A study conducted by Schranz et al. examines how integrating a Point-of-Care Clinical Decision Support Tool (POC CDST) into the workflow of head and neck cancer specialists alters referral behaviour for radiological tests. The findings, published in "Insights into Imaging," reveal significant improvements in imaging efficiency and patient safety.
Increasing concerns over inappropriate medical imaging have led to the study of a Point-of-Care Clinical Decision Support Tool (POC CDST) at a key institution. This tool, embedded directly into the physician’s workflow, aims to optimise the selection of radiological tests, thereby reducing unnecessary patient exposure to radiation and enhancing the sustainability of imaging practices.
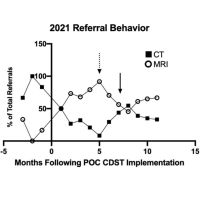
The study retrospectively analysed CT and MRI neck data from a group of specialists before and after the POC CDST implementation. It compared imaging volume, effective radiation doses, and carbon emissions from the imaging process.
Key Findings:
Reduction in Imaging Volume: The study found an 8.2% decrease in overall imaging volume and a significant 61% reduction in duplicate imaging (CT and MRI for the same condition).
Shift Towards MRI: There was a notable shift in ordering behaviour, favouring MRI over CT, which contributed to a significant decrease in radiation exposure.
Decrease in Radiation Dose: The effective radiation dose was reduced by 0.27 mSv per patient, equating to 13 fewer chest x-rays per patient.
Lower Carbon Emissions: The study also highlighted a 13.5% reduction in carbon emissions due to decreased imaging volume.
The implementation of the POC CDST significantly impacted imaging practices, evident in reduced imaging volume, radiation exposure, and carbon emissions. This approach not only benefits patients by reducing unnecessary radiation exposure but also contributes to environmental sustainability.
The results suggest that widespread adoption of POC CDSTs could greatly improve the efficiency of medical imaging referrals, potentially reducing patient wait times and healthcare costs. This approach aligns with broader goals of enhancing patient care while also addressing environmental concerns. By ensuring that the most appropriate imaging test is chosen initially, the study underscores the potential for significant advancements in both patient outcomes and healthcare sustainability.
While the study focused on head and neck cancer referrals, its implications extend to other areas of medical imaging. Further research could explore the impact of POC CDSTs across various medical specialties and healthcare settings. Additionally, investigating the tool's influence on time to diagnosis and overall patient management could provide deeper insights into its clinical benefits.
This concise article encapsulates the significant findings of the original study, highlighting the crucial role of integrated clinical decision support tools in modern healthcare. By demonstrating a tangible impact on referral behaviour, patient safety, and environmental sustainability, the study sets a precedent for future research and implementation of such technologies in healthcare systems worldwide.
Source:Insights into Imaging