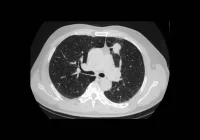
Technological advances in computed tomography (CT) have significantly improved diagnostic capabilities, enabling faster, higher-quality imaging across a wide range of clinical scenarios. However, a concerning trend has emerged over the past decade: a sharp increase in single CT examinations with effective doses of 50 millisieverts (mSv) or more. Although these cases remain a small percentage of overall CT volume, their rise is substantial and primarily associated with larger patients, multiphase imaging and the use of advanced scanners. This pattern raises important questions about imaging practice, scanner capabilities and the balance between diagnostic benefit and radiation risk.
The Role of Patient Size and Imaging Complexity
Between 2013 and 2022, 1.35 million CT scans were conducted in a major U.S. academic centre, with just under 0.5% involving doses of 50 mSv or more. While small in proportion, the number of these high-dose exams grew by 244% between 2017 and 2022. Among cases where body mass index (BMI) data was available, nearly 80% of high-dose scans involved overweight or obese patients. For this group, the annual number of high-dose exams increased by 250 each year from 2018 to 2022, compared with just 39 additional exams per year among patients with underweight or normal BMI.
Internal link: Refining CT Image Quality Assessment
The increase in radiation exposure is largely driven by the need to maintain diagnostic image quality in patients with higher body mass, who require greater X-ray output to achieve comparable clarity. Multiphase imaging, which involves multiple sequential scans during different phases of contrast enhancement, adds further dose burden. CT angiography of the aorta and coronary arteries were the most common protocols associated with these elevated doses, alongside evaluations for oncological and vascular conditions.
Technology, Protocols and Scanner Variability
The introduction of newer CT scanners equipped with powerful X-ray tubes and larger gantry diameters has enabled imaging of larger patients and more complex diagnostic assessments. However, these machines, while technologically advanced, carry the potential for excessive radiation delivery if not properly calibrated. In the institution studied, the majority of high-dose exams were performed using scanners from a single vendor, with notable differences in dose levels observed across equipment from different manufacturers, even when controlling for patient size and protocol.
Increased dose levels were particularly associated with diagnostic exams involving three or more phases, which represented nearly 60% of high-dose cases. Between 2013 and 2018, these exams were relatively rare, but since 2019 they have become the dominant contributor to the rise in dose. Interventional CT procedures, such as guided biopsies, also contributed, but to a lesser extent. While these procedures made up only 2% of all CT scans, they accounted for over a quarter of high-dose exams with BMI data.
These patterns suggest that scanner design, protocol settings and clinical workflow choices all play a role in determining radiation exposure. Suboptimal protocol selection, automatic tube current modulation systems not tailored to patient size, and the adoption of multiphase protocols without sufficient dose oversight can contribute to unnecessarily high doses.
Implications for Practice and Future Directions
The findings illustrate the need for comprehensive radiation dose management strategies, particularly in the context of rising obesity rates and expanding CT capabilities. The presence of more powerful scanners must be matched with rigorous protocol optimisation, including limiting scan ranges, reducing the number of phases and leveraging dose-saving technologies such as iterative reconstruction and virtual non-contrast imaging. Vendor-provided tools to cap tube current and institutional policies promoting patient-specific protocol selection are essential to mitigate risk.
Despite the challenges, modern scanners have enabled imaging for patients who were previously difficult or impossible to assess using older systems. Increased gantry sizes and table capacities have improved accessibility for bariatric patients and image quality in this population has markedly improved. However, the increase in radiation dose demands further scrutiny, particularly in relation to whether higher doses lead to meaningful clinical benefit or simply enhance image clarity without diagnostic gain.
Further research is needed to evaluate the diagnostic justification for high-dose scans and to compare outcomes with lower-dose alternatives. Advances in artificial intelligence may offer the potential for real-time, patient-specific dose estimation, improving personalisation and oversight. In the absence of standardised reference values for multiphase exams, the use of effective dose remains a practical metric, although it has known limitations.
The rising use of high-dose CT examinations reflects both the strengths and the risks of modern imaging technology. While improvements in scanner design have broadened access and diagnostic capability, particularly for larger patients and complex cases, they also necessitate increased vigilance in radiation management. Ensuring patient safety requires coordinated efforts in protocol development, scanner optimisation and the adoption of personalised imaging strategies. In the future, maintaining a balance between image quality and dose safety will be critical to preserving both diagnostic integrity and long-term patient well-being.
Source: British Journal of Radiology
Image Credit: iStock