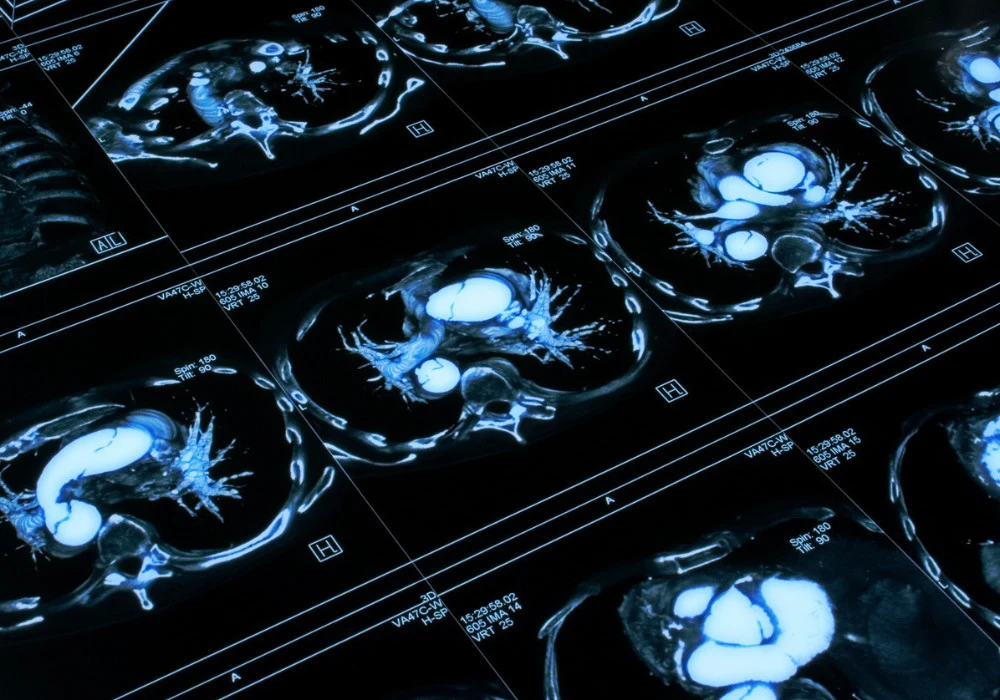
Low-dose CT has become the cornerstone of lung cancer screening programmes, enabling early detection and reducing mortality. It is widely integrated into clinical practice and endorsed by international guidelines. However, repeated exposure to ionising radiation through regular follow-up CT scans raises concerns, especially for screening populations and younger patients. Pulmonary MRI has emerged as a radiation-free alternative, but its uptake has been hindered by motion artefacts, longer scan times and reduced image quality in challenging anatomical areas.
Recent advancements in MRI acquisition and reconstruction, including parallel imaging, compressed sensing and deep learning, have renewed interest in MRI-based lung imaging. An accelerated 3D gradient echo sequence using AI-enhanced reconstruction has now been assessed for its ability to detect pulmonary nodules and assign Lung-RADS classifications, offering a potential substitute for CT.
Performance of AI-Enhanced MRI
The AI-enhanced 3D gradient echo MRI sequence was evaluated in a prospective clinical trial involving 75 patients with a total of 135 lung nodules. MRI scans were performed within one week of a reference low-dose CT, and three radiologists assessed nodule presence, size, morphology and Lung-RADS classification independently. The MRI sequence demonstrated a detection rate of 96.3%, missing only five nodules across all readers. The missed nodules were small—typically under 6 mm—and located in areas prone to motion artefacts or adjacent to structures such as the mediastinum or pleura. Despite these exceptions, the MRI sequence captured a wide range of nodule types, including solid, part-solid, ground-glass and calcified lesions. Morphological assessment showed strong agreement with CT across all readers.
Quantitative analysis further confirmed the robustness of the MRI protocol. Nodule size measurements on MRI closely matched those on CT, with average deviations of less than 0.3 mm per reader. Inter-rater and intra-rater reliability for both modalities were excellent. The MRI sequence achieved this high accuracy with a nominal scan time of under four minutes, using isotropic voxels and respiratory gating. This balance between speed and resolution positions the technique as a viable alternative in clinical workflows where both diagnostic confidence and patient throughput are critical.
Must Read: Refining Nodule Management in Lung Cancer Screening
Agreement in Risk Stratification
Lung-RADS classification is central to lung cancer screening, guiding clinical decision-making based on nodule characteristics. The AI-enhanced MRI sequence demonstrated substantial to near-perfect agreement with CT in Lung-RADS categorisation. For two of the three radiologists, agreement between MRI and CT reached almost perfect levels, while the third achieved substantial concordance. Inter-rater agreement was also high within each modality. Classification discrepancies between CT and MRI occurred in 14.2% of cases on average, with 4.9% resulting in changes that could alter clinical management. These critical changes included both upgrades and downgrades across key thresholds such as Lung-RADS 4A, 4B and 4X.
The changes were not uniformly distributed. Most were associated with the least experienced reader, suggesting that reader expertise plays a significant role in maintaining classification consistency. Review of the discrepant cases revealed that differences in perception of ground-glass components and small size variations near threshold values contributed to some of the misclassifications. While the number of critical changes was relatively low, they underline the importance of consistency in Lung-RADS assignment, particularly when using newer imaging modalities. Targeted training or integration of decision support tools could help standardise interpretation and mitigate these discrepancies.
Clinical Feasibility and Future Directions
The evaluated MRI sequence offers several practical advantages. Unlike ultrashort echo time (UTE) or zero echo time (ZTE) sequences, which often require specialised equipment and longer acquisition times, the AI-enhanced Cartesian protocol is compatible with standard MRI systems. The combination of compressed sensing, parallel imaging and deep learning reconstruction, branded as SmartSpeed, is deployable on existing hardware equipped with GPU capability. This enables broader implementation without extensive infrastructure upgrades.
Despite the overall strong performance, motion artefacts remain a challenge, particularly for smaller or subsolid nodules located near the pleura or central airways. In several missed cases, patient movement during acquisition contributed to reduced image quality. Emerging techniques such as real-time motion correction, retrospective AI-based correction algorithms and enhanced patient coaching offer promising solutions to further minimise artefacts. These improvements, combined with the fast acquisition protocol, could strengthen the case for routine use of MRI in screening and follow-up scenarios.
The study population, while diverse in terms of nodule types and sizes, included a predominance of metastatic lesions rather than early-stage primary lung cancers. This limits generalisability to true screening cohorts, where early detection of indolent lesions and ground-glass opacities is more common. Nevertheless, the MRI sequence showed good performance even in these more challenging subtypes, with only one ground-glass nodule missed. Additional validation in screening-specific, multi-centre trials will be essential to establish clinical equivalence.
Radiologist experience also emerged as a variable affecting diagnostic accuracy. None of the participating readers had substantial prior exposure to AI-enhanced pulmonary MRI, which may have influenced the few classification discrepancies observed. Future studies should consider experience stratification or the inclusion of automated assistance in classification tasks to improve diagnostic consistency and reduce subjectivity.
AI-accelerated 3D gradient echo MRI demonstrates strong potential as a radiation-free alternative to CT in lung nodule detection and risk stratification. With high detection rates, strong reader agreement and rapid scan times, the technique meets key requirements for integration into clinical workflows. Its compatibility with standard imaging platforms and reduced dependence on specialised hardware support widespread adoption. To fully establish its role in lung cancer screening, further validation in representative cohorts and multi-centre environments will be essential. Complementary strategies such as radiologist training and AI-driven decision support may further enhance its diagnostic value, making radiation-free lung screening a realistic prospect for future practice.
Source: Academic Radiology
Image Credit: iStock