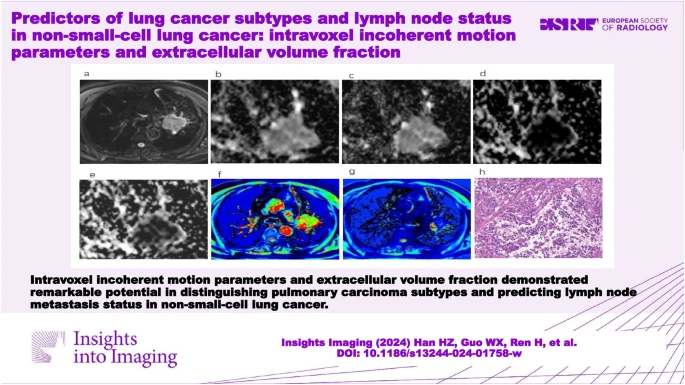
Lung cancer stands as one of the most formidable adversaries in the realm of oncology, being a leading cause of cancer-related deaths worldwide. Primarily classified into small-cell lung cancer (SCLC) and non-small-cell lung cancer (NSCLC), the latter accounts for approximately 85% of cases. NSCLC is further divided into adenocarcinoma (Adeno-Ca) and squamous cell carcinoma (SCC). While SCLC is highly invasive with a propensity for early metastasis, NSCLC's treatment depends significantly on factors like lymph node metastasis (LNM) and clinical staging. Accurate differentiation of lung cancer histologic types and precise LNM assessment are crucial for personalised treatment plans and improved prognosis. A recent study published in Insights into Imaging explored the performance of intravoxel incoherent motion (IVIM) parameters and the extracellular volume fraction (ECV) in distinguishing between different subtypes of lung cancer and predicting lymph node metastasis (LNM) status in patients with non-small-cell lung cancer (NSCLC).
IVIM and ECV in Lung Cancer Subtypes
Intravoxel incoherent motion (IVIM) and extracellular volume fraction (ECV) have emerged as promising tools for distinguishing lung cancer subtypes. IVIM provides insights into both diffusion and perfusion within tissues, effectively differentiating malignant from benign tumours and various pathological classifications. The true diffusion coefficient (D) from IVIM is particularly reliable, reflecting the extracellular space independent of microcirculation perfusion. ECV, calculated based on T1 values before and after contrast agent injection, indicates extracellular space proportions, offering insights into microvascular density and stromal fibrosis.
Research indicates that the ADC, D, and ECV values are significantly lower in SCLC compared to NSCLC, aligning with the high cellular density and restricted water diffusion in SCLC. The D value also distinguishes Adeno-Ca from SCC, reflecting differences in cellular structures. These parameters collectively offer a non-invasive approach to classify lung cancer subtypes, aiding in clinical decision-making.
Predicting Lymph Node Metastasis in NSCLC
Lymph node metastasis is a critical factor in the prognosis and treatment strategy for NSCLC patients. The presence of LNM is associated with elevated interstitial fluid pressure and hypoxia in primary lesions. ECV and perfusion fraction (f) values are higher in NSCLC patients with LNM, indicating increased microcirculation and extracellular space that facilitate metastatic spread.
In our study, ECV demonstrated superior diagnostic performance in predicting LNM status compared to the f value. This capability of ECV to assess lymphovascular stromal infiltration can guide preoperative interventions or postoperative treatments, improving patient outcomes. The high diagnostic accuracy of ECV and its ability to be less affected by variations in field strengths and acquisition techniques make it a valuable tool in clinical practice.
Study Design and Methodology
Our study, approved by the local institutional review board, prospectively enrolled 187 participants from September 2021 to October 2023. Inclusion criteria included CT findings indicative of lung cancer and no prior treatment. Exclusion criteria involved significant calcification or necrosis and poor imaging quality. All participants underwent MRI scans using a 3.0-T clinical magnetic resonance scanner, and histological evaluations were conducted within a week of the MRI scan.
The study aimed to clarify the role of IVIM parameters and ECV in differentiating lung cancer subtypes and predicting LNM status in NSCLC. MRI data processing involved extracting ADC, D, pseudo-diffusion coefficient (D*), and perfusion fraction (f) values. The findings demonstrated that ADC, D, and ECV values effectively distinguished SCLC from NSCLC, while the D value differentiated Adeno-Ca from SCC. ECV and f values were significant in predicting LNM status, with ECV showing higher diagnostic accuracy.
IVIM parameters and ECV offer a promising non-invasive approach to differentiate lung cancer subtypes and predict LNM status in NSCLC. These biomarkers provide clinicians with quantitative tools to promptly determine pathology types and identify high-risk cases of LNM, facilitating personalised treatment strategies. Future research should focus on larger sample sizes, standardised scanning parameters, and the inclusion of smaller lesions to further validate these findings and enhance the diagnostic capabilities of IVIM and ECV in lung cancer management.
The integration of IVIM parameters and ECV into clinical practice holds the potential to revolutionise lung cancer diagnosis and treatment, ultimately improving patient outcomes and prognosis.
Source: Insights into Imaging
Image Credit: iStock