A line is often drawn between radiologists and clinicians. Several articles published recently touch upon the concept that there should be a distinction between radiologists and clinicians thus implying that radiologists are nonclinicians.
While there may be some truth to this, the fact is that passing on such a broad statement as to classify radiologists as nonclinicians is actually a grave injustice to professionals in this area who work very hard and make vital contributions to patients.
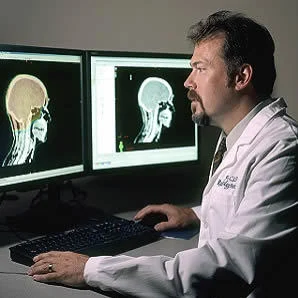
In medical usage, the term clinician distinguishes patient-care specialists from physicians who focus on education, research and administrative work. All clinicians, in some form or the other, have direct contact with patients and all of them have direct responsibility for patient care. But it is unfair to say that radiologists are not clinicians because every time they wield an ultrasound
transducer, produce a radiology report, or consult with a colleague
about a patient’s case, they are in fact, functioning as clinicians and hold direct responsibility for patient care.
Surprisingly, there is conflict about the clinician status even among radiologists. Interventional cardiologists believe that diagnostic radiologists are nonclinicians since they do not have outpatient clinics, do not hold admitting privileges at hospitals and do not routinely prescribe medications. Their role is thus different from real clinicians or so they propose. It is true that diagnostic radiologists are generally not a patient's first point of contact and are not immersed in a patient's electronic medical record. But they do work in another system and do contribute. Therefore, it is still not accurate to label them nonclinicians.
A case-study should highlight the important role a radiologist can play in a patient's care. This particular case actually suggests that not only do radiologists deserve to be accepted as clinicians but may as well be at the head of the clinician pack.
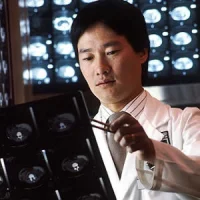
A musculoskeletal
radiologist performed a sonographic examination of a young man for
shoulder pain. The radiologist was aware that there was a low probability of a rotator cuff but he still went ahead and evaluated each of the tendons. However, the patient did not feel that the examination provided any explanation for his pain. The radiologist explained that there were limitations of the examination and while talking to the patient, he discovered that the patient had experienced a succession of injuries. By building rapport with the patient, the radiologist further discovered that the patient had suffered a twisting injury to his foot two months ago that had left him with persistent pain and disability. The patient showed him a selfie he had taken of the foot on the day after the incident.
By looking at the selfie, the radiologist was able to identify a classic case of Lisfranc injury and urged the patient to get another set of radiographs and to consult an orthopaedic surgeon immediately. The patient hesitated since his was a worker's compensation case and he could not afford to seek treatment without consulting his case worker. The patient did not think he could get approval within a month. In such a scenario, the radiologist could have simply said that a clinician could deal with it but he did not. He remained by the patient's side and decided to take matters into his own hands. He asked the patient to call his case worker and then when he realised the patient was not able to convince her, took the phone and provided the case worker a detailed description of the patient's injury and the possible consequences if not treated immediately. The case worker's attitude changed and she scheduled an appointment with an orthopaedic surgeon for the next day. Further evaluation revealed a missed Lisfranc fracture-dislocation and the patient had to undergo surgical reduction and fusion.
To this day, there is no written record of the radiologist's contribution in this case. On the outside, the radiologist appears to have functioned as a nonclinican but in reality, it was his diagnosis and his efforts that helped the patient get the care he needed.
Harry Mellins says it perfectly: "The
diagnostic radiologist is a clinician who has sacrificed one of the
greatest glories of the practice of medicine and its greatest
responsibility—daily contact with the ill and their families—in order to
concentrate more on the essence of our profession, the pathology of the
living. This he sees through the medium of shadows, which has left
him open to the charge of not quite being a real clinician. But shadows,
after all, are real. What are we to one another and what is the world
to any of us but an inverted image on the retina? Seeing is done with
the mind.…The radiologist perceives the shadow, sees the lesion, and
imagines the man. The bedside physician sees the man, perceives the
signs, and imagines the lesion. They practice from the outside in and we
from the inside out. But both are clinicians, for in truth there is no
other kind of doctor worthy of the name."
Source: Journal of the American College of Radiology
Image Credit: Wikimedia Commons