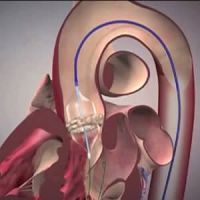
A new study that explored the relationship between procedural volume and in-hospital adverse events shows that individual operator experience with transcatheter aortic valve replacement (TAVR) plays an important role in achieving better clinical outcomes. The study is published in JACC: Cardiovascular Interventions.
The relationship between operator experience and patient outcomes is a hot topic in cardiology these days. The US Centers for Medicare & Medicaid Services (CMS) is currently evaluating whether hospitals should be required to meet prespecified volume requirements for TAVR. A decision is expected in 2019, and thus these study findings can be an indicator of how important this relationship could be.
You might also like: Cardiovascular outcomes at top-ranked vs. nonranked hospitals
The American Association for Thoracic Surgery (AATS), American College of Cardiology Foundation (ACCF), Society for Cardiovascular Angiography and Interventions (SCAI), and Society of Thoracic Surgeons (STS) have also recently issued a statement recommending an institutional minimum of 50 TAVR procedures annually and 40 AVRs per year.
This is the first time that a study has assessed the relationship between operator experience and clinical outcomes after TAVR. Generally, the focus is on institutional volume rather than individual experience.
The study analysed data from 8771 TAVR procedures in the New York Statewide Planning and Research system database. 207 operators were included in the analysis. The volume of TAVR procedures was classified as low (1-23 cases), medium (24-79 cases) and high (≥ 80 cases). 5912 patients underwent elective TAVR. 1973 were treated by low- volume operators, 1860 by medium-volume operators and 2083 by high-volume operators.
Less mortality and less risk of stroke were evident in the high-volume physician group. Reduction in death/MI/stroke was significantly evident among high-volume operators compared to low-volume operators.
The findings clearly establish an inverse association between physician volume and death/MI/stroke outcomes.
The analysis showed that physicians who performed 80 or more procedures per year had a 41% lower risk of in-hospital death, acute MI or stroke compared to operators who had performed fewer than 24 procedures per year.
Even though it is difficult to predict the ideal number of TAVR procedures per year for optimal patient outcomes, it is evident from the study findings that positive patient outcomes tend to increase after the first 100 procedures. Study investigators also highlight that the first 20 procedures are also critical and anything between these two numbers can have an impact on patient outcomes.
Overall, it seems obvious that the more TAVR procedures an operator performs, the better they become at it and the better the outcomes tend to be. These findings are important because so far, the focus has always been on institutional volume and outcomes.
During this analysis, the researchers took into consideration the initial learning curve. Early cases were excluded to account for this learning. Even then, a clear relationship was evident between volume and outcomes. Operators who performed 200 procedures in the year prior had a 59% lower risk of post-procedural stroke and a 55% lower risk of death/MI/stroke compared with operators who performed only one TAVR. A lower event rate was observed in operators who performed more than 300 TAVR procedures annually.
Overall, it seems obvious that the more TAVR procedures an operator performs, the better they become at it and the better the outcomes tend to be. These findings are important because so far, the focus has always been on institutional volume and outcomes.
During this analysis, the researchers took into consideration the initial learning curve. Early cases were excluded to account for this learning. Even then, a clear relationship was evident between volume and outcomes. Operators who performed 200 procedures in the year prior had a 59% lower risk of post-procedural stroke and a 55% lower risk of death/MI/stroke compared with operators who performed only one TAVR. A lower event rate was observed in operators who performed more than 300 TAVR procedures annually.
Image Credit: iStock
References:
Salemi, A et al. (2018) Individual Operator Experience and Outcomes in Transcatheter Aortic Valve Replacement. JACC: Cardiovascular Interventions. DOI: 10.1016/j.jcin.2018.10.030
Latest Articles
TAVR, transcatheter aortic valve replacement, individual operator experience
A new study shows that individual operator experience with TAVR plays an important role in clinical outcomes. More experience generally translates into better outcomes and vice versa.