Staff shortages in radiology departments pose an organisational challenge. Shaping up a thriving interdisciplinary team within a radiology department can be an option to alleviate shortage by fostering a culture of reshuffling tasks. The problem can be described as assessing the right number of people with the right skills in the right place at the right time, to provide the right services to the right people. In this session chaired by Joseph Castillo(Malta), lecturers shed a light on the advantages of interdisciplinary relationships in clinical work and education.
Building bridges and exploring the value of other healthcare professionals within the radiology department
Lyanne Molenaar (Netherlands) outlined that work-life balance and personal growth aspirations are compromised by the workload induced by administrative tasks and complex cases. In addition to efforts aimed at improving staff retention, reshuffling tasks can appear as a solution. Radiology department should be seen as an interdisciplinary ecosystem where radiologists, radiographers and support workers work hand-in-hand for the patient’s interest. It is important to recognize the value of the radiographer and support roles, and foster synergies between radiology professionals to create a lattice of value for the patient and balance better the workload.
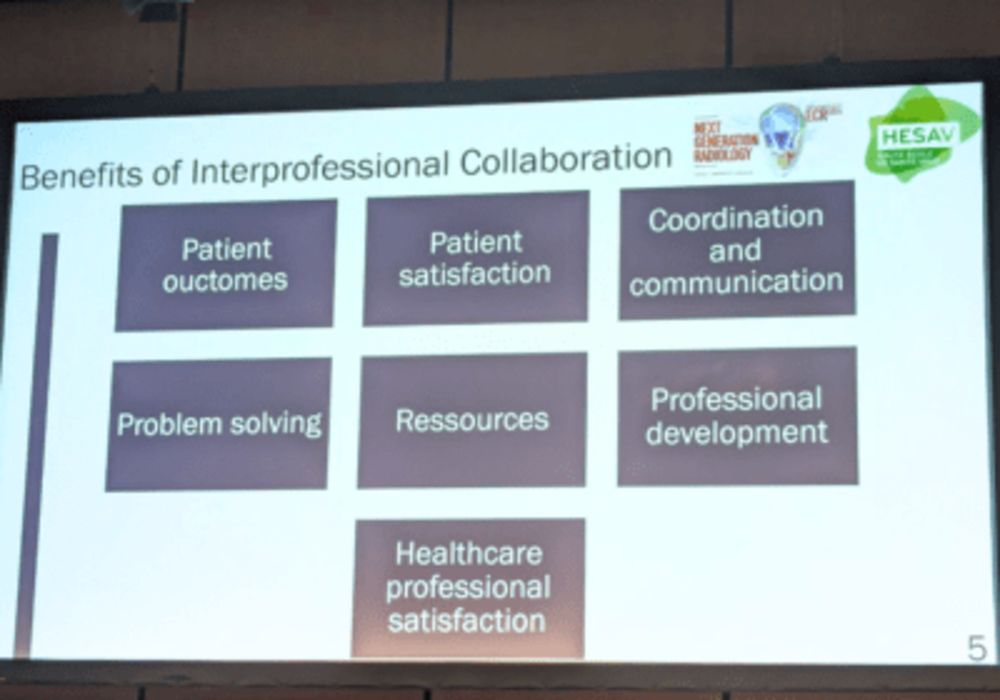
Celebrating the value offered by multidisciplinary collaboration in the radiology department can bring many positive outcomes: Job satisfaction increase for radiographers and support, reduced workload for the radiologist, cost-effectivity, patient-centred care, increased patient experience gains and additional personal development opportunities.
Common challenges are local legal barriers, trust between professional groups, education funding, supervisor capacity. Appreciating all roles in the radiology department and allowing for task reshuffling can also blur boundaries, but it’s important to focus of what can be gained from this paradigm shift.
Interprofessional education to enhance patient-centred care
Interprofessional synergies and emulation are more valuable the earlier they are implemented, Switinder Singh Ghotra (Switzerland) outlined the benefits of interprofessional education. A framework was used to combine five learning processes within a jointly designed 3-week interprofessional education (IPE) programme. The interprofessional training programme focused on person-centred care enhanced critical thinking through the development of five skills: interprofessional communication, role clarification, team functioning, conflict management and leadership.
Interprofessional collaboration can be defined as two or more professionals with different background meeting, interacting, learning together and practicing. The patient is at the centre of care.
Interprofessional education (IPE) is fundamental to developing future healthcare professional and the benefits are numerous:
- Improved collaboration skills
- Respect collaboration and role
- Positive attitudes towards interprofessional collaboration
- Work to improve patient outcomes
- Improve quality of care and patient safety
- Inclusion of patients and their families is valuable
- Break stereotypical attitudes, power-based relationships, beliefs and values
Interprofessional activities require collaboration and impose high demands on team dynamics in order to share knowledge and mental models, to share decision-making and to share problem-solving. Obstacles to building a common understanding can arise, due to the potential confrontation on divergent views related to professional culture, team building skills, power relationships, shared decision making and different beliefs and values. Same challenges can emerge in teacher/students situations.
The framework deployed at HESAV to create a 3-week interprofessional education programme was applied to 1000 students over 3 years among various training fields: Nurses, midwives, radiographers, physiotherapists and occupational therapists. The care situations covered in the program focused on patient routes, trajectories or itineraries; emphasis was placed on daily care situations and learning activities were gradually incremented by the complexity of patients’ situations and the interactivity of the students. Training objectives were to acquire collaborative practice skills, teaching and learning must be shaped/adapted. Education sessions focused on three cross-cutting objectives:
- Articulate educational (learning outcomes) with practical process (health outcomes).
- Combine intra- with inter- learning to building interprofessional existing programs. by committing into collaboration new and
- Build a common vision based on PCC and safety approach, their trajectories and their care by evaluating their local context to determine their needs and capabilities.
It is important not to confuse inter-professionalism with the sharing of skills. The development of skills in collaborative practice requires the combination of various types of skill components: personal, social, technical and methodological. The way students interact is fundamental in achieving the expected learning outcomes: cognition, critical thinking, and transfer of knowledge.
Critical thinking is defined as the mental process of actively and skilfully perception, analysis, synthesis and evaluation of collected information through observation, experience and communication that leads to a decision for action. PCC mobilised five main critical thinking processes:
- Working with the beliefs and values of patients and families
- Engage authentically with the person
- Providing a sympathetic presence
- Share decision-making
- Offer holistic care
In conclusion, interprofessional education is vital for the healthcare system, but needs the development of educational frameworks which are complex and need to take into consideration many aspects and barriers. Critical thinking is fundamental to enhancing interprofessional education and patient-centred care. Radiology professionals need to collaborate, research and work together towards the future development of interprofessional education for better patient-centred care.