Breast cancer treatment has advanced significantly over the years, with various methods being employed to improve patient outcomes. One such innovative method is ultrasound-guided cryoablation, which offers a safe, effective, and minimally invasive outpatient procedure to treat breast cancer. This procedure utilises extremely cold temperatures to induce tissue necrosis and cell death. A recent article published in AJR explores the benefits, efficacy, and implementation of cryoablation in treating breast cancer, particularly in patients who are considered poor surgical candidates due to comorbidities.
Benefits of Cryoablation Over Traditional Surgery
Cryoablation presents several advantages over traditional surgical methods for treating breast cancer. One of the most significant benefits is using local anaesthesia without the need for sedation or general anaesthesia. This feature alone makes the procedure less risky and more accessible, especially for patients who may not tolerate general anaesthesia well due to other health conditions. Additionally, cryoablation offers shorter recovery times, which translates to less downtime and quicker patient return to daily activities.
Cosmetic outcomes are another area where cryoablation excels. Traditional breast cancer surgery can often leave noticeable scars and result in significant changes to the breast's appearance. In contrast, cryoablation is less invasive, improving cosmetic outcomes and higher patient satisfaction. Moreover, the overall cost of cryoablation is generally lower than that of traditional surgery, making it a more economical option for both patients and healthcare providers.
Clinical Trials and Patient Selection
Prospective clinical trials, such as ACOSOG Z1072 and ICE3, have evaluated the procedural efficacy of cryoablation for breast cancer treatment. These trials have set strict inclusion criteria, focusing on patients with characteristics associated with favourable cryoablation responses. Typically, these criteria include female patients aged 50 and above, with early-stage, low-risk, unifocal invasive ductal carcinoma (IDC) measuring less than 1.5 cm. Other requirements include no extensive intraductal component, a low Ki-67 proliferation index, and positive hormone receptor status (ER+ and PR+, but HER2-). Additionally, the tumour must be well-visualized on ultrasound, located at least 0.5 cm from the skin, and at least 0.3 cm from the pectoralis muscle.
The trials have shown that cryoablation is a safe and efficacious alternative to surgery for breast cancer treatment in this restricted patient population. However, data on cryoablation for patients who do not meet these criteria remain limited. Therefore, it is essential to evaluate the safety and outcomes of cryoablation in patients with less favourable characteristics who are not eligible for these trials.
Implementation and Procedural Details
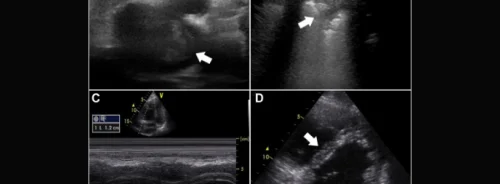
Implementing a breast cryoablation service requires careful planning and consideration of several factors. Cryoablation procedures are performed under ultrasound guidance in an outpatient setting, typically by a fellowship-trained radiologist. Various cryoablation devices are available, including those that use liquid nitrogen or high-pressure argon gas. The choice of device often depends on institutional availability, physician preference, and lesion characteristics.
During the procedure, the radiologist selects and places the cryoablation needle to ensure the entire targeted lesion is exposed to lethally cold temperatures. The process involves two freeze-thaw cycles, intending to create an ice ball that extends beyond all tumour margins. Adverse events are monitored and documented, with any occurring events classified according to the Common Terminology Criteria for Adverse Events (CTCAE).
Pre-ablation and post-ablation imaging protocols vary depending on the institution and proceduralist preferences. Patients typically undergo pre-ablation imaging via mammography and ultrasound, with some also receiving MRI. Follow-up imaging is critical to assess the procedural success and detect any recurrence. A biopsy is recommended for suspicious findings detected on follow-up imaging.
In conclusion, ultrasound-guided cryoablation represents a promising minimally invasive treatment option for breast cancer, offering numerous benefits over traditional surgery. It is particularly advantageous for patients who are poor surgical candidates due to comorbidities. Clinical trials have demonstrated the efficacy of cryoablation in a select patient population with favourable characteristics. However, expanding its use to a broader range of patients requires further research and evaluation.
Implementing a cryoablation service involves meticulous planning and adherence to procedural protocols to ensure safety and effectiveness. While the frequency of adverse events is low and technical success rates are high, ongoing monitoring and follow-up are essential to detect any recurrences early. Cryoablation's potential to provide good cosmetic outcomes, shorter recovery times, and lower costs make it an attractive alternative to traditional breast cancer surgery, particularly for those who seek less invasive treatment options. As the medical community continues to explore and refine this technique, cryoablation could become a standard option in the arsenal against breast cancer.
Source: AJR
Image Credit: iStock