Osteoporosis is a prevalent condition characterised by reduced bone density and increased fracture risk. With the ageing global population, the incidence of osteoporotic fractures is expected to rise significantly. Early detection and accurate fracture risk prediction in osteoporosis patients are crucial for preventing debilitating outcomes and reducing healthcare costs. A recent study published in Academic Radiology explores the diagnostic accuracy of Dual-Energy CT (DECT) in predicting osteoporosis-associated fractures compared to other commonly used metrics such as Hounsfield Unit (HU)-based values and cortical thickness ratio. The study demonstrates the superior predictive value of DECT-based bone mineral density (BMD) measurements over traditional methods.
DECT-Based BMD Assessment
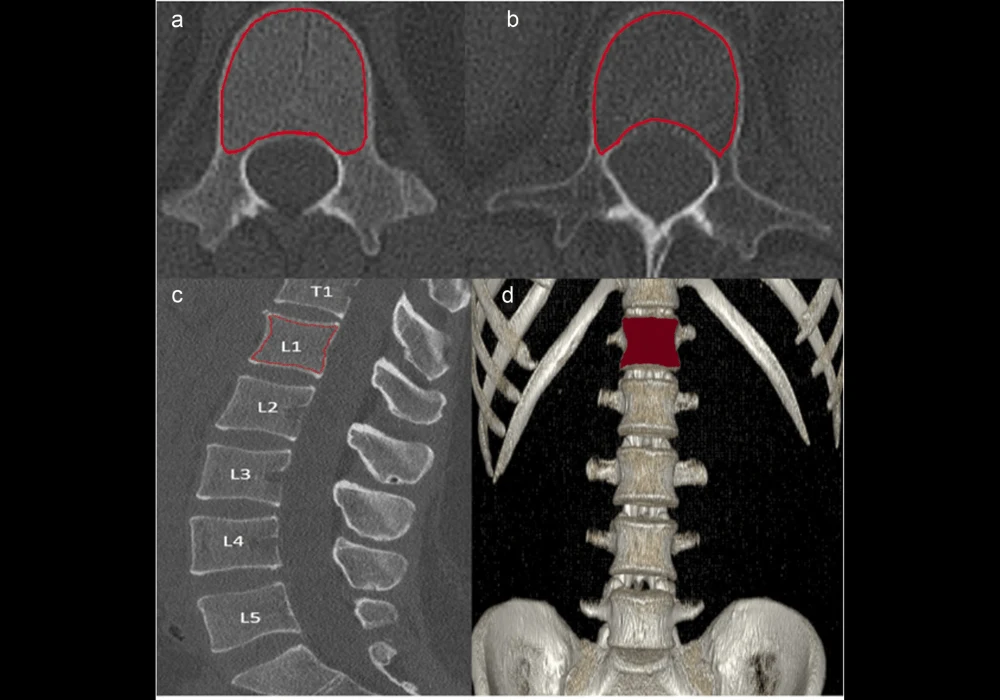
Dual-Energy CT (DECT) has emerged as a powerful imaging modality capable of assessing bone quality without the need for calibration phantoms. Unlike traditional CT, which relies on Hounsfield Units (HU) to measure bone density, DECT provides volumetric BMD assessments by differentiating materials within the bone structure. This method allows for more accurate and comprehensive evaluations of bone quality, making it particularly useful in predicting osteoporotic fractures.
This study compared DECT-based BMD assessments with traditional metrics such as trabecular HU, cortical HU, and cortical thickness ratio in predicting the 2-year risk of osteoporosis-associated fractures. The findings revealed that DECT-derived BMD outperformed HU-based metrics and cortical thickness ratio in diagnostic accuracy, with a significantly higher area under the curve (AUC) in receiver operating characteristic (ROC) and precision-recall (PR) curve analyses.
Comparative Analysis of Bone Quality Metrics
The study highlights the limitations of traditional bone quality assessment methods, such as HU-based measurements and cortical thickness ratio. While widely used, HU-based assessments are subject to inaccuracies due to factors such as variations in body composition, overlying tissue distortion, and changes in scan resolution. These limitations often lead to underestimation of bone density and reduced diagnostic accuracy.
Cortical thickness ratio, another commonly used metric, is also influenced by various factors such as age, sex, and dietary habits. This variability can result in inconsistent and unreliable predictions of fracture risk. In contrast, DECT-based BMD assessments provide a more reliable and accurate measure of bone quality, as demonstrated by the study's findings.
The study's ROC and PR curve analyses showed that DECT-based BMD had the highest sensitivity and specificity for predicting osteoporotic fractures, with an AUC of 0.95 for the ROC curve and 0.96 for the PR curve. In comparison, the AUCs for trabecular HU, cortical HU, and cortical thickness ratio were significantly lower, indicating their reduced effectiveness in predicting fracture risk.
Clinical Implications of DECT-Based BMD
The superior diagnostic performance of DECT-based BMD assessments has significant implications for clinical practice. Early and accurate prediction of osteoporotic fractures is essential for implementing timely interventions, such as pharmacological treatments and lifestyle modifications, to prevent fractures and reduce healthcare costs. DECT-based BMD assessments offer a promising tool for clinicians to identify patients at high risk of fractures and tailor treatment plans accordingly.
However, the widespread adoption of DECT in clinical practice is currently limited by the high cost and limited availability of DECT scanners. As a result, DECT-based BMD assessments are primarily used in specialised clinics, and more affordable and accessible alternatives are needed to ensure broader implementation. Future research should focus on developing cost-effective DECT technologies and exploring the integration of DECT-based BMD assessments into routine clinical workflows.
Conclusion
In conclusion, DECT-based BMD assessments offer a superior method for predicting osteoporosis-associated fractures compared to traditional HU-based metrics and cortical thickness ratio. The study's findings underscore the importance of incorporating DECT into clinical practice for early detection and accurate fracture risk prediction in osteoporosis patients. While challenges remain in terms of cost and accessibility, the potential benefits of DECT-based BMD assessments in improving patient outcomes and reducing healthcare costs make it a valuable tool in the fight against osteoporosis.
As healthcare systems continue to grapple with the rising burden of osteoporosis, the adoption of advanced imaging technologies like DECT could play a pivotal role in enhancing diagnostic accuracy and preventing fractures. Future research and technological advancements will be key to making DECT more widely available and further improving its clinical utility in osteoporosis management.
Source & Image Credit: Academic Radiology