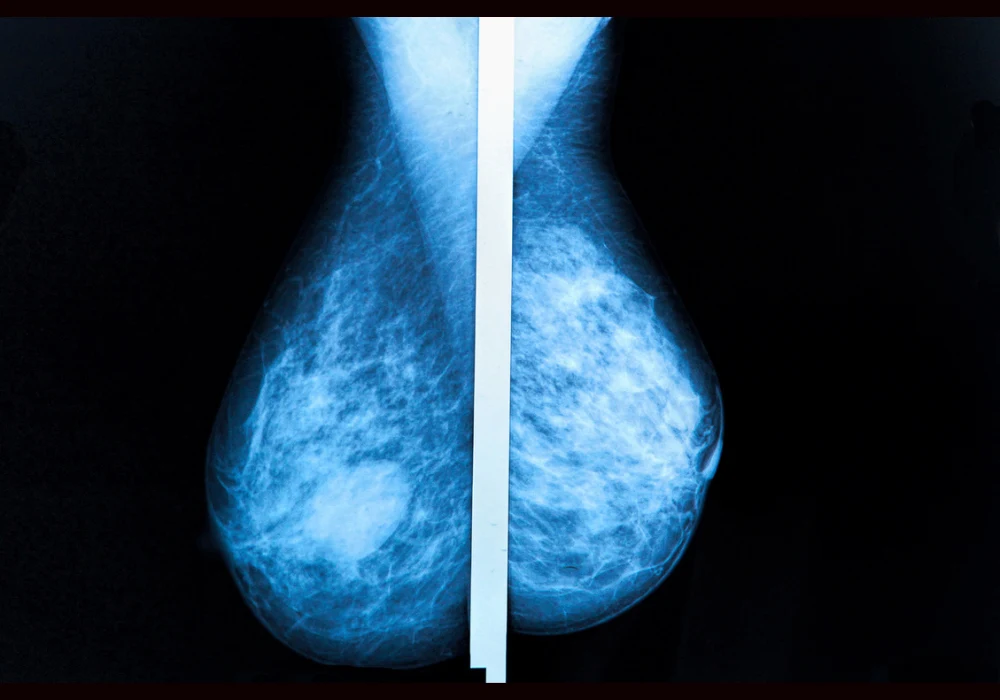
Suspicious microcalcifications are frequently detected in screening mammography, with malignancy rates ranging widely depending on imaging characteristics. The standard approach for further investigation of BI-RADS 4 microcalcifications involves stereotactic-guided vacuum-assisted breast biopsy (VABB), a reliable but invasive and costly procedure. With concerns over patient discomfort, procedural complications and healthcare costs, contrast-enhanced magnetic resonance imaging (CE-MRI) has emerged as a non-invasive alternative. CE-MRI offers the potential to reduce unnecessary biopsies while maintaining diagnostic safety. A cost-effectiveness analysis compared the two strategies to determine whether CE-MRI could viably replace routine biopsy in certain clinical scenarios.
Comparing Diagnostic Strategies
The economic model contrasted two diagnostic pathways for women presenting with BI-RADS 4 microcalcifications: the established route of stereotactic biopsy for all cases, and an alternative approach using CE-MRI to stratify risk before proceeding to biopsy only when MRI findings remained suspicious. In the latter, lesions downgraded to BI-RADS 3 underwent imaging surveillance with mammography at 12 and 24 months.
Using a decision tree and Markov modelling over a 36-month period, the analysis incorporated clinical outcomes such as true positives and false negatives alongside cost data from the US healthcare system. Quality of life metrics were factored into quality-adjusted life years (QALYs), with assumptions including temporary reductions due to biopsy-related anxiety or complications.
Supplemental MRI was found to avoid biopsy in approximately 76–81% of cases, depending on specificity, with a minor false-negative rate of 3.7%. The cumulative cost per woman was slightly higher with MRI in the short term, particularly in the 12-month follow-up model, but overall outcomes were comparable across both strategies. When considering a 24-month follow-up period, CE-MRI resulted in marginally lower cumulative costs and equal or slightly improved QALYs.
Sensitivity Analysis and Cost Drivers
Sensitivity analysis confirmed the robustness of findings across varying assumptions. Key determinants of cost-effectiveness included the price differential between MRI and biopsy, and the specificity of the MRI scan. MRI remained cost-effective as long as its cost remained below 31.1% of the cost of biopsy. Even when MRI specificity was modelled at the lower end of its reported range, incremental cost-effectiveness ratios (ICERs) remained well below accepted thresholds.
Must Read: Detecting Breast Arterial Calcifications with DL
Another important factor was the reduction in quality of life due to unnecessary biopsies. When this factor was excluded from the model, the clinical outcomes between the two strategies became nearly identical, suggesting that much of MRI’s added value may lie in patient-centred benefits rather than improved survival or cancer detection.
The model also assumed high availability and utility of mammographic follow-up in cases where MRI findings did not justify immediate biopsy. This presumes a setting with robust patient compliance and established imaging infrastructure.
Implications and Considerations for Practice
The analysis supports CE-MRI as a viable alternative to immediate stereotactic biopsy for many women with BI-RADS 4 microcalcifications, particularly for lesions classified as BI-RADS 4a and 4b. With a high negative predictive value for invasive cancers and potential to reduce the burden of unnecessary biopsies, CE-MRI offers a patient-friendly approach aligned with modern principles of personalised care and shared decision-making.
Nonetheless, limitations remain. MRI sensitivity is slightly lower for ductal carcinoma in situ (DCIS), which may necessitate cautious selection of candidates. MRI may also reveal incidental findings that require additional imaging or intervention, which could offset savings and affect patient well-being. Furthermore, the findings are based on data from the US Medicare system and may not directly translate to other healthcare settings with different cost structures and reimbursement models.
Clinical pathways incorporating CE-MRI must also address logistical considerations, such as scanner availability and radiologist expertise. Additionally, the role of MRI-guided biopsy for MRI-only lesions must be clarified, though current practice suggests that most such findings can be managed with ultrasound-guided techniques.
Contrast-enhanced MRI offers a non-invasive, cost-effective alternative to stereotactic biopsy for many women with BI-RADS 4 microcalcifications. By enabling risk stratification without immediate tissue sampling, MRI can reduce procedural harms and healthcare costs while preserving diagnostic safety. These findings reinforce the need for shared decision-making and suggest that CE-MRI could be integrated into diagnostic workflows, particularly where patient compliance and imaging follow-up are reliable. Broader implementation will depend on healthcare infrastructure and evolving clinical guidelines.
Source: Insights into Imaging
Image Credit: iStock