Health authorities in the UK are developing regional initiatives to make significant improvement to health and care. The needs look beyond departmental and organizational boundaries, focusing on the needs of the local population.[1] (These initiatives are called STPs, sustainability and transformational plans). In this article, Chris Scarisbrick, Sectra UK and Ireland, looks at how diagnostic imaging IT can accelerate these plans. Silo-busting and integrated diagnostics is on the near-future horizon, and population based health fueled by machine learning/AI is a real possibility if the opportunity is seized to create regionalized diagnostic functions.
Regionalised approaches to health and social care are beginning to take hold across the country. Health devolution in Greater Manchester has been one highly prominent example, where the much publicised ‘Devo Manc’ will involve £6bn of devolved funding for regional management of health and social care services. But this is just the beginning. Regionalised health and care will rapidly become commonplace in the near future, with the implementation of sustainability and transformation plans, and the creation of integrated care organisations.
But as the shift to better co-ordination of services starts to sweep across the land, a crucial question remains: has sufficient thought been given to the role that imaging and diagnostic disciplines can play in joined-up and regional working?
Don’t miss the opportunity to regionalise diagnostics
The NHS (National Health Services, the publicly funded national healthcare system for England and one of the four National Health Services of the United Kingdom) in England could now be faced with a greater opportunity than ever before to modernise diagnostics and break down barriers for the ‘ologies’. Diagnostic departments play a crucial role as one of the earliest points in determining the needs of a patient, and the actions that must be taken to remedy illness and support wellbeing.
But still today, diagnostic departments suffer from silos of information just as much as any other part of the health and care set up, with some, such as pathology, only at the beginning of their journey of embracing digital information.
We have had some national direction to consolidate pathology services as part of the STP process, in an echo of recommendations set out previously by Lord Carter. But at a time when diagnostic resources are stretched more than they have ever been, this is just the tip of the iceberg in what can be achieved.
Questions must be how to make the opportunity much more than about cost savings for pathology, where diagnostics is seen as part of a back-office reorganisation, and how we can use consolidation and regionalisation as a means for diagnsostic services to work together around the needs of the patient and better tailor treatement decisions.
Silo-busting in the hospital so that we can treat human beings
There is now an unprecedented chance to break down silos for diagnostic disciplines, whilst also still retaining specialist departmental services, across the healthcare enterprise, so that we can make the most of imaging for patient care and even unearth a goldmine of data for better patient outcomes.
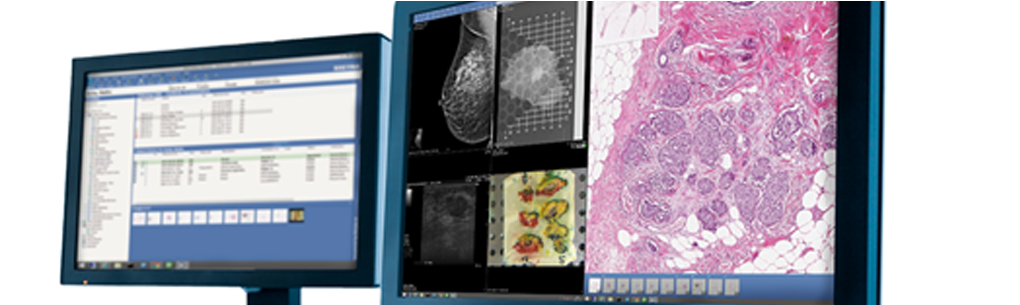
We have an opportunity to enable every diagnostic discipline, from radiology to pathology, dermatology, breast, and more, to work more closely than ever before and to make the most of the information they capture.
The technology now exists to make this possible. Hospitals in other parts of the world are already making information and image sharing between diagnostic disciplines and the wider hospital enterprise possible by starting to exploit technologies such as the vendor neutral archive (VNA), or by making their picture archiving and communication system (PACS) about more than radiology.
Some PACS vendors have anticipated the shift towards enterprise imaging and have developed support for all kinds of multimedia formats outside of the traditional DICOM space. Many NHS hospitals have made significant investments in their radiology PACS solutions, in many cases these investments can be leveraged to provide first class workflows to departments that have traditionally developed solutions outside of radiology.
The VNA is also often simply used as a data storage facility in the NHS, but can offer so much more potential to allow interrogation of imaging from any ology in any part of the hospital.
Linking information from the VNA or PACS back to the electronic patient record (EPR) can alert frontline clinical staff to important diagnostic information, but equally importantly, providing different diagnostic disciplines and multi-disciplinary teams (MDTs) with access to the full range of diagnostic imaging, can mean a substantial difference to making informed clinical decisions and diagnoses.
And if we can establish a bi-directional link with an EPR, so that diagnostic MDTs have access to all ancillary information from across the enterprise, then decisions can be made on the diagnosis of a patient and on personalised remedial steps, such as whether to operate on a cancer, based on an understanding of social factors, their lifestyle, and more.
This is about understanding and treating human beings, not just illnesses, and engaging in real silo-busting to place the patient at the centre of the diagnostic experience. We must move away from making patients go to multiple departments on different days of the week, when they are managed at the departmental level. If you can bring scheduling up a level, for example, you can see a holistic overview of the patient’s pathway and schedule all their appointments across the diagnostic chain for a single day. For a frail or elderly patient, or for someone who has a busy working and family life, avoiding potentially dozens of trips to hospital can be very significant.
Breaking down silos also offers the chance to remove costly IT managerial lines and processes. As pathology starts to embrace digitisation at scale, there are opportunities for sharing infrastructure and expertise with radiology, a discipline that digitised some 15 years ago.
But the future is not for any diagnostic department to hold the reigns of IT infrastructure. Integrated diagnostics will rely on the burden of IT management and infrastructure being removed to an enterprise level. There is no need to replicate IT provider management in individual departments along with all the associated costs and integration complications.
Blurring beyond the single hospital – taking diagnostics to the regional level
For any hospital the question of whether to engage in ‘silo-busting’ should almost be a no-brainer, given the above advantages for better and more affordable ways of working. But tapping into regionalisation can expand these benefits for patients and for cost savings across the health economy, whilst also providing new foundations to support the shift to population health.
There is now an opportunity to use the restructuring of health and care services to relaunch the diagnostic landscape, so that diagnostic departmental boundaries are broken down not just in the hospital but across entire healthcare regions.
Economies of scale can be exploited to maximum gain in this way. For diagnostics, resources are diminishing particularly rapidly, with fewer and fewer specialists, reduced funding and challenges in recruitment. We need to make the most of specialist expertise, and to draw on technology in a way that can support workflows around the patient and around being able to remotely share the reach of specialist expertise across a region.
Regions can also no longer afford to continue to procure multiple instances of the same technologies and to replicate management structures, when there is an opportunity to create a regional solution. This is not about the needs of any one hospital, any one department, or any one professional who shouts out ‘it’s better for me to have X solution’. We do need to make sure functionality of technology responds to real workflow, but organisational centric views cannot be allowed to lead the NHS, particularly as organisational identities are beginning to blur. We must look at the bigger picture.
We now have a chance to start to create regional diagnostic hubs, that allow digital imaging to flow where it is needed to make the best use of scarce resources, and to follow the individual, so that timely and better decisions can be made for and with patients.
And in the shift to population based approaches to health, regionalised diagnostic functions can lead to the creation of a vast source of imaging data that can flow between systems, with the potential to provide powerful sources for big data analysis, and for machine learning where artificial intelligence can flag up patients at risk of serious conditions.
Changing business models and new models of care that are emerging from STPs, offer a chance to change the very nature of how diagnostics are run for the better. There is no better time for the NHS to seize this opportunity.







