ICU Management & Practice, Volume 24 - Issue 1, 2024
Critical care pharmacists have grown in numbers and effectiveness, but their need exceeds availability. Their contributions, role, and benefits are discussed with how to justify adding these highly trained practitioners to your critical care team.
Introduction
I was asked recently what the most important change I had seen during the last four decades of critical care (CC) pharmacy. While there have been amazing advances in technology for monitoring and treatment and important new categories of pharmaceuticals, from my biased perspective, I would suggest that the coalescence of multiple professionals who work together as a CC team to treat patients and apply these advances is a major improvement. Clearly, not one specialty is enough in the complex critical care environment, and the team concept and contributors continue to expand and improve. However, 50 years ago, pharmacists and the pharmacy team were not a consistent part of critical care. Thankfully, the current model of team-based intensive care unit (ICU) care now includes pharmacists as essential members contributing to improved use of medications and monitoring therapeutic effects, development and utilisation of quality improvement processes, education of colleagues, patients and families, and scholarly work that advances knowledge through publication (Haupt et al. 2003). Unfortunately, many places lack these valuable team members for several reasons, including an insufficient number of trained pharmacists, concern with the salary cost of specialty pharmacists, or failure of CC team members to recognise their benefit, as will be discussed.
Clinical Pharmacist Defined
Clinical pharmacists are those individuals who provide direct patient care in a host of different settings. Clinical pharmacy, defined by the American College of Clinical Pharmacy (ACCP), "is a health science discipline in which pharmacists provide patient care that optimizes medication therapy and promotes health, wellness, and disease prevention. The practice of clinical pharmacy embraces the philosophy of pharmaceutical care; it blends a caring orientation with specialized therapeutic knowledge, experience, and judgement for the purpose of ensuring optimal patient outcomes”. As a discipline, clinical pharmacy also has an obligation to contribute to the generation of new knowledge that advances health and quality of life (ACCP 2024). Specialised clinical pharmacists follow the medical structure model and are found in a wide spectrum of adult and paediatric practice areas. While the International Pharmacy Federation has outlined a framework for advanced pharmacy specialisation, the definitions and focus vary by country (Galbraith and Bates 2015; Bates et al. 2020). These highly trained individuals can be found worldwide.
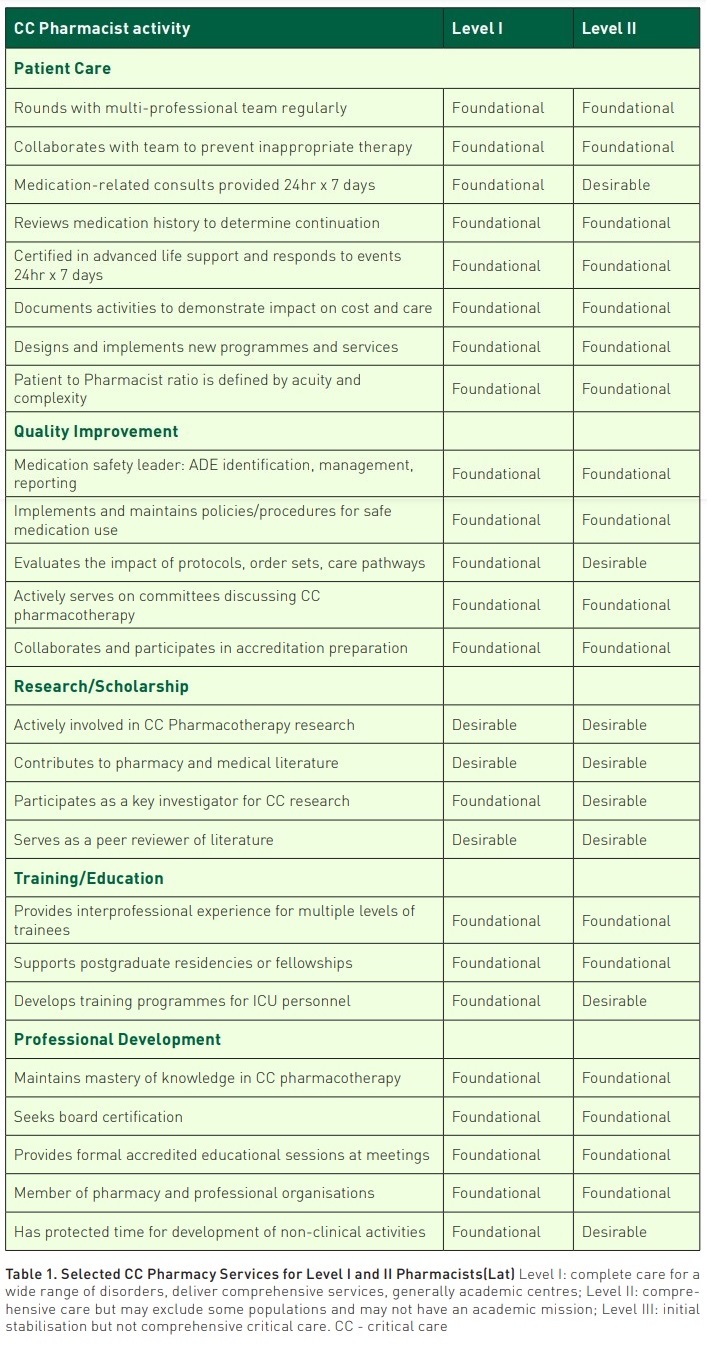
Critical care pharmacists have detailed basic clinical duties and defined specific roles and services to be provided for patient care, quality improvement, research/scholarship, training/education, and professional development at a foundational level or a desirable level, depending on the level of CC service (Lat et al. 2020) (Table 1). In practice, however, a broad range of clinical and nonclinical services were reported in a 2018-2019 survey of pharmacists and physicians to illustrate how time was allocated and what features were available in medication use systems to support their role (MacLaren et al. 2021). In summary, 50% (Interquartile range (IQR) 40-60%) of time was spent on patient care, 10% (IQR 8-16%) on teaching, 8% (IQR 5-18%) on order processing, 5% (IQR 2-10%) administrative work, 5% (IQR 0-10%) scholarship, and 5% (IQR 0-10%) on non-ICU patient care.
Preparation for these CC specialists is generally accomplished through additional advanced training programmes after meeting general pharmacist licensure criteria. The U.S. pharmacy postgraduate year-1 (PGY-1) is focused on general skills and experiences in a broad range of patient care populations. The PGY-2 specialty residency training programme for critical care has grown substantially (over 205 programmes in 2020) and now includes related programmes in emergency medicine pharmacy. This rigorous 1-year programme encompasses clinical training in various ICU types, research, teaching certification, and quality improvement activities following a specialty standard and CC-specific requirements (ASHP 2023). Successful completion of these intensive programmes prepares a pharmacist to practice at an elevated level in critical care and achieve board certification. How those individuals practice is subject to significant variability and may benefit from greater consistency in job description. Other models for preparation and achievement of required milestones have been developed elsewhere (Choudhary and Newham 2020). The U.K. model for Advanced Level Practice follows several years of structured experiential activities and is now a programme of the Royal Pharmaceutical Society (RPS). It includes a competency framework, syllabus and credentialing but has not been utilised as extensively as desired, based on the volume of care needed, but numbers have improved (Seneviratne et al. 2017). Key components of the development programme include mentorship, organised networks for education and training, supervision of research/projects, integration of trainees into a multi-professional team for experience, education, and skill development and teamwork- both in CC and within the pharmacy with a training ladder and definition of key milestones. Achievement of the highest-level practice, called Consultant/Mastery, gives independent prescribing privileges. A 2020 survey found that 72% of responding advanced care ICUs had a prescribing pharmacist on the team (Borthwick et al. 2023). Some level of prescriptive authority similarly exists in the U.S. based on local practice agreements or protocols and state law. A survey of CC pharmacists in the U.S. reported dependent prescriptive authority was available to 51.1% and independent authority to 13.4% in 2019 (MacLaren et al. 2021).
Board certification is a tool to demonstrate competency via examination since 2015. At least 4230 pharmacists worldwide are board-certified critical care pharmacists using the title BCCCP. While the majority are in the U.S. (3753), many are elsewhere, including Canada (41), Egypt (21), Saudi Arabia (29), Singapore (18), Taiwan (12), United Arab Emirates (15), Netherlands (8), Hong Kong (4), Qatar (8), and Thailand (4) and more (BPS 2024). It is an important credential for individuals and a tool for screening job candidates. Board certification is a required element for the Society of Critical Care Medicine (SCCM) to consider eligibility for fellowship in the American College of Critical Care Medicine (ACCM).
Pharmacy Team
The continuum of optimal medication use as a component of patient-centred care starts with the identification of all prescribed, non-prescription medications and supplements that are taken by the patient, and to describe those that are not properly utilised, as non-adherence is a frequent contributor to hospital admission. Continuing essential medications also helps avoid withdrawal reactions. Transitions of care warrant re-evaluation of medications to de-escalate treatments and avoid unnecessary, prolonged use. Many members of the pharmacy team (generalist pharmacists and technicians) contribute to accurate medication histories.
Medications must be supplied in a timely manner and in a form that is safe and efficient for the other caregivers. The pharmacy team additionally includes compounding and operational pharmacy specialists who ensure that the medication supply chain is optimised. Ready-to-administer products can increase safety but, importantly, can increase nursing efficiency in the face of greater patient volume, complexity, number of medications, and reduced staffing.
Workforce Development and Expansion
Optimal staffing of CC pharmacists overall is still a dream in many settings, and more fundamental roles for pharmacy staff have yet to be implemented. A growing number of pharmacists are available 24 x 7 (actual or virtual) to meet the rapidly changing needs of critically ill patients (Kruer et al. 2023). The addition of an evening pharmacist in one hospital led to a mean of 9.8 interventions accepted per day with significant cost avoidance (Chase et al. 2023). However, the process of expanding coverage and the number of positions is not clear-cut for pharmacists, as additional nurses, midlevel providers, and physicians are also needed. Many questions remain unanswered regarding the optimal intensity of CC pharmacist staffing, and additional tools are needed to quantify the impact.
The Medication Regimen Complexity score for the ICU (MRC-ICU) has been developed as an indicator of the volume and complexity of medications for a given patient or population of patients, and additional research is ongoing to determine how this information can best be measured and utilised (e.g. to allocate staffing on a given day or as a dependent variable in the measurement of how staffing may affect patient outcome) (Sikora et al. 2022). The feasibility of embedding this scoring tool into the electronic medical record (EMR) has been demonstrated and would expedite the collection of this data (Newsome et al. 2021; Webb et al. 2023).
The best patient-to-pharmacist ratio is undefined and will vary based on the contributions of support staff, such as technicians to collect medication history, additional pharmacists who manage the operations and verification of medication orders, and other responsibilities such as scholarly work, education, and quality improvement. While a ratio of one specialist to approximately 15 patients is often cited as optimal, a median ratio of 17 (IQR 12-26) was reported in a survey of CC pharmacists (MacLaren et al. 2021), and a higher ratio was reported by more than 80% of respondents in an earlier survey- and considered likely unsafe (Newsome et al. 2019). The largest assessment reported a ratio of 26.8 ± 22.1 patients per pharmacist (Rech 2021).
Expanding services to a greater number of patients or needing to cover two service teams was associated with a lower rate of acceptance of interventions compared with coverage of a single service (Smetana et al. 2023). Numerous factors likely contribute to diminishing returns, including communication methods (phone or messaging compared with in-person), lack of team cohesiveness, lack of trust or fear of speaking up.
Excessive workload caused by covering a larger number of patients than is optimal may lead to pharmacist dissatisfaction, turnover and burnout, just as experienced by other members of the care team (Vincent et al. 2019; Ball et al. 2020). A report prior to the initiation of the pandemic suggested that 64% of CC pharmacists surveyed had at least one component of burnout and is likely unchanged in the current CC environment. A higher staffing ratio has led to reduced quantity and intensity of pharmacist interventions and could lower the ability to effectively improve patient outcome (Sikora et al. 2022). Burnout strategies that have been proposed for other professionals, such as reducing the upstream stressors of EMR inefficiency, inadequate technician utilisation, or excessive trainee assignment in a teaching setting, will also be needed for pharmacists.
Metrics
Clinical pharmacists have documented the impact of their interventions in patient care worldwide and summarised in a recent scoping review on papers from nine countries (Crosby et al. 2023). Interventions typically include adverse event avoidance, reduced length of stay (LOS), reduced costs, and intervention acceptance rate. Evaluations have focused on specific aspects of medication use (sedation, analgesia, antimicrobial use, diabetes regimens, heart failure, and renal replacement therapy, among other topics) as well as overall ICU populations. It is impossible for a pharmacist to take credit for patient-level metrics (morbidity, mortality, LOS, etc.) when care is provided with a team, and there may be reporting bias in the literature. Quantitative measurement of interventions may dilute the impact of high-value activities such as adverse event prevention, individualisation of care, and improved use of resources. Many different methods are used in practice to track productivity, leading to greater difficulties in comparison between sites (Forehand et al. 2022). Economic evaluations of pharmacists have been reported with varying methodologies and often lack robust analysis, but recent studies have improved design.
A Delphi process was used to define important cost-effectiveness interventions for CC teams without assigning responsibility, although pharmacists can be important contributors (Kansal et al. 2023). A report of pharmacist-led quality improvement interventions that included protocolised monitoring of medications, mode of ventilation, antimicrobial stewardship, and reduction of invasive catheters were associated with reductions in ICU and hospital LOS, along with overall drug cost savings of €10,840 per month (95% confidence interval (CI) €10,727 to 10,952) (Leguelinel-Blache et al. 2018). Most reports are more focused on medication utilisation.
The Pharmacist Avoidance or Reductions in Medical costs in CRITically ill adults (PHARM-CRIT) study was a multicentre, prospective, observational study of CC pharmacist interventions in 2018-2019 (Rech et al. 2021). Pharmacist interventions (n=55,926) within 38 categories were reported. The quantity accepted, and potential impact (using a defined cost per intervention) suggested a mean cost avoidance of $418 US per intervention, $845 per patient day, and $7435 per pharmacist shift. The potential return on investment (ROI) was between $3.30 to $9.60 per dollar of salary. While bias in reporting could have influenced these values, prior studies reported ROI values as high as $24 to 1 (Hammond et al. 2019). The most common category of intervention was for individualisation of therapies (52.4%), and these represented 42% of total cost avoidance. Generalisability of this ROI data to other sites is difficult, despite the number of participating pharmacists and practice settings, but this serves as a resource for justification of new positions.
Internationally, pharmacists have also reported economic impact, and a few will be highlighted. Data from the Netherlands, where CC pharmacists have practiced for over a decade, demonstrated cost avoidance, cost savings, a net cost benefit of €64-78 per monitored patient day and a cost: benefit ratio (including salary and benefit costs) of €3.23-3.34, (sensitivity analysis 2.41 – 5.28 to 1) depending on the specific ICU measured (Bosma et al. 2018). Similarly, in Singapore, where pharmacists have practiced in CC for decades, a recent report described total and net cost avoidance from pharmacist intervention for a net ROI of 3.99 to 1 for pharmacist salary (sensitivity analysis 1.07 to 4.29 to 1) (Chan et al. 2021).
Inconsistent patient populations between ICUs make cost impact comparison difficult, and a system to measure medication intensity/complexity is proposed, along with other patient severity-of-illness measures. In a multicentre observational study that included 3908 patients at 28 centres, the MRC-ICU score was significantly associated with higher mortality (odds ratio 1.09, 1.08-1.11), LOS, and the total number of pharmacist interventions (Sikora et al. 2022). Mortality rate tripled from the lowest to highest quartile of the MRC-ICU score (7.8% to 24.8%, p< 0.01). Multivariate regression analysis maintained that the MRC-ICU score was significantly associated with mortality and that a higher patient-to-pharmacist ratio was associated with longer LOS and reduced quantity and intensity of interventions. The mean staffing ratio was 26.8 ± 22.1 patients per pharmacist, indicating a significant workload for many pharmacists, although it was not a significant factor for mortality prediction. Thus, it is safe to conclude that CC pharmacists participating actively in bedside care have a valuable impact on drug costs.
Pharmacist intervention patterns may change over time, as other clinicians on the team learn best practices and require less prompting for standard changes such as intravenous to oral therapy or discontinuation of stress ulcer prophylaxis when the need is gone (Leguelinel-Blache et al. 2018). However, in an academic model where team members rotate off service, the dedicated pharmacist has a greater influence in ensuring consistency of practice and continuity of care with new team personnel. Full utilisation of decision support tools with more automated responses in the EMR may also facilitate lower-level task completion with minimal personnel time.
Medication errors remain frequent, can worsen patient outcomes and incur extra costs. A recent report of hospital-wide adverse events found that 39% were medication-related adverse events despite the use of systems and technology to minimise occurrence (Bates et al. 2023). In 2010, prolonged hospitalisation resulted from voluntarily reported ICU medication errors and associated with harm in 12% of cases (Kane-Gill et al. 2010). Underreporting of events is typical. Thus, avoiding medication-related adverse events is a key role for CC pharmacists working at the point of administration and facilitating proper orders. Activities such as individualising medication doses for organ function, appropriately scheduling doses, continuing medications that could result in withdrawal symptoms, and discontinuing duplicative agents are important for optimal patient outcomes. De-escalation of unnecessary therapies (antimicrobials, fluids, sedatives, analgesics, etc.) has a significant potential to avoid unnecessary drug costs and limit adverse effects, but estimating the actual cost of what has been prevented is fraught with potential error. Assumptions must be made about the potential duration without intervention. Ensuring application of protocols for prevention of complications (venous thromboembolism prevention, delirium screening, improved timeliness of stroke thrombolysis or antimicrobial initiation in sepsis, etc.) are other significant roles for pharmacists (Leguelinel-Blache et al. 2018).
Organisational Roles
Critical care pharmacists were not identified specifically when SCCM was formed in 1972, although roles for allied health professionals were predicted, and pharmacist membership has grown to exceed 1800 members of this multi-professional organisation. Pharmacists have served in all leadership roles, including president, chancellor of the ACCM, programme chair, committee chair, journal editorial board member, guideline author, and section and chapter chair. Active participation allows pharmacists to build a network, gain leadership experience and training, become more familiar with best practices and innovative research, and serve as a forum for presentations. Serving alongside other members of the CC team can inform them of this valuable resource and facilitate growth in the profession by creating advocates at other sites.
Other professional organisations foster similar opportunities, and CC pharmacists have participated in CC and pharmacy organisations worldwide. These external forums enhance expertise that translates to similar roles at local practice sites and academia.
Creating Critical Care Pharmacy Roles
Settings without or with inadequate CC pharmacist participation will need a strategic plan to facilitate expansion. Critical care personnel and pharmacy administrators should plan together. A needs assessment of processes that need improvement, which costs could be avoided, or need for programmes to enhance medication safety, education, or optimise medication usage is an important initial step. Pilot projects to collect preliminary data will help build the business plan. Applicable literature should be summarised. Availability of trained CC pharmacists may be a limitation that could require facilitation of training using existing clinical pharmacists.
Creation of a business case for expansion of services and personnel is needed to sell the idea to administrators and describe how expansion of employee numbers (a fixed expense) can reduce other costs. A business plan template has been published and more fully describes the necessary structure and elements, and specific examples have been published (Erstad et al. 2016; Forehand et al. 2023). Medications used in the ICU contributed over 30% of one health-system drug costs in 2012 and had increased by a mean of 5.8% yearly (Altawalbeh et al. 2018). The factors contributing to cost escalation included generic medications (fewer producers, exclusivity), drug shortages, device changes, and expensive new treatments as contributors (Flannery et al. 2017). The ability to keep critically ill patients alive for longer LOS and with more complex treatments is also a potential factor. Mitigation of rising costs is neither simple nor a singular task. The CC team must evaluate drug cost data, evaluate alternatives, and, importantly, take ownership to manage medication utilisation- from prescribing to monitoring and de-escalation. The ROI of a pharmacist has been described as highly beneficial to the organisation relative to cost avoidance, but their input on all aspects of medication optimisation is essential.
The job description should include at least the minimal expectation for the position and should be compatible with the needs assessment and team goals. Metrics for quality and safety outcomes, as well as economic impact and productivity, should be defined along with timelines for initiation and development. Evolution of the role is expected, and the job description should be reassessed frequently in the first year and then annually with revision of duties and goals and elimination of less useful activities as needed.
The addition of a new CC team member may require some change in focus for the entire team, and prospective planning will improve communication and teamwork as roles are redefined. Asking other team members to relinquish some of their tasks may be uncomfortable but can be balanced with the opportunity to add new activities. Defining a format for expanded team-based rounds has the potential to maximise personnel utilisation, participation, patient/family engagement, and teamwork (Real et al. 2020; Lane et al. 2013).
Future
While CC pharmacists have been actively improving patient care in a growing number for over four decades, additional challenges remain, including an inadequate workforce to meet the worldwide needs of critically ill patients. Nevertheless, active CC pharmacists continue to explore new roles and areas for involvement in patient care, initiation, modification, and discontinuation of drug therapy within the context of team-based care (Buckley et al. 2023).
Conclusion
Pharmacists have accomplished a lot in the last four-plus decades and continue to expand roles for optimal CC patient care outcomes and efficient medication utilisation. Structure and important activities have been defined, and metrics to measure impact continue to improve. Although the number of training programmes has expanded, the needs in individual countries may far outstrip the available workforce. Critical care clinicians who do not have a CC pharmacist or do not have consistent coverage will need to work with pharmacy and hospital administrators to advocate for them. Pharmacists in those CC positions are challenged to continue to improve and document their effectiveness and impact to help make the business case for expansion in their setting and others.
Conflict of Interest
None.
References:
ACCP. Definition of a Clinical Pharmacist. Available at https://www.accp.com/about/clinicalPharmacyDefined.aspx
Altawalbeh SM, Saul MI, Seybert AL et al. (2018) Intensive care unit drug costs in the context of total hospital drug expenditures with suggestions for targeted cost containment. J Crit Care. 44:77-81.
ASHP. Accreditation standard for postgraduate pharmacy residency programs, 2023. Available at ASHP-Accreditation-Standard-Guidance-BOD-Approved-FINAL-2023-0915
ASHP. Required competency areas, goals, and objectives for postgraduate year two (PG-2) critical care pharmacy residencies (2017) Available at PGY2 Critical Care Pharmacy Residency Goals and Objectives (ashp.org)
Ball AM, Schultheis J, Lee H-J, Bush PW (2020) Evidence of burnout in critical care pharmacists. Am J Health-Syst Pharm. 77:790-796.
Bates I, Bader LR, Galbraith K (2020) A global survey on trends in advanced practice and specialisation in the pharmacy workforce. Int J Pharm Pract. 28:173-181.
Bates DW, Levine DM, Salmasian H et al. (2023) The safety of inpatient health care. N Engl J Med. 388:142-153.
Board of Pharmacy Specialties (BPS). Statistics. Available at https://portalbps.cyzap.net/dzapps/dbzap.bin/apps/assess/webmembers/managetool?webid=BPS&pToolCode=certrecord&pRecCmd=StatsByLocation&pLandScape=Yes
Bondi DS, Acquisto NM, Buckley MS et al. (2023) Rewards, recognition, and advancement for clinical pharmacists. J Am Coll Clin Pharm. 6:427-439.
Borthwick M, Barton G, Ionnides CP et al. (2023) Critical care pharmacy workforce: a 2020 re-evaluation of the UK deployment and characteristics. Human Resource Health. 21, 28.
Bosma BE, van den Bemt PMLA, Melief PHGJ et al. (2018) Pharmacist interventions during patient rounds in two intensive care units: Clinical and financial impact. Netherland J Med. 76:115-124.
Buckley MS, Acquisto NM, Adams C, et al. (2023) Critical care pharmacy practice advancement recommendations on direct patient care activities: An opinion of the American College of Clinical Pharmacy Critical Care Practice and Research Network. J Am Coll Clin Pharm. 6:925-933.
Chan LEJ, Soong JL, Lie SA (2023) A cost avoidance study of critical care pharmacists’ interventions in a tertiary institution in Singapore. Am J Health-Syst Pharm. 80:267-283.
Chase AM, Forehand CC, Keats KR et al. (2023) Evaluation of Critical Care Pharmacist Evening Services at an Academic Medical Center. Hospital Pharmacy.
Choudhary T, Newham R (2020) The advanced clinical practice pharmacy role and its implementation to practice in England. Pharm Educ. 20: 215-224.
Crosby A, Jennings JK, Mills AT et al. (2023) Economic evaluations of adult critical care pharmacy services: a scoping review. Int J Pharm Pract. 31:574-584.
Erstad BL, Mann HJ, Weber RJ (2016) Developing a business plan for critical care pharmacy services. Hosp Pharm. 51:856-862.
Flannery AH, Pandya K, Laine M et al. (2017) Managing the rising costs and high drug expenditures in critical care pharmacy practice. Pharmacother. 37:54-64.
Forehand CC, Fitton K, Keats K et al. (2022) Productivity tracking: a survey of critical care pharmacist practices and satisfaction. Hosp Pharm. 57:273-280.
Forehand C, Keats K, Amerine LB, Sikora A (2023) Rethinking justifications for critical care pharmacist positions: Translating bedside evidence to the C-suite. AM J Health-Syst Pharm. 80:1275-1279.
Galbraith K, Bates I (2015) FIP Advanced Practice and Specialization in Pharmacy: Global Report 2015 Available at https://www.fip.org/file/1397
Hammond DA, Flowers HJC, Meena N et al. (2019) Cost avoidance associated with clinical pharmacist presence in a medical intensive care unit. JACCP. 2:610-615.
Haupt MT, Bekes CE, Brilli RJ et al. (2003) Guidelines on critical care services and personnel: Recommendations based on a system of categorization of three levels of care. Crit Care Med. 31:2677-2683.
Kansal A, Latour JM, See KC et al. (2023) Interventions to promote cost-effectiveness in intensive care units: consensus statement and considerations for best practice from a multidisciplinary and multinational eDelphi study. Crit Care. 27:487.
Kane-Gill SL, Kowiatek JG, Weber RJ (2010) A comparison of voluntarily reported medication errors in intensive care and general care units. Qual Saf Health Care. 19:55-59.
Keats K, Sikora A, Heavner MS et al. (2023) Optimizing Pharmacist Team-Integration for ICU patient management: Rationale, study design, and methods for a multicentered exploration of pharmacist-to-patient ratio (OPTIM). Crit Care Explor.
Kruer RM, Czosnowski Q, Miller EM et al. (2023) Expansion of around the clock critical care and emergency medicine clinical pharmacy services at a large urban academic medical center. J Am Coll Clin Pharm. 1‐11.
Lane D, Ferri M, Lemaire J et al. (2013) A systematic review of evidence-informed practices for patient care rounds in the ICU. Crit Care Med. 41:2015-2029.
Lat I, Paciullo C, Daley MJ et al. (2020) Position paper on critical care pharmacy services: 2020 update. Crit Care Med. 48: e813-e834.
Leguelinel-Blache G, Nguyen T-L, Louart B et al. (2018) Impact of quality bundle enforcement by a critical care pharmacist on patient outcomes and cost. Crit Cre Med. 46:199-207.
MacLaren R, Roberts RJ, Dzierba AL et al. (2021) Characterizing critical care pharmacy services across the United States. Crit Care Explor 2021.
Newsome AS, Murray B, Smith SE et al. (2021) Optimization of critical care pharmacy clinical services: A gap analysis approach. Am J Health-Syst Pharm. 78:2077-2085.
Real K, Bell S, Williams MV et al. (2020) Patient perceptions and real-time observations of bedside rounding team communication: The interprofessional teamwork innovation model (ITIM). Joint Commission J Qual Patient Saf. 46:400-409.
Rech MA, Gurnani PK, Peppard WJ et al. (2021) Pharmacist Avoidance or Reductions in Medical costs in CRITically ill adults: PHARM-CRIT) study. Crit Care Explor.
Seneviratne RE, Bradbury H, Bourne RS (2017) How do pharmacists develop into advanced level practitioners? Learning from the experiences of critical care pharmacists. Pharmacy. 5:38.
Sikora A, Ayyala D, Rech MA et al. (2022) Impact of pharmacists to improve patient care in the critically ill: A large multicenter analysis using meaningful metrics with the Medication Regimen Complexity (MRC-ICU) score. Crit Care Med. 50:1318-1328.
Smetana KS, Flannery AH, Gurnani PK et al. (2023) Pharmacist avoidance or reductions in medical costs in CRITically ill adults rounding with one SERVICE compared with two or more services: PHARM-CRIT-SERVICE. J Am Coll Clin Pharm. 1-8.
Vincent L, Brindley PG, Highfield J et al. (2019) Burnout syndrome in UK intensive care unit staff: Data from all three Burnout Syndrome domains and across professional groups, genders, and ages. J Intensive Care Soc. 20:363-369.
Webb AJ, Carver B, Rowe S et al. (2023) The use of electronic health record embedded MRC-ICU as a metric for critical care pharmacist workload. JAMIA Open. 6 (4): ooad101.




















