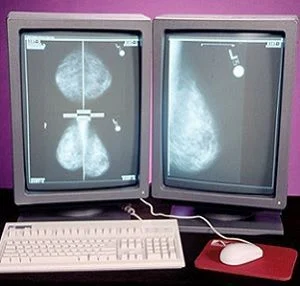
Computer-aided detection (CAD) in screening mammography is supposed to help radiologists identify subtle cancers that might otherwise be missed. However, analysis of results from a large Breast Cancer Surveillance Consortium database of digital screening mammograms revealed that CAD was not associated with improved diagnostic accuracy. The study is published online in JAMA Internal Medicine.
"CAD is a technology that does not seem to warrant added compensation beyond coverage of the mammographic examination. The results of our comprehensive study lend no support for continued reimbursement for CAD as a method to increase mammography performance or improve patient outcomes,” write Constance D. Lehman, MD, PhD, of the Massachusetts General Hospital, Boston, and co-authors. The U.S. Food and Drug Administration approved CAD for mammography in 1998 and the Centers for Medicare and Medicaid Services (CMS) increased reimbursement for CAD in 2002.
The researchers measured the performance of digital screening mammography with and without CAD in U.S. community practice. The researchers included more than 625,000 mammograms interpreted by 271 radiologists with CAD (n=495,818) or without (n=129,807) from 2003 through 2009 among 323,973 women. Linkages with tumour registries identified 3,159 breast cancers in the 323,973 women within one year of the screening.
The researchers found that screening performance with CAD was not associated with improvement based on the metrics they assessed:
Moreover, in subset analyses among 107 radiologists who interpreted mammograms both with and without CAD, performance was not improved with CAD and CAD was associated with decreased sensitivity (missing breast cancers).
 Commenting on the findings, Joshua J. Fenton (pictured), MD, MPH, of the University of California, Davis Health System, Sacramento, told HealthManagement.org: "CAD attempts to address a real problem: the imperfect sensitivity of screening mammography for breast cancer. But it simply doesn't achieve this goal in actual practice...The lesson of CAD is that we need large, real world evaluations of new screening technologies before we adopt them widely."
Commenting on the findings, Joshua J. Fenton (pictured), MD, MPH, of the University of California, Davis Health System, Sacramento, told HealthManagement.org: "CAD attempts to address a real problem: the imperfect sensitivity of screening mammography for breast cancer. But it simply doesn't achieve this goal in actual practice...The lesson of CAD is that we need large, real world evaluations of new screening technologies before we adopt them widely."
He is in agreement with the study authors' conclusion that insurers pay more for CAD with no established benefit to women. "Since it [CAD] apparently yields no clinical benefit, payers, including the U.S. Medicare programme, should stop paying for CAD use," Dr. Fenton said.
In a related commentary published in JAMA, Dr. Fenton who also has published several research articles about the merits of CAD, said any potential positive effects of CAD may be undetectable in the context of digital mammography, which may improve the radiologist’s interpretation regardless of CAD. "It is also conceivable that improvements in digital mammography technology have swamped any incremental impacts of CAD on interpretation that may have been previously detectable," he wrote.
Claire Pillar, Managing Editor, HealthManagement.org
Source: JAMA; Interview
Image credit: UC Davis; Flickr.com
"CAD is a technology that does not seem to warrant added compensation beyond coverage of the mammographic examination. The results of our comprehensive study lend no support for continued reimbursement for CAD as a method to increase mammography performance or improve patient outcomes,” write Constance D. Lehman, MD, PhD, of the Massachusetts General Hospital, Boston, and co-authors. The U.S. Food and Drug Administration approved CAD for mammography in 1998 and the Centers for Medicare and Medicaid Services (CMS) increased reimbursement for CAD in 2002.
The researchers measured the performance of digital screening mammography with and without CAD in U.S. community practice. The researchers included more than 625,000 mammograms interpreted by 271 radiologists with CAD (n=495,818) or without (n=129,807) from 2003 through 2009 among 323,973 women. Linkages with tumour registries identified 3,159 breast cancers in the 323,973 women within one year of the screening.
The researchers found that screening performance with CAD was not associated with improvement based on the metrics they assessed:
- Sensitivity was 85.3 percent with CAD and 87.3 percent without CAD
- Specificity was 91.6 percent with CAD and 91.4 percent without CAD
- Overall cancer detection rate (4.1 cancers per 1,000 women screened with and without CAD) or in the invasive cancer detection rate (2.9 vs. 3.0 cancers per 1,000 women screened with CAD or without)
Moreover, in subset analyses among 107 radiologists who interpreted mammograms both with and without CAD, performance was not improved with CAD and CAD was associated with decreased sensitivity (missing breast cancers).
 Commenting on the findings, Joshua J. Fenton (pictured), MD, MPH, of the University of California, Davis Health System, Sacramento, told HealthManagement.org: "CAD attempts to address a real problem: the imperfect sensitivity of screening mammography for breast cancer. But it simply doesn't achieve this goal in actual practice...The lesson of CAD is that we need large, real world evaluations of new screening technologies before we adopt them widely."
Commenting on the findings, Joshua J. Fenton (pictured), MD, MPH, of the University of California, Davis Health System, Sacramento, told HealthManagement.org: "CAD attempts to address a real problem: the imperfect sensitivity of screening mammography for breast cancer. But it simply doesn't achieve this goal in actual practice...The lesson of CAD is that we need large, real world evaluations of new screening technologies before we adopt them widely."He is in agreement with the study authors' conclusion that insurers pay more for CAD with no established benefit to women. "Since it [CAD] apparently yields no clinical benefit, payers, including the U.S. Medicare programme, should stop paying for CAD use," Dr. Fenton said.
In a related commentary published in JAMA, Dr. Fenton who also has published several research articles about the merits of CAD, said any potential positive effects of CAD may be undetectable in the context of digital mammography, which may improve the radiologist’s interpretation regardless of CAD. "It is also conceivable that improvements in digital mammography technology have swamped any incremental impacts of CAD on interpretation that may have been previously detectable," he wrote.
Claire Pillar, Managing Editor, HealthManagement.org
Source: JAMA; Interview
Image credit: UC Davis; Flickr.com
References:
Lehman CD et al. (2015) Diagnostic Accuracy of Digital Screening Mammography With and Without Computer-Aided Detection. JAMA Intern Med.
Published online September 28, 2015. doi:
10.1001/jamainternmed.2015.5231
Fenton JJ (2015) Is It Time to Stop Paying for Computer-Aided Mammography? JAMA Intern Med. Published online September 28, 2015. doi: 10.1001/jamainternmed.2015.5319
Fenton JJ (2015) Is It Time to Stop Paying for Computer-Aided Mammography? JAMA Intern Med. Published online September 28, 2015. doi: 10.1001/jamainternmed.2015.5319
Latest Articles
healthmanagement, computer-aided diagnosis, CAD, digital mammography, breast cancer, Medicaid
Computer-aided detection (CAD) in screening mammography is supposed to help radiologists identify subtle cancers that might otherwise be missed. However, analysis of results from a large Breast Cancer Surveillance Consortium database of digital screening