Pancreatic cancer remains one of the deadliest malignancies, with a five-year survival rate of just 11%. While most cases are sporadic, a notable subset arises in individuals with hereditary or familial predispositions. These high-risk individuals (HRIs) face a significantly elevated lifetime risk of developing pancreatic cancer. Early detection through imaging surveillance is considered crucial, with most programmes employing both magnetic resonance imaging (MRI) and endoscopic ultrasound (EUS). A recent study focused on assessing the effectiveness of an MRI-only surveillance protocol in a Scandinavian cohort of HRIs, examining its diagnostic performance and the incidence of pancreatic malignancy and preneoplastic lesions.
Surveillance Methodology and Findings
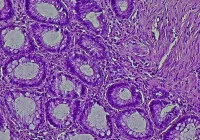
The retrospective study analysed 274 HRIs enrolled between 2002 and 2023. From 2010 onward, MRI became the primary surveillance tool. The median follow-up was 5.8 years. MRI revealed focal pancreatic lesions in 59% of patients, with cysts being the most frequent finding. However, only 5% of individuals required further clinical action. Suspicious cysts were identified in four patients, with three undergoing surgery. None of the resected cysts exhibited high-grade dysplasia or malignancy, pointing to a potential for overtreatment.
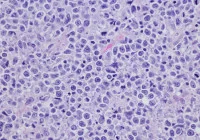
Solid lesions were detected in ten patients. Six were malignant, including three resected pancreatic cancers and three unresectable stage IV tumours. Two of the cancers were interval cases, diagnosed shortly after a prior negative MRI. The resectability rate among cancer patients was 50%, and the incidence of pancreatic cancer across the cohort was low, at 0.32 per 100-person-years. Notably, the rate of early-stage (stage I) and late-stage (stage IV) cancer detection was similar, suggesting limited success in identifying tumours at a surgically curable stage.
Diagnostic Performance and Limitations
The MRI-based protocol demonstrated high specificity (98%) and a strong negative predictive value (99%), indicating that it was reliable in ruling out disease. However, sensitivity was modest (67%), and the positive predictive value was low (44%), highlighting limitations in identifying malignant lesions. The detection of high-grade dysplasia, a key target of surveillance, was absent. Furthermore, interval cancers and missed malignancies suggest that MRI alone may not adequately capture subtle early-stage disease.
The study design, while robust in its longitudinal follow-up, has some constraints. It relied on retrospective analysis and original radiology reports without reassessing imaging data. Additionally, improvements in MRI technology over the two-decade study period may have influenced findings. The study also involved a relatively small number of HRIs with verified genetic mutations, potentially limiting generalisability. Data on metabolic markers such as HbA1c were only recently incorporated into surveillance protocols, restricting insights into their utility for early detection.
Clinical Implications and Future Directions
The findings raise concerns about the sufficiency of MRI as a standalone surveillance tool in HRIs. The absence of high-grade dysplasia, low cancer incidence and limited detection of early-stage disease suggest that current imaging approaches may not meet the expectations of early diagnosis. Although EUS was selectively used in this cohort, its complementary strengths—particularly for solid lesion detection—could enhance surveillance outcomes when used alongside MRI.
Biomarkers may provide additional support. While serum CA 19-9 was routinely monitored, its diagnostic performance is limited. Emerging evidence suggests that glucose metabolism markers such as fasting glucose or HbA1c could assist in identifying individuals at risk of progression, although their value remains inconclusive. The high false positive rate, combined with the low rate of high-risk lesions found, underscores the need for more precise risk stratification and diagnostic criteria to minimise unnecessary interventions.
MRI-based surveillance in HRIs for pancreatic cancer detected a high prevalence of small cystic lesions, but its effectiveness in identifying malignant or preneoplastic changes was limited. The programme demonstrated high specificity but suboptimal sensitivity and positive predictive value. Given the challenges of early detection and the risk of overtreatment, a multimodal approach incorporating MRI, EUS and possibly biomarkers should be considered to optimise surveillance in this vulnerable population.
Source: European Journal of Radiology
Image Credit: iStock