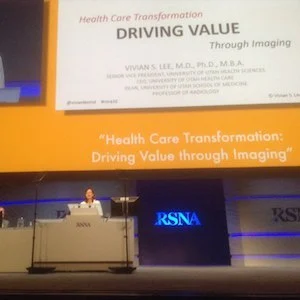
Radiologists can and should drive value-based healthcare, and they have a significant role to play in the path to transforming healthcare to a value basis, says Vivian Lee, MD, PhD, CEO of University of Utah Healthcare.
Lee shared the University of Utah health system's journey towards value-based healthcare with delegates to the Radiological Society of North America (RSNA) annual scientific meeting in Chicago last week, presenting the meeting's annual oration in diagnostic radiology. Lee, a radiologist, also serves as Professor of Radiology, Senior Vice-President for Health Sciences and Dean of the School of Medicine, University of Utah School of Medicine.
See Also: Improving Diagnosis Is Urgent: Multidisciplinary Effort Required
Put simply, value is quality and service delivered at a reasonable cost, said Lee. Quality refers to patient outcome and service is the patient experience. These two need to be delivered at a reasonable cost. At Utah the transformation to value has been a virtuous cycle, as they are no. 1 in the U.S. for quality
Improved Patient Satisfaction
Lee noted that her predecessor as CEO, Lorris Betz, put it well, “Medical care can only be truly great if the patient thinks it is.†On patient satisfaction they asked patients to score satisfaction with communication, decision-making, engagement and respect. With this they could benchmark physicians against national data. They post data online on their providers, and ratings improved such that there was a consistently higher score for all healthcare providers (Lee et al. 2016).
Improving Quality and Analysing Costs
Working on the quality/cost ratio was harder, as they had to build the data tools themselves. The project was analysed in a recent article in JAMA (Lee et al. 2016b). Despite healthcare having the problem of high cost, it is the only industry that does not know the costs of providing services - no wonder costs continue to grow out of control, said Lee. At Utah they set out to cost every element of care in their delivery system. As a result, they can map it to any healthcare provider, any patient or any ICD code. This also allows them to see outliers by provider and any inconsistent processes. Armed with this information, staff, many of whom are trained in the Lean process, can map out processes, identify inconsistencies and work towards improving quality.
Role of Radiologists
Lee observed that the most important attributes of radiology are clarity, utility and timeliness. The paradox remains that while imaging is regarded as the most impactful health advance of the 20th century, many of the Choosing Wisely recommendations are against imaging, and none favoured imaging over another approach. The radiology job market is diminishing, as question are raised about the value of the role. The lowest hanging fruit is improving reporting. However, radiologists need to create the same feedback loop across all referring physicians to ensure that they learn and continually improve, urged Lee. At Utah they ask referring physicians to score the usefulness of the imaging study and the radiology report for patient care. For the most part the study value is ranked high, and the report value a little bit lower. Where value is added is in improving diagnostic confidence, and in improving value for the customer. Breast imaging leads the way in patient-centred care, observed Lee. For example offering online scheduling for mammography exams increases patient access. The one-stop clinic that offers mammography, tomosynthesis and same day biopsy reduces the time to reporting and time to diagnosis. For radiology departments the challenge is to reduce the costs of imaging and analyse processes to improve efficiency without sacrificing quality. At Utah, they found that 80 percent of the cost of a CT scan is labour, predominantly the costs of interpretation. It may be possible to reduce costs by using lower cost personnel when applicable and also to use clinical decision support (CDS) systems. Lee questioned if there was a role for radiological assistants, and if so, would it not be better if radiologists supervise them rather than others in the health system?
Diagnostic errors need to be avoided and diagnosis needs to be improved. With improved diagnostics, it will be possible to find the patients who can really benefit from particular therapies, said Lee. Imaging can be used to assess the value of new tests, drugs and devices and it should be integrated into better clinical diagnosis and decisions. As a value-driven profession, radiologists can own responsibility for accurate and timely diagnoses to drive value.
Claire Pillar
Editorial Director
HealthManagement
References:
Lee VS, Miller T, Daniels C, Paine M, Gresh B, Betz AL (2016a) Creating
the exceptional patient experience in one academic health system. Acad
Med, 91(3): 338-44.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4885533/
Lee VS, Kawamoto K, Hess R, Park C, Young J, Hunter C, Johnson S, Gulbransen S, Pelt CE, Horton DJ, Graves KK, Greene TH, Anzai Y, Pendleton RC (2016b) Implementation of a value-driven outcomes program to identify high variability in clinical costs and outcomes and association with reduced cost and improved quality. JAMA, 316(10): 1061-72.
Lee VS, Kawamoto K, Hess R, Park C, Young J, Hunter C, Johnson S, Gulbransen S, Pelt CE, Horton DJ, Graves KK, Greene TH, Anzai Y, Pendleton RC (2016b) Implementation of a value-driven outcomes program to identify high variability in clinical costs and outcomes and association with reduced cost and improved quality. JAMA, 316(10): 1061-72.
Latest Articles
#RSNA16, RSNA 2016, Radiologists, Value-Based Healthcare
Radiologists can and should drive value-based healthcare, and they have a significant role to play in the path to transforming healthcare to a value basis, says Vivian Lee, MD, PhD, CEO of University of Utah Healthcare.