs for at least three months prior. Participants were randomly assigned in a 1:1 ratio to either continue RASIs until the day of surgery or discontinue them 48 hours before, with the last dose taken three days prior to surgery. Both groups were advised to resume RASI treatment as soon as feasible after surgery, once the oral route was possible.
The primary endpoint was a composite of all-cause mortality and major post-operative complications within 28 days of surgery. Major post-operative complications included cardiovascular events (such as acute myocardial infarction, arterial or venous thrombosis, stroke, acute pulmonary oedema, cardiogenic shock, acute severe hypertension crisis, and new cardiac arrhythmias requiring intervention), sepsis or septic shock, respiratory complications, unplanned ICU admission or readmission, AKI, hyperkalaemia, or the need for surgical reintervention. Secondary endpoints included intra-operative hypotension, all-cause mortality, episodes of AKI, post-operative organ failure, and length of hospital and ICU stay within 28 days post-surgery.
A total of 2,222 patients were enrolled, with a mean age of 67 years, and 65% were male. Most patients (98%) were treated for hypertension, while 9% had chronic kidney disease, 8% had diabetes, and 4% had heart failure. At baseline, 46% were on ACEIs, and 54% were on ARBs.
For the primary endpoint, the rates of all-cause mortality and major post-operative complications were identical in both the discontinuation and continuation groups, each at 22%. The impact of discontinuing versus continuing RASIs on post-operative complications was consistent across various subgroups.
Intra-operative hypotension occurred in 41% of patients in the discontinuation group and 54% in the continuation group. The median duration of hypotension was 6 minutes in the discontinuation group and 9 minutes in the continuation group, with a mean difference of 3.7 minutes. No other differences in trial outcomes were observed.
The results from the STOP-or-NOT trial provide evidence that can inform guideline recommendations, which are currently weak. Given the lack of significant differences, both continuation and discontinuation strategies are acceptable, suggesting a tailored approach may be beneficial. A discontinuation strategy might be chosen if there is a specific concern about hypotension, while continuation may be preferred for patients apprehensive about stopping their medication or for practical reasons.
Source & Image Credit: ESC Congress 2024