Pulmonary embolism (PE) involves blockage of pulmonary arterial branches by a substance, usually a deep venous thrombus. It is a common and deadly cardiovascular condition, second only to heart attack and stroke. Since PE symptoms are often vague, clinical guidelines recommend using decision rules like the Wells or Revised Geneva score for initial patient assessment. In cases of low or intermediate probability, a normal D-dimer test can rule out PE, though its specificity decreases significantly with age and comorbidities, leading to many false positives. As a result, only about 20% of patients referred for imaging are diagnosed with PE. Meta-analyses suggest that using ultrasound (heart, lungs, lower extremities) can better select patients for imaging. Cardiac ultrasound can show right ventricular strain, lung ultrasound can reveal subpleural infarctions, and venous ultrasound can find thrombotic material. While single-organ ultrasound findings have high specificity but low sensitivity, a multi-organ approach increases overall sensitivity and has a high negative predictive value for low pre-test probability patients. Studies suggest this approach could reduce referrals for CT pulmonary angiography by about 50% without compromising safety. The PRIME study recently published in the Lancet aimed to evaluate whether using a tailored ultrasound protocol could reduce the need for diagnostic imaging in real-life settings, and measure the failure rate (missed PEs diagnosed within three months) and adverse events. The study aimed to improve patient selection for imaging and ensure safety.
Study Design and Objectives of the PRIME Trial
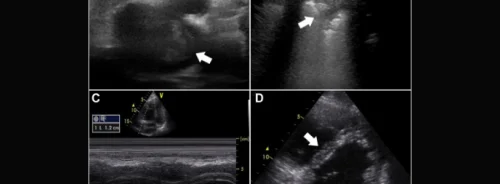
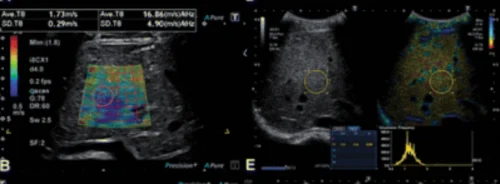
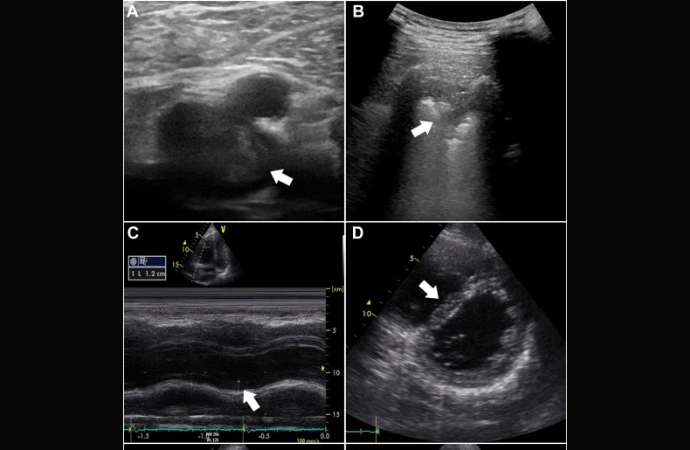
The PRIME study is an open-label multicentre randomised controlled trial conducted at six Danish hospitals. It started on June 18, 2021, and concluded recruitment on February 1, 2023. The trial included patients over 18 suspected of pulmonary embolism (PE), excluding those who were pregnant, hemodynamically unstable, had prior ultrasound, recent PE diagnosis, or mental disabilities. Participants were randomised to either a multiorgan ultrasound investigation or standard diagnostic imaging (CT pulmonary angiography or lung scintigraphy). In the ultrasound group, certified investigators performed cardiac, lung, and lower extremity venous ultrasounds following specific protocols to detect signs of PE. Based on the findings, patients were categorised into three groups: confirmed PE, dismissed PE suspicion, or uncertain PE requiring further imaging.The primary goal was to evaluate if the tailored ultrasound protocol could reduce referrals for diagnostic imaging while ensuring patient safety. Secondary outcomes were assessed three months post-inclusion through a review of electronic patient records. The study aimed to improve patient selection for imaging and monitor the incidence of missed PEs and adverse events.
Enrollment, Outcomes, and Cost-Effectiveness of the PRIME Trial
From June 18, 2021, to February 1, 2023, the PRIME trial assessed 218 patients for eligibility and enrolled 150. Seventy-three patients were assigned to ultrasound investigation, and 77 to usual diagnostic imaging, with no exclusions or dropouts. Both groups had similar baseline characteristics, with a median age of 68 years and common symptoms of dyspnoea (79.3%) and chest pain (44.7%). In the ultrasound group, PE suspicion was dismissed in 30 patients, confirmed in 11, and 32 required further diagnostic imaging. In the control group, 75 of 77 patients underwent CT pulmonary angiography or lung scintigraphy. The ultrasound group saw a 45.2% reduction in referrals for diagnostic imaging. PE was diagnosed in 31.5% of the ultrasound group and 33.8% of the control group at enrollment. The ultrasound group had a 4.0% failure rate for detecting PE during the 3-month follow-up. Adverse events were higher in the ultrasound group (43.8%) compared to the control group (22.6%), though bleeding complications were rare in both groups. Nine patients in the ultrasound group and six in the control group died during the follow-up, with no deaths due to missed PE. The reduction in diagnostic imaging referrals led to an estimated savings of €156.6 per patient, with no additional costs for the ultrasound procedure. Overall, the study supports the feasibility and cost-effectiveness of using ultrasound to reduce unnecessary diagnostic imaging in suspected PE cases.
Significant Reduction in Imaging Referrals with High Failure Rate
This study is the first randomised pragmatic trial to evaluate the use of ultrasound in confirming or dismissing the suspicion of pulmonary embolism (PE). The findings indicate that incorporating multiorgan ultrasound in the diagnostic work-up of suspected PE can significantly reduce referrals for diagnostic imaging. However, the study's associated failure rate is considered unacceptably high, necessitating further studies with adequate power to assess safety or modifications to improve sensitivity. Previous studies, such as the YEARS and PEGeD studies, also aimed to reduce unnecessary diagnostic imaging in PE diagnostics, achieving reductions with lower failure rates compared to this study. In the current study, ultrasound led to a 45.2% reduction in diagnostic imaging referrals but had a higher 3-month failure rate of 4.0% overall and 6.7% for patients dismissed by ultrasound alone.
Ensuring Safety and Reliability in Ultrasound Use for Pulmonary Embolism
The study highlights several limitations, including the need for integrating D-dimer levels as a safety threshold, the potential for selection bias due to slow patient recruitment, and the variability in ultrasound interpretation among physicians. It also notes the importance of adequate training and competency assessment for ultrasound use. Future studies should focus on low-probability patients to enhance the negative predictive value of ultrasound findings. Additionally, limiting D-dimer levels and ensuring rigorous competency standards for ultrasound operators are recommended. The study concludes that while ultrasound can reduce diagnostic imaging referrals, more research is needed to ensure its safety and reliability before clinical implementation.
Source & Image Credit: The Lancet