Breast cancer is the most prevalent cancer and the leading cause of cancer-related deaths among women. Incidental breast lesions, found in 0.3% to 7.63% of cases during computed tomography (CT) scans, pose a clinical challenge as 31.0% to 70.0% of these lesions are malignant. Dual-energy CT (DECT) captures data at two energy levels, offering enhanced contrast and material differentiation, which is useful for tumour imaging and assessing breast lesions. DECT has been studied for various applications, including determining optimal energies for virtual monoenergetic images (VMIs), distinguishing benign from malignant lesions, evaluating lymph node and distant metastasis, and predicting immunohistochemical biomarkers.
DECT's routine use in clinical exams and its high tissue resolution make it potentially valuable for characterising multifocal breast lesions, potentially reducing the need for MRI. DECT could also help differentiate incidental lesions, decreasing unnecessary referrals. Previous studies indicate DECT parameters like iodine concentration, effective atomic number, and curve slope have diagnostic value in distinguishing lesion types. However, integrating clinical and imaging characteristics for differential diagnosis has not been explored.
This study hypothesises that combining DECT quantitative parameters with clinical and morphological features can effectively characterise benign and malignant breast lesions. The goal is to develop and validate a DECT-based model to aid in the further work-up of breast lesions detected on DECT.
A Prospective Study from July 2022 to July 2023
In a study conducted from July 2022 to July 2023, patients with suspected breast cancer undergoing chest dual-phase contrast-enhanced DECT scans before surgery were enrolled to evaluate mediastinal and axillary lymph nodes or underlying lung neoplasms. Inclusion criteria included BI-RADS 4A/4B/4C or 5 breast lesions detected by ultrasound or mammography, no prior chemotherapy or radiotherapy, and no history of iodine allergy or renal insufficiency. Exclusion criteria involved incomplete pathological information, invisible target lesions on DECT, and poor image quality due to severe metal artefacts. Eligible lesions were randomly divided into training and test cohorts at a 7:3 ratio.
Clinical and morphological characteristics from DECT images were collected, including age, family history, menopausal status, symptoms, lesion location, fibroglandular tissue (FGT), background parenchymal enhancement (BPE), lesion shape, margin, enhancement, inner enhancement, and maximum diameter. DECT morphological characteristics were evaluated by two radiologists and confirmed by a senior radiologist using MRI-BI-RADS lexicon criteria. Dense FGT and moderate/marked BPE were categorised based on specific criteria, and lesion shapes and margins were classified as regular or irregular and non-circumscribed, respectively.
Participants underwent chest contrast-enhanced DECT in the prone position. Iodinated contrast agent was administered, and scans were performed in arterial and venous phases. Radiation dose was recorded, and DECT images were reconstructed on a dedicated workstation. Quantitative parameters such as attenuation, iodine concentration (IC), effective atomic number (Zeff), and slope of the curve (λHU) were measured, normalised, and averaged over three slices.
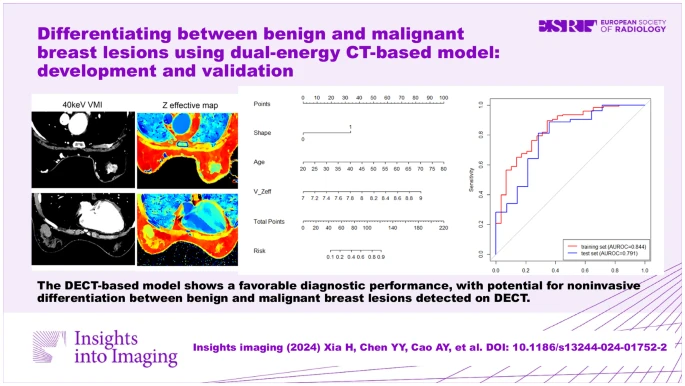
A DECT-based model was developed to differentiate benign and malignant breast lesions using significant parameters identified through univariate and multivariate logistic regression analyses. The model's performance was assessed using ROC curves, sensitivity, specificity, accuracy, Hosmer-Lemeshow test, calibration curves, and decision curve analysis, demonstrating its potential clinical utility in distinguishing between benign and malignant breast lesions detected on DECT.
Promising Diagnostic Performance in Differentiating Benign and Malignant Breast Lesions
The study enrolled 227 patients with suspected breast cancer, ultimately including 200 patients with 222 breast lesions after exclusions. Of these, 43 lesions were benign and 179 were malignant, as confirmed by pathology. There were no significant differences in clinical and DECT-derived morphological features between the training and test cohorts.
Key findings from univariate analysis in the training cohort indicated that malignant lesions were associated with older age, postmenopausal status, irregular shape, and non-circumscribed margins. DECT quantitative parameters such as attenuation, iodine concentration (IC), effective atomic number (Zeff), and the slope of the curve (λHU) were higher in malignant lesions compared to benign ones.
A DECT-based model was constructed using age, lesion shape, and Zeff in the venous phase as independent predictors. The model, visualised by a nomogram, showed strong diagnostic performance, with AUCs of 0.844 in the training cohort and 0.791 in the test cohort. Sensitivity, specificity, and accuracy were 89.7%, 65.5%, and 85.2% in the training cohort and 86.8%, 64.3%, and 82.1% in the test cohort. Calibration analysis showed good agreement between predicted probabilities and actual outcomes, and decision curve analysis indicated that the model provided enhanced net benefits over default strategies.
The DECT-based model demonstrated promising diagnostic performance in differentiating benign and malignant breast lesions, potentially aiding in clinical decision-making.
Clinical Implications and the Way Forward
Key findings indicated that malignant lesions were more likely to present in older, postmenopausal women, with irregular shapes and non-circumscribed margins. Venous phase DECT parameters were particularly effective in distinguishing lesion types, possibly due to better contrast agent penetration. The study highlighted the potential of DECT in reducing radiation exposure by focusing on venous phase scans.
The model's calibration and decision curve analysis confirmed its reliability and clinical utility. The study's limitations included a single-centre design, imbalance between benign and malignant cases, exclusion of some invisible lesions, and potential variability in radiologist interpretations. Future multicentre studies with balanced datasets and additional DECT parameters are recommended for further validation and enhancement of the model.
In conclusion, the DECT-based model integrating clinical, morphological, and quantitative parameters shows promise in identifying benign and malignant breast lesions, aiding radiologists in clinical decision-making.
Source: Insights into Imaging
Image Credit: iStock